UNITED STATES
SECURITIES AND EXCHANGE COMMISSION
Washington, D.C. 20549
FORM 6-K
REPORT OF FOREIGN
PRIVATE ISSUER PURSUANT TO RULE 13a-16 OR 15d-16 UNDER THE SECURITIES EXCHANGE ACT OF 1934
November 8, 2023
Commission File Number: 001-39363
IMMATICS N.V.
Paul-Ehrlich-Straße 15
72076 Tübingen, Federal Republic of Germany
(Address of principal executive office)
Indicate by check mark whether the registrant files
or will file annual reports under cover of Form 20-F or Form 40-F:
INFORMATION CONTAINED IN THIS REPORT ON FORM
6-K
On November 8, 2023, Immatics N.V. (the “Company” or “Immatics”)
provided interim data from its ongoing Phase 1 trial with ACTengine® IMA203 GEN1, with a focus on IMA203 GEN1 in melanoma
at the recently defined recommended Phase 2 dose (“RP2D”), and IMA203CD8 GEN2 TCR-T both as monotherapy in patients with recurrent
and/or refractory solid cancers. The data cutoff was September 30, 2023.
IMA203 GEN1 in Melanoma Patients Treated as RP2D
| · | 16 PRAME-positive patients with cutaneous, uveal or melanoma of unknown primary origin were infused
with IMA203 GEN1 at the RP2D (1-10x109 total TCR-T cells) across Phase 1a or Phase 1b Cohort A. |
| o | All 16 patients experienced expected cytopenia (Grade 1-4) associated with lymphodepletion as expected. Patients had mostly mild-moderate
cytokine release syndrome (“CRS”), of which 10 patients (63%) had Grade 1 CRS, and 5 patients (31%) had Grade 2 CRS, and 1
patient (6%) had Grade 3 CRS. |
| o | One non-serious, mild (Grade 1) immune effector cell associated neurotoxicity syndrome (“ICANS”) was observed. |
| o | No dose-dependent increase of CRS, no dose-limiting toxicity, and no IMA203-related death was observed. |
| o | The most common Grade ≥3 treatment-emergent adverse events (“TEAEs”) observed across all dose levels (N=49) and at
the RP2D (N=28) for all patients are set forth in the tables below: |

All treatment-emergent adverse events (TEAEs) with ≥
Grade 3 regardless of relatedness to study treatment that occurred in at least 1 patient (except for ICANS, where only Grade 1-2 occurred;
listed for completeness due to being an adverse event of special interest) are presented. Adverse events were coded using the Medical
Dictionary for Regulatory Activities. Grades were determined according to National Cancer Institute Common Terminology Criteria of Adverse
Events, version 5.0. Grades for CRS and ICANS were determined according to CARTOX criteria (Neelapu et al., 2018). Patients
are counted only once per adverse event and severity classification. Based on interim data extracted from open clinical database (30-Sep-2023);
1 Two patients with disease progression after first IMA203 infusion received exploratory second IMA203 infusion. They had these
≥ Grade 3 TEAEs only after second infusion, which are included in the table: First patient: Abdominal pain, Cytokine release syndrome,
Diarrhoea, Hypokalaemia, Proteinuria; Second patient: Humerus fracture, Muscle spasms, Neutropenia, Thrombocytopenia; 2
ICANS: Immune effector cell-associated neurotoxicity syndrome; 3 DLT: Dose limiting toxicity in phase 1a at DL2 reported
on March 17, 2021; 4 Fatal Adverse events were not considered related to any study drug; 5 Patient died from sepsis
of unknown origin and did not receive IMA203 TCR-T cells.

