Based on ECHO Phase III trial results which
showed more than 16 months of progression-free survival improvement
vs. chemoimmunotherapy alone
First and only BTK inhibitor approved for
the 1st-line treatment of MCL in the US
AstraZeneca’s CALQUENCE® (acalabrutinib) in combination with
bendamustine and rituximab has been approved in the US for the
treatment of adult patients with previously untreated mantle cell
lymphoma (MCL) who are ineligible for autologous hematopoietic stem
cell transplantation.
The approval was granted by the Food and Drug Administration
(FDA) after securing Priority Review. It was based on results from
the ECHO Phase III trial which were presented at the European
Hematology Association 2024 Congress.
MCL is a rare and typically aggressive form of non-Hodgkin
lymphoma (NHL), often diagnosed at an advanced stage.1,2 It is
estimated that there are more than 21,000 patients diagnosed with
MCL in the US, UK, France, Germany, Spain, Italy, Japan and
China.3
Michael Wang, MD, Puddin Clarke Endowed Professor, Director of
Mantle Cell Lymphoma Program of Excellence and principal
investigator in the trial, said: “Managing this aggressive cancer
requires maximizing efficacy while maintaining tolerability,
especially for elderly patients. Results from the pivotal ECHO
trial highlight the promise of the acalabrutinib combination in
defining a new standard of care, with today’s approval underscoring
the transformative potential of this regimen as a first-line
treatment for older patients with mantle cell lymphoma.”
Dave Fredrickson, Executive Vice President, Oncology Business
Unit, AstraZeneca, said: “With today’s approval, CALQUENCE provides
a critical new treatment option to mantle cell lymphoma patients in
the US, with CALQUENCE proven to deliver nearly one and a half
years of additional time without disease progression. This approval
brings a new and effective treatment option to those living with
this disease and further reinforces our belief in CALQUENCE as a
backbone therapy across multiple blood cancers.”
Meghan Gutierrez, Chief Executive Officer, Lymphoma Research
Foundation, said: “New treatment options have long been needed in
the first-line treatment of mantle cell lymphoma in the US.
Patients with this rare and often aggressive cancer can experience
severe symptoms by the time they are diagnosed - having an
effective therapy that can significantly improve outcomes for
patients early in the treatment process is a much-needed
advancement.”
Results from the ECHO trial showed CALQUENCE plus bendamustine
and rituximab reduced the risk of disease progression or death by
27% compared to standard-of-care chemoimmunotherapy (hazard ratio
[HR] 0.73; 95% confidence interval [CI] 0.57-0.94; p=0.016). Median
PFS was 66.4 months for patients treated with the CALQUENCE
combination versus 49.6 months with chemoimmunotherapy alone.
This approval additionally converts CALQUENCE’s accelerated
approval to a full approval for adult patients with MCL treated
with at least one prior therapy, as granted by the FDA in October
2017.
The ECHO trial enrolled patients throughout the COVID-19
pandemic. After censoring for COVID-19 deaths, PFS was further
improved in both arms, with the CALQUENCE combination reducing the
risk of disease progression or death by 36% (HR 0.64; 95% CI
0.48-0.84). Although OS data were not mature at the time of the
analysis, when censored for COVID-19, a favorable trend was seen
for OS (HR 0.75; 95% CI 0.53-1.04), despite 69% of patients in the
chemoimmunotherapy arm receiving treatment with a BTK inhibitor on
relapse or disease progression.
The safety and tolerability of CALQUENCE was consistent with its
known safety profile, and no new safety signals were
identified.
The US regulatory submission was reviewed under Project Orbis,
which provides a framework for concurrent submission and review of
oncology medicines among participating international partners. As
part of Project Orbis, CALQUENCE plus chemoimmunotherapy is also
under review by regulatory authorities in Australia, Canada, and
Switzerland for the same indication. Regulatory applications are
also under review in the EU, Japan, and other countries based on
the ECHO results.
INDICATIONS AND USAGE
CALQUENCE is a Bruton tyrosine kinase (BTK) inhibitor indicated
in combination with bendamustine and rituximab (BR) for the
treatment of adult patients with previously untreated mantle cell
lymphoma (MCL) who are ineligible for autologous hematopoietic stem
cell transplantation (HSCT), as monotherapy for the treatment of
adult patients with MCL who have received at least one prior
therapy, and for the treatment of adult patients with chronic
lymphocytic leukemia (CLL) or small lymphocytic lymphoma (SLL).
