Aetna to Waive Cost-sharing Charges for Hospital Admissions for Covid-19 Treatment
March 25 2020 - 11:25AM
Dow Jones News
By Anna Wilde Mathews
CVS Health Corp. said its Aetna unit will waive cost-sharing
charges for people who are admitted to the hospital for treatment
of Covid-19, the respiratory illness tied to the new
coronavirus.
The big insurer's move, which will apply in its employer plans,
goes beyond a recently-passed law that forces insurers to cover
coronavirus testing without out-of-pocket cost to members. That law
included visits to a doctor or emergency room that result in a
test, but didn't include treatment for those sick with
Covid-19.
An Aetna spokesman said the insurer believes it is the first to
waive cost-sharing on Covid-19 hospital stays on a national basis.
He said the new policy applies to fully-insured employer plans and
also for self-insured employers, though they can opt out.
Aetna will waive co-payments and co-insurance, and the hospital
stays will be covered without out-of-pocket charges even before the
patient's deductible is maxed out. The new policy applies to
inpatient admissions at in-network hospitals for treatment of
Covid-19 or complications from it. The policy applies from now
through June 1.
Hospital treatment for Covid-19 can be costly. The Kaiser Family
Foundation estimated that in employer plans, the total cost of a
hospital admission for pneumonia with major complications was more
than $20,000 on average, and the average out-of-pocket cost for the
patient was about $1,300.
(END) Dow Jones Newswires
March 25, 2020 11:10 ET (15:10 GMT)
Copyright (c) 2020 Dow Jones & Company, Inc.
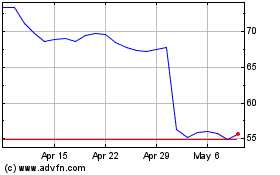
CVS Health (NYSE:CVS)
Historical Stock Chart
From Aug 2024 to Sep 2024
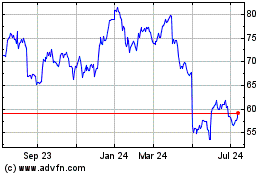
CVS Health (NYSE:CVS)
Historical Stock Chart
From Sep 2023 to Sep 2024