All treatment-emergent adverse events (TEAEs) with ≥
Grade 3 regardless of relatedness to study treatment that occurred in at least 1 patient (except for ICANS, where only Grade 1-2 occurred;
listed for completeness due to being an adverse event of special interest) are presented. Adverse events were coded using the Medical
Dictionary for Regulatory Activities. Grades were determined according to National Cancer Institute Common Terminology Criteria of Adverse
Events, version 5.0. Grades for CRS and ICANS were determined according to CARTOX criteria (Neelapu et al., 2018). Patients
are counted only once per adverse event and severity classification. Based on interim data extracted from open clinical database (30-Sep-2023);
1 One patient in Phase 1a DL4 with disease progression after first IMA203 infusion received exploratory second IMA203 infusion
and had these ≥ Grade 3 TEAEs only after second infusion, which are included in the table: Humerus fracture, Muscle spasms, Neutropenia,
Thrombocytopenia; 2 ICANS: Immune effector cell-associated neurotoxicity syndrome; 3 Fatal Adverse events were
not considered related to any study drug
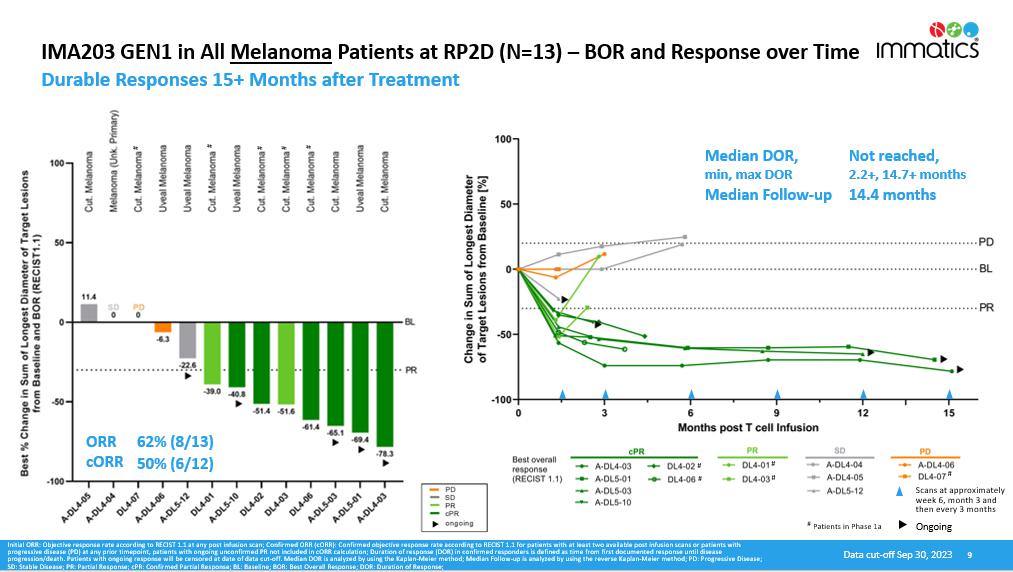
| o | 13 out of 16 melanoma
patients infused at RP2D were evaluable for efficacy analysis based on at least one tumor response assessment being available
post treatment. These patients received a median total infused dose of 1.73x109 IMA203 TCR-T cells (range 1.07-5.12x109
TCR-T cells). |
| o | Most patients were heavily pre-treated with a median of 4 lines of systemic therapies, thereof a median of 2 lines of checkpoint inhibitors.
All 8 cutaneous melanoma patients were checkpoint inhibitor-refractory and 5 of 8 cutaneous melanoma patients were BRAF inhibitor-pretreated. |
| o | 50% (6/12) cORR and 62% (8/13) initial objective response rate (“ORR”) (according to RECIST 1.1). |
| o | Durability of responses ongoing beyond 12 months in one patient and 15 months in two patients after treatment. |
| o | Median duration of response (“mDOR”) was not reached (min. 2.2+ months, max. 14.7+ months) at a median follow-up (“mFU”)
of 14.4 months. |
| o | The best overall response and response over time for melanoma patients in Phase 1a and Phase 1b Cohort A at the RP2D are set forth
in the charts below: |

Initial ORR: Objective response rate according to RECIST
1.1 at any post infusion scan; Confirmed ORR (cORR): Confirmed objective response rate according to RECIST 1.1 for patients with at least
two available post infusion scans or patients with progressive disease (PD) at any prior timepoint, patients with ongoing unconfirmed
PR not included in cORR calculation; Duration of response (DOR) in confirmed responders is defined as time from first documented response
until disease progression/death. Patients with ongoing response will be censored at date of data cut-off. Median DOR is analyzed by using
the Kaplan-Meier method; Median Follow-up is analyzed by using the reverse Kaplan-Meier method; PD: Progressive Disease; SD: Stable Disease;
PR: Partial Response; cPR: Confirmed Partial Response; BL: Baseline; BOR: Best Overall Response; DOR: Duration of Response.