IMPORTANT SAFETY INFORMATION ABOUT CALQUENCE® (acalabrutinib)
tablets
Serious and Opportunistic Infections Fatal and serious
infections, including opportunistic infections, have occurred in
patients with hematologic malignancies treated with CALQUENCE.
Serious or Grade 3 or higher infections (bacterial, viral, or
fungal) occurred in 32% of 1,764 patients exposed to CALQUENCE in
clinical trials, most often due to respiratory tract infections
(19% of all patients, including pneumonia in 9%). These infections
predominantly occurred in the absence of Grade 3 or 4 neutropenia,
with neutropenic infection reported in 2.7% of all patients.
Opportunistic infections in recipients of CALQUENCE have included,
but are not limited to, hepatitis B virus reactivation, fungal
pneumonia, Pneumocystis jirovecii pneumonia, Epstein-Barr virus
reactivation, cytomegalovirus, and progressive multifocal
leukoencephalopathy (PML). Consider prophylaxis in patients who are
at increased risk for opportunistic infections. Monitor patients
for signs and symptoms of infection and treat promptly.
Hemorrhage Fatal and serious hemorrhagic events have
occurred in patients treated with CALQUENCE. Major hemorrhage
(serious or Grade 3 or higher bleeding or any central nervous
system bleeding) occurred in 4.4% of patients, with fatal
hemorrhage occurring in 0.2% of 1,764 patients exposed to CALQUENCE
in clinical trials. Bleeding events of any grade, excluding
bruising and petechiae, occurred in 40% of patients.
Use of antithrombotic agents concomitantly with CALQUENCE may
further increase the risk of hemorrhage. In clinical trials, major
hemorrhage occurred in 7% of patients taking CALQUENCE without
antithrombotic agents and 4% of patients taking CALQUENCE with
antithrombotic agents. Consider the risks and benefits of
antithrombotic agents when co-administered with CALQUENCE. Monitor
patients for signs of bleeding.
Consider the benefit-risk of withholding CALQUENCE for 3 to 7
days pre- and post-surgery depending upon the type of surgery and
the risk of bleeding.
Cytopenias CALQUENCE can cause Grade 3 or 4 cytopenias.
Grade 3 or 4 cytopenias included absolute neutrophil count
decreased (26%), platelets decreased (10%), hemoglobin decreased
(10%), and absolute lymphocyte count decreased (10%) in patients
treated with CALQUENCE alone or in combination with obinutuzumab;
Grade 4 neutropenia developed in 14% of patients.
Monitor complete blood counts regularly during treatment.
Interrupt treatment, reduce the dose, or discontinue treatment as
warranted.
Second Primary Malignancies Second primary malignancies,
including skin cancers and other solid tumors, occurred in 18% of
1,764 patients exposed to CALQUENCE in clinical trials. The most
frequent second primary malignancy was non-melanoma skin cancer,
reported in 10% of patients, followed by other solid tumors in 9%
(including melanoma, lung cancer, gastrointestinal cancers, and
genitourinary cancers) and hematologic malignancies (1%). Monitor
patients for the development of second cancers and advise
protection from sun exposure.
Cardiac Arrhythmias Fatal and serious cardiac arrhythmias
have occurred in patients treated with CALQUENCE. Grade 3 or 4
atrial fibrillation or flutter was reported in 2.6% of 1,764
patients treated with CALQUENCE, with all grades of atrial
fibrillation or flutter reported in 7% of all patients. Grade 3 or
higher ventricular arrhythmia events were reported in 0.6% of
patients, including fatal cases in 0.3% of all patients. The risk
of arrhythmias may be increased in patients with cardiac risk
factors, hypertension, previous arrhythmias, and acute infection.
Monitor for symptoms of arrhythmia (eg, palpitations, dizziness,
syncope, dyspnea) and manage as appropriate.
Hepatotoxicity, Including Drug-Induced Liver Injury
Hepatotoxicity, including severe, life-threatening, and potentially
fatal cases of drug-induced liver injury (DILI), has occurred in
patients treated with Bruton tyrosine kinase inhibitors, including
CALQUENCE.
Evaluate bilirubin and transaminases at baseline and throughout
treatment with CALQUENCE. For patients who develop abnormal liver
tests after CALQUENCE, monitor more frequently for liver test
abnormalities and clinical signs and symptoms of hepatic toxicity.
If DILI is suspected, withhold CALQUENCE. Upon confirmation of
DILI, discontinue CALQUENCE.