IMA203CD8 GEN2
| · | 12 PRAME-positive patients were infused with IMA203CD8 GEN2 across DL3 (0.2-0.48x109 TCR-T
cells/m2 BSA), DL4a (0.481-0.8x109 TCR-T cells/m2 BSA) and DL4b (0.801-1.2x109 TCR-T cells/m2)
in Cohort C with a median total infused dose of 1.17x109 IMA203CD8 TCR-T cells (range 0.64-2.05x109 TCR-T cells). |
| · | All patients were heavily pre-treated with a median of 3 lines of systemic therapies. |
| o | All patients experienced cytopenia (Grade 1-4) associated with lymphodepletion as expected. 11 out of 12 patients (92%) experienced
a CRS, of which 8 patients (67%) had Grade 1 or 2 CRS, 2 patients (17%) had Grade 3 CRS, and 1 patient (8%) had a Grade 4 CRS. The latter
patient also had a reported Grade 4 neurotoxicity. |
| o | No ICANS or neurotoxicity was reported for the other patients. |
| o | No IMA203CD8-related deaths were observed. |
| o | DLTs were reported for 2 of 4 patients treated at DL4b. No DLT was reported for 4 patients treated at DL3 or 4 patients treated at
DL4a. The DL4a dose cohort is ongoing. |
| o | The most common Grade ≥3 TEAEs observed are set forth in the table below: |

All treatment-emergent adverse events (TEAEs) with ≥
Grade 3 regardless of relatedness to study treatment that occurred in at least 1 patient (except for ICANS, where no event was documented;
listed for completeness due to being an adverse event of special interest) are presented. Adverse events were coded using the Medical
Dictionary for Regulatory Activities. Grades were determined according to National Cancer Institute Common Terminology Criteria of Adverse
Events, version 5.0. Grades for CRS and ICANS were determined according to CARTOX criteria (Neelapu et al., 2018). Patients
are counted only once per adverse event and severity classification. Based on interim data extracted from open clinical database (30-Sep-2023);
1 DLT: Dose limiting toxicity in patient DL4b-04. 2 DLTs in patient DL4b-01.
| o | Initial clinical activity was observed with a cORR of 56% (5/9) and initial ORR of 58% (7/12) (RECIST 1.1). |
| o | 6 of 7 responses (including two unconfirmed responses with no subsequent scan available at data cut-off) were ongoing at data cut-off
with longest response at >12 months after infusion. |
| o | mDOR was not reached (min. 2.0+ months, max. 11.5+ months) at a mFU of 4.8 months. |
| o | Reduction of tumor size was observed in 11 out of 12 patients, with a deepening of response from initially stable disease (“SD”)
to partial response (“PR”) observed in two patients. |
| o | The best overall response and response over time for IMA203CD8 GEN2 are set forth in the charts below: |

Initial ORR: Objective response rate according to RECIST
1.1 at any post infusion scan; Confirmed ORR (cORR): Confirmed objective response rate according to RECIST 1.1 for patients with at
least two available post infusion scans or patients with progressive disease (PD) at any prior timepoint, patients with ongoing unconfirmed
PR not included in cORR calculation; PD: Progressive Disease; SD: Stable Disease; PR: Partial Response; cPR: Confirmed Partial Response;
BL: Baseline; BOR: Best Overall Response; CPI: Checkpoint Inhibitor .
| o | Translational data showed enhanced pharmacology of IMA203CD8 GEN2: trend towards responses at lower T cell dose and higher tumor burden
compared to IMA203 GEN1, IMA203CD8 GEN2 achieved higher peak expansion (Cmax) when normalized to infused dose and T cells showed higher,
initial activation levels without exhaustion over time. |
Development Path for IMA203 GEN1 and IMA203CD8 GEN2 Monotherapies
The goal of Immatics’ development strategy is to make its cell
therapies targeting PRAME available to the broadest possible solid cancer patient population with an initial focus on the US market. To
achieve this, Immatics has announced a three-step development strategy for leveraging the full breadth of PRAME, a target that is highly
expressed in various solid cancers.