ADVERSE REACTIONS
Previously Untreated Mantle Cell
Lymphoma The most common adverse reactions (≥15%) of any
grade in patients with previously untreated MCL who received
CALQUENCE plus BR were rash (47%), COVID-19 (38%), fatigue (37%),
diarrhea (37%), pneumonia (31%), headache (31%), upper respiratory
tract infection (30%), pyrexia (29%), cough (27%), vomiting (26%),
constipation (25%), hemorrhage (20%), edema (20%), secondary
primary malignancy (19%), dizziness (18%), arthralgia (18%), and
dyspnea (17%).
Grade 4 laboratory abnormalities in >15% of patients treated
with CALQUENCE plus BR include lymphocytes decreased (26%),
absolute neutrophils decreased (36%), and uric acid increased
(17%).
Serious adverse reactions occurred in 69% of patients who
received CALQUENCE plus BR. Serious adverse reactions reported in
≥2% of patients were pneumonia (23%; includes COVID-19 pneumonia),
COVID-19 (20%; includes COVID-19 pneumonia), second primary
malignancy (7%), pyrexia (6%), rash (3.4%), febrile neutropenia
(3.4%), atrial fibrillation (3%), sepsis (2.7%), and anemia (2.4%).
Fatal adverse reactions that occurred within 30 days of the last
study treatment were reported in 12% who received CALQUENCE plus BR
including COVID-19 (6%; includes COVID-19 pneumonia), pneumonia
(1%), second primary malignancy (0.7%), sepsis (0.3%), and
pneumonitis (0.3%).
Adverse reactions led to permanent discontinuation of CALQUENCE
in 43%, dosage interruptions in 74%, and dosage reductions in 10%
of patients. Adverse reactions that resulted in dosage modification
in >10% included infections, cytopenias, rashes, and
gastrointestinal toxicity. Adverse reactions which resulted in
permanent discontinuation of CALQUENCE in ≥4% of patients included
COVID-19 (includes COVID-19 pneumonia) and neutropenia.
Previously Treated Mantle Cell
Lymphoma The most common adverse reactions (≥20%) of any
grade in patients with relapsed or refractory MCL exposed to
CALQUENCE were anemia,* thrombocytopenia,* headache (39%),
neutropenia,* diarrhea (31%), fatigue (28%), myalgia (21%), and
bruising (21%). The most common Grade ≥3 non-hematological adverse
reaction (reported in at least 2% of patients) was diarrhea
(3.2%).
*Treatment-emergent decreases (all grades) of hemoglobin (46%),
platelets (44%), and neutrophils (36%) were based on laboratory
measurements and adverse reactions.
Dose reductions or discontinuations due to any adverse reaction
were reported in 1.6% and 6.5% of patients, respectively. Increases
in creatinine to 1.5 to 3 times the upper limit of normal (ULN)
occurred in 4.8% of patients.
Chronic Lymphocytic Leukemia The
most common adverse reactions (≥30%) of any grade in patients with
CLL exposed to CALQUENCE were anemia,* neutropenia,*
thrombocytopenia,* headache, upper respiratory tract infection, and
diarrhea.
*Treatment-emergent decreases (all grades) of hemoglobin,
platelets, and neutrophils were based on laboratory measurements
and adverse reactions.
In patients with previously untreated CLL exposed to CALQUENCE,
fatal adverse reactions that occurred in the absence of disease
progression and with onset within 30 days of the last study
treatment were reported in 2% for each treatment arm, most often
from infection. Serious adverse reactions were reported in 39% of
patients in the CALQUENCE plus obinutuzumab arm and 32% in the
CALQUENCE monotherapy arm, most often due to events of pneumonia
(2.8% to 7%).
Adverse reactions led to CALQUENCE dose reduction in 7% and 4%
of patients in the CALQUENCE plus obinutuzumab arm (N=178) and
CALQUENCE monotherapy arm (N=179), respectively. Adverse events led
to discontinuation in 11% and 10% of patients, respectively.
Increases in creatinine to 1.5 to 3 times ULN occurred in 3.9% and
2.8% of patients in the CALQUENCE combination arm and monotherapy
arm, respectively.
In patients with relapsed/refractory CLL exposed to CALQUENCE,
serious adverse reactions occurred in 29% of patients. Serious
adverse reactions in >5% of patients who received CALQUENCE
included lower respiratory tract infection (6%). Fatal adverse
reactions within 30 days of the last dose of CALQUENCE occurred in
2.6% of patients, including from second primary malignancies and
infection.
Adverse reactions led to CALQUENCE dose reduction in 3.9% of
patients (N=154), dose interruptions in 34% of patients, most often
due to respiratory tract infections followed by neutropenia, and
discontinuation in 10% of patients, most frequently due to second
primary malignancies followed by infection. Increases in creatinine
to 1.5 to 3 times ULN occurred in 1.3% of patients who received
CALQUENCE.