| 1. | Focus on IMA203 GEN1 in cutaneous melanoma (potentially bundled with uveal melanoma), targeted to enter a registration-enabling Phase
2 clinical trial in 2024. Discussions with FDA to align on patient population, clinical trial design and CMC aspects are ongoing under
the RMAT designation achieved for IMA203 GEN1 in multiple cancer types including cutaneous and uveal melanoma. There are up to 3,300 HLA-A*02
and PRAME-positive cutaneous and uveal melanoma last-line patients per year in the US. A next update on the clinical development plan
is expected in the first quarter of 2024. |
| 2. | In parallel, commence dedicated dose expansion cohorts for signal finding in ovarian and uterine cancer, preferentially with IMA203CD8
GEN2. Enrollment of patients with these cancer types is already ongoing. There are up to 9,000 HLA-A*02 and PRAME-positive ovarian and
uterine last-line cancer patients per year in the US. |
| 3. | The development of a broader tumor-agnostic label in PRAME+ solid cancers, including in NSCLC, triple-negative breast cancer, and
others. This could leverage the full potential of PRAME across multiple solid cancer types. |
* * *
In connection with the foregoing, the Company issued a press release,
a copy of which is attached hereto as Exhibit 99.1, and provided a presentation, a copy of which is attached hereto as Exhibit 99.2, and
made available an updated corporate presentation, a copy of which is attached hereto as Exhibit 99.3.
Certain statements in this report may be considered forward-looking
statements. Forward-looking statements generally relate to future events or the Company’s future financial or operating performance.
For example, statements concerning timing of data read-outs for product candidates, the timing and outcome of clinical trials, the nature
of clinical trials (including whether such clinical trials will be registration-enabling), the timing of IND or CTA filing for pre-clinical
stage product candidates, the Company’s focus on partnerships to advance its strategy, and other metrics are forward-looking statements.
In some cases, you can identify forward-looking statements by terminology such as “may”, “should”, “expect”,
“plan”, “target”, “intend”, “will”, “estimate”, “anticipate”,
“believe”, “predict”, “potential” or “continue”, or the negatives of these terms or variations
of them or similar terminology. Such forward-looking statements are subject to risks, uncertainties, and other factors which could cause
actual results to differ materially from those expressed or implied by such forward looking statements. These forward-looking statements
are based upon estimates and assumptions that, while considered reasonable, Immatics and its management, are inherently uncertain. New
risks and uncertainties may emerge from time to time, and it is not possible to predict all risks and uncertainties. Factors that may
cause actual results to differ materially from current expectations include, but are not limited to, various factors beyond management's
control including general economic conditions and other risks, uncertainties and factors set forth in the Company’s Annual report
on Form 20-F and other filings with the Securities and Exchange Commission (SEC). Nothing in this report should be regarded as a representation
by any person that the forward-looking statements set forth herein will be achieved or that any of the contemplated results of such forward-looking
statements will be achieved. You should not place undue reliance on forward-looking statements, which speak only as of the date they are
made. The Company undertakes no duty to update these forward-looking statements. All the scientific and clinical data presented within
this report are – by definition prior to completion of the clinical trial and a clinical study report – preliminary in nature
and subject to further quality checks including customary source data verification.
INCORPORATION BY REFERENCE
This Report on Form 6-K (other than Exhibits 99.1,
99.2 and 99.3 hereto) shall be deemed to be incorporated by reference into the registration statements on Form F-3 (Registration Nos.
333-258351, 333-240260 and 333-274218) of Immatics N.V. and to be a part thereof from the date on which this report is filed, to the extent
not superseded by documents or reports subsequently filed or furnished.