DRUG INTERACTIONS
Strong CYP3A Inhibitors: Avoid co-administration of
CALQUENCE with a strong CYP3A inhibitor. If these inhibitors will
be used short-term, interrupt CALQUENCE. After discontinuation of
strong CYP3A inhibitor for at least 24 hours, resume previous
dosage of CALQUENCE.
Moderate CYP3A Inhibitors: Reduce the dosage of CALQUENCE
to 100 mg once daily when co-administered with a moderate CYP3A
inhibitor.
Strong CYP3A Inducers: Avoid co-administration of
CALQUENCE with a strong CYP3A inducer. If co-administration is
unavoidable, increase the dosage of CALQUENCE to 200 mg
approximately every 12 hours.
SPECIFIC POPULATIONS
Based on findings in animals, CALQUENCE may cause fetal harm and
dystocia when administered to a pregnant woman. There are no
available data in pregnant women to inform the drug-associated
risk. Advise pregnant women of the potential risk to a fetus.
Pregnancy testing is recommended for females of reproductive
potential prior to initiating CALQUENCE therapy. Advise female
patients of reproductive potential to use effective contraception
during treatment with CALQUENCE and for 1 week following the last
dose of CALQUENCE.
It is not known if CALQUENCE is present in human milk. Advise
lactating women not to breastfeed while taking CALQUENCE and for 2
weeks after the last dose.
Avoid use of CALQUENCE in patients with severe hepatic
impairment (Child-Pugh class C). No dosage adjustment of CALQUENCE
is recommended in patients with mild (Child-Pugh class A) or
moderate (Child-Pugh class B) hepatic impairment.
Please see full Prescribing Information,
including Patient Information.
Notes
Mantle cell lymphoma While MCL patients initially respond
to treatment, patients do tend to relapse.4 MCL comprises about
3-6% of non-Hodgkin lymphomas, with an annual incidence of 0.5 per
100,000 population in Western countries; in the US, it is estimated
that approximately 4,000 new patients are diagnosed with MCL each
year.4,5
ECHO ECHO is a randomized, double-blind,
placebo-controlled, multi-center Phase III trial evaluating the
efficacy and safety of CALQUENCE plus bendamustine and rituximab
compared to SoC chemoimmunotherapy (bendamustine and rituximab) in
adult patients at or over 65 years of age (n=635) with previously
untreated MCL.6 Patients were randomized 1:1 to receive either
CALQUENCE or placebo administered orally twice per day,
continuously, until disease progression or unacceptable toxicity.
Additionally, all patients received six 28-day cycles of
bendamustine on days 1 and 2 and rituximab on day 1 of each cycle,
followed by rituximab maintenance for two years if patients
achieved a response after induction therapy.6
The primary endpoint is PFS assessed by an Independent Review
Committee; other efficacy endpoints include OS, overall response
rate (ORR), duration of response (DoR) and time to response (TTR).6
The trial was conducted in 27 countries across North and South
America, Europe, Asia and Oceania.6
The ECHO trial enrolled patients from May 2017 to March 2023,
continuing through the COVID-19 pandemic. Prespecified PFS and OS
analyzes censoring for COVID-19 deaths were conducted to assess the
impact of COVID-19 on the study outcome in alignment with the FDA.
Patients with blood cancer remain at a disproportionately high risk
of severe outcomes from COVID-19, including hospitalization and
death compared to the general population.6,7
CALQUENCE CALQUENCE (acalabrutinib) is a
second-generation, selective inhibitor of Bruton’s tyrosine kinase
(BTK). CALQUENCE binds covalently to BTK, thereby inhibiting its
activity.8 In B-cells, BTK signaling results in activation of
pathways necessary for B-cell proliferation, trafficking,
chemotaxis and adhesion.
CALQUENCE has been used to treat more than 85,000 patients
worldwide9 and is approved for the treatment of chronic lymphocytic
leukemia (CLL) and small lymphocytic lymphoma (SLL) in the US and
Japan, approved for CLL in the EU and many other countries
worldwide and approved in China for relapsed or refractory CLL and
SLL. CALQUENCE is also approved for the treatment of adult patients
with previously untreated MCL in the US, and in China and several
other countries for the treatment of adult patients with mantle
cell lymphoma (MCL) who have received at least one prior therapy.
CALQUENCE is not currently approved for the treatment of MCL in
Japan or the EU.