EXHIBIT INDEX
SIGNATURES
Pursuant to the requirements of the Securities
Exchange Act of 1934, the registrant has duly caused this report to be signed on its behalf by the undersigned, thereunto duly authorized.
| |
IMMATICS N.V. |
| Date: November 8, 2023 |
|
| |
By: |
/s/ Harpreet Singh |
| |
Name: |
Harpreet Singh |
| |
Title: |
Chief Executive Officer |
Exhibit 99.1

PRESS RELEASE
Immatics
Reports Interim Clinical Data from ACTengine® IMA203 and IMA203CD8 TCR-T Monotherapies Targeting PRAME in an Ongoing Phase 1 Trial
Company
to host conference call and webcast today, November 8, at 8:30 am EST/2:30 pm CET
IMA203
data with focus on melanoma patients presented at the International Congress
of the Society for Melanoma Research today, November 8
| · | IMA203 GEN1 TCR cell therapy targeting PRAME – update on Phase
1a and Cohort A |
| o | Continues to be well tolerated |
| o | 50% confirmed objective response rate (cORR) in melanoma patients
treated at recommended Phase 2 dose; durability with some ongoing responses at >15 months and median duration of response not reached
at a median follow-up of 14.4 months |
| o | Targeted to enter registration-enabling Phase 2 trial in melanoma
in 2024; discussions with FDA ongoing based on recently obtained RMAT designation |
| · | IMA203CD8 GEN2 TCR cell therapy targeting PRAME – first clinical
data from Cohort C |
| o | Manageable tolerability, dose escalation ongoing |
| o | Initial clinical activity with 56% (5/9) cORR and 58% ORR (7/12)
observed during dose escalation dose levels 3 and 4; 6 out of 7 responses ongoing with longest response at >12 months |
| o | Enhanced pharmacology and differentiated response pattern |
| · | Signal finding in non-melanoma indications started, including ovarian
cancer, uterine cancer, NSCLC, triple-negative breast cancer, preferentially with IMA203CD8 GEN2 |
| · | Cash and cash equivalents over $500 million and cash reach well
into 2026; updates across the entire clinical portfolio of Cell Therapy and two TCR Bispecifics programs planned throughout 2024 |
Houston,
Texas and Tuebingen, Germany, November 8, 2023 – Immatics
N.V. (NASDAQ: IMTX, “Immatics”), a clinical-stage biopharmaceutical company active in the discovery and development
of T cell-redirecting cancer immunotherapies, today announced interim data from the ongoing Phase 1 trial with ACTengine®
IMA203 in patients with recurrent and/or refractory solid cancers. The update is focused on IMA203 GEN1 in melanoma at the recently defined
recommended Phase 2 dose (RP2D) and the first clinical data for IMA203CD8 GEN2.
| Immatics Press Release November 8, 2023 | 1 | 8 |
Treatment with IMA203 GEN1 monotherapy in Phase
1a and Phase 1b Cohort A at RP2D demonstrated durable objective responses in melanoma patients with one patient exceeding 12 months and
two patients exceeding 15 months post infusion and a 50% (6/12) confirmed objective response rate (cORR). In line with previous results,
IMA203 GEN1 monotherapy was well tolerated at total doses up to 10x109 TCR-T cells infused.
In addition, the first data on the company’s
second-generation product candidate IMA203CD8 demonstrated 56% (5/9) cORR with enhanced pharmacology and a differentiated response pattern
compared to IMA203 GEN1. The company plans to develop IMA203 GEN1 in melanoma and to pursue development of IMA203 in ovarian cancer, uterine
cancer, NSCLC, triple-negative breast cancer and other tumor types preferentially with IMA203CD8 GEN2.
The melanoma-focused data on IMA203 GEN1 will be
presented today by Martin Wermke, MD, Professor at the University Hospital Dresden and Coordinating Investigator of the ACTengine®
IMA203 TCR-T trial, at the 20th International Congress of the Society for Melanoma Research in Philadelphia, PA, taking place
November 6th-9th, 2023.
In addition, Dr. Wermke together with Cedrik Britten,
MD, Chief Medical Officer at Immatics will provide the complete data update during a conference
call and webcast today, November 8 at 8:30 am EST/2:30 pm CET. The presentation is available on Immatics’
website – covering the complete data set including Phase 1a, Phase 1b Cohort A and the deprioritized Cohort B
(IMA203 GEN1 combined with nivolumab).