As part of an extensive clinical development program, CALQUENCE
is currently being evaluated as a single treatment and in
combination with standard-of-care chemoimmunotherapy for patients
with multiple B-cell blood cancers, including CLL, MCL and diffuse
large B-cell lymphoma.
AstraZeneca in hematology AstraZeneca is pushing the
boundaries of science to redefine care in hematology. Our goal is
to help transform the lives of patients living with malignant, rare
and other related hematologic diseases through innovative medicines
and approaches that are shaped by insights from patients,
caregivers and physicians.
In addition to our marketed products, we are spearheading the
development of novel therapies designed to target underlying
drivers of disease across multiple scientific platforms. Our
acquisitions of Alexion, with expertise in rare, non-malignant
blood disorders, and Gracell Biotechnologies Inc., pioneers of
autologous cell therapies, expand our hematology pipeline and
enable us to reach more patients with high unmet needs through the
end-to-end discovery, development and delivery of novel
therapies.
AstraZeneca in oncology AstraZeneca is leading a
revolution in oncology with the ambition to provide cures for
cancer in every form, following the science to understand cancer
and all its complexities to discover, develop and deliver
life-changing medicines to patients.
The Company's focus is on some of the most challenging cancers.
It is through persistent innovation that AstraZeneca has built one
of the most diverse portfolios and pipelines in the industry, with
the potential to catalyze changes in the practice of medicine and
transform the patient experience.
AstraZeneca has the vision to redefine cancer care and, one day,
eliminate cancer as a cause of death.
AstraZeneca
AstraZeneca is a global, science-led biopharmaceutical company
that focuses on the discovery, development, and commercialization
of prescription medicines in Oncology, Rare Diseases, and
BioPharmaceuticals, including Cardiovascular, Renal &
Metabolism, and Respiratory & Immunology. Based in Cambridge,
UK, AstraZeneca operates in over 125 countries, and its innovative
medicines are used by millions of patients worldwide. For more
information, please visit astrazeneca-us.com and follow us on
social media @AstraZeneca.
References
- Lymphoma Research Foundation. Mantle Cell Lymphoma. Accessed
January 2025. https://lymphoma.org/aboutlymphoma/nhl/mcl/
- National Organization for Rare Disorders. Mantle Cell Lymphoma.
Accessed January 2025. Available at:
https://rarediseases.org/rare-diseases/mantle-cell-lymphoma/
- AstraZeneca 2024. Q3 2024 Financial Results. Accessed January
2025. https://www.astrazeneca.com/investor-relations.html
- Cheah C, Seymour J, Wang ML. Mantle cell lymphoma. J Clin
Oncol. 2016;34(11):1256-1269. doi: 10.1200/JCO.2015.63.5904.
- MD Anderson Cancer Center. What to know about mantle cell
lymphoma. Accessed January 2025.
https://www.mdanderson.org/cancerwise/what-to-know-about-mantle-cell-lymphoma-symptoms-diagnosis-and-treatment.h00-159385101.html
- ClinicalTrials.gov. A Study of BR Alone Versus in Combination
With Acalabrutinib in Subjects With Previously Untreated MCL.
Accessed January 2025.
https://clinicaltrials.gov/study/NCT02972840
- Dube S, et al. Continued Increased Risk of COVID-19
Hospitalization and Death in Immunocompromised Individuals Despite
Receipt of ≥4 Vaccine Doses: Updated 2023 Results from INFORM, a
Retrospective Health Database Study in England. Poster P0409 at
ECCMID 2024.
- Wu J, Zhang M, Liu D. Acalabrutinib (ACP-196): a selective
second-generation BTK inhibitor. J Hematol Oncol. 2016;9(21).
- Data on File, REF-236261. AstraZeneca Pharmaceuticals LP.
US-48947 Last Updated 1/25
View source
version on businesswire.com: https://www.businesswire.com/news/home/20250117223765/en/
Media Inquiries Fiona Cookson +1 212 814 3923 US Media
Mailbox: usmediateam@astrazeneca.com
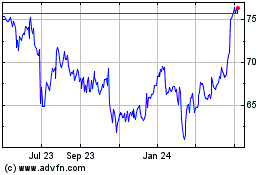
AstraZeneca (NASDAQ:AZN)
Historical Stock Chart
From Dec 2024 to Jan 2025
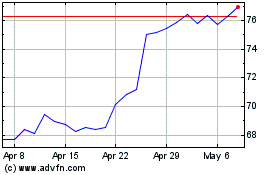
AstraZeneca (NASDAQ:AZN)
Historical Stock Chart
From Jan 2024 to Jan 2025