“A cancer diagnosis can be the start of a
daunting journey characterized by devastating setbacks when conventional therapies fail. I believe that the updated data on IMA203 GEN1
shows meaningful benefit and long-term durability in melanoma patients,” said Martin Wermke, MD, Coordinating Investigator of the
ACTengine® IMA203 TCR-T trial. “With the maturation of the clinical data set, it becomes progressively evident to me that targeting
PRAME with Immatics’ IMA203 TCR-T approach has the potential to provide a durable benefit for advanced-stage checkpoint- and BRAF-inhibitor
refractory melanoma patients.”
"Today, we are excited to report on the continued
clinical progress for our ACTengine® IMA203 TCR-T cell therapies, which we believe have demonstrated meaningful clinical benefit for
last-line solid cancer patients treated with IMA203 or its second-generation product candidate IMA203CD8. We now plan to progress IMA203
into a registration-enabling Phase 2 trial in melanoma as quickly as possible, while we believe that our second-generation approach is
exhibiting unique patterns in pharmacology guiding our development efforts towards other
| Immatics Press Release November 8, 2023 | 2 | 8 |
tumor types such as ovarian, uterine, lung and
triple-negative breast cancer," commented Dr. Cedrik Britten, Chief Medical Officer at Immatics. "We plan to provide an update
on the clinical development plan for IMA203 in the first quarter of 2024 as well as updates across the entire clinical TCR cell therapy
and bispecifics portfolio throughout 2024.”
Clinical data on anti-tumor activity and
safety
IMA203 GEN1 in melanoma patients treated
at RP2D: IMA203 GEN1 demonstrates a high rate of objective responses with ongoing durability of more than 15 months after
treatment
| · | At data cut-off on September 30, 2023, a total of 16 PRAME-positive patients
with cutaneous, uveal or melanoma of unknown primary origin were infused with IMA203 GEN1 at the recommended Phase 2 dose (RP2D, 1-10x109
total TCR-T cells) across Phase 1a or Phase 1b Cohort A. |
| · | IMA203 GEN1 monotherapy continues to be well tolerated. All 16 patients
experienced cytopenia (Grade 1-4) associated with lymphodepletion as expected. Patients had mostly mild-moderate cytokine release syndrome
(CRS), of which 10 patients (63%) had Grade 1, and 5 patients (31%) Grade 2 and 1 patient (6%) Grade 3 CRS. One non-serious, mild (Grade
1) immune effector cell associated neurotoxicity syndrome (ICANS) was observed. No dose-dependent increase of CRS, no dose-limiting toxicities
(DLTs) and no IMA203-related death was observed. The safety profile for non-melanoma patients treated with IMA203 GEN1 was generally consistent
with safety in the melanoma subset and is provided in the appendix of the presentation. |
| · | 13 out of 16 infused patients were evaluable for efficacy analysis based
on at least one tumor response assessment being available post treatment. These patients received a median total infused dose of 1.73x109
IMA203 TCR-T cells (range 1.07-5.12x109 TCR-T cells). |
| · | Most patients were heavily pre-treated with a median
of 4 lines of systemic therapies, thereof a median of 2 lines of checkpoint inhibitors; all 8 cutaneous melanoma patients were checkpoint
inhibitor-refractory and 5 of 8 were BRAF inhibitor-pretreated. |
| · | 50% (6/12) confirmed objective response rate (cORR)
and 62% (8/13) initial ORR (RECIST 1.1). |
| · | Durability of responses ongoing beyond 12 months
in one patient and 15 months in two patients after treatment. |
| · | Median duration of response (mDOR) was not reached (min 2.2+ months,
max 14.7+ months) at a median follow-up (mFU) of 14.4 months. |
| · | RP2D has been defined at 1-10x109 total TCR-T cells. |
| · | Cell product manufacturing: |
| o | 7-day manufacturing process plus 7-day release testing |
| o | Manufacturing success rate: >95% to reach RP2D |
| Immatics Press Release November 8, 2023 | 3 | 8 |
| · | Immatics has recently received Regenerative Medicine Advanced Therapy (RMAT)
designation from the FDA for IMA203 GEN1 in multiple PRAME-expressing cancers, including cutaneous and uveal melanoma, and is now targeting
a registration-enabling Phase 2 trial in cutaneous melanoma potentially bundled with uveal melanoma in 2024. Discussions with FDA to align
on patient populations, trial design and CMC aspects concerning the planned Phase 2 trial are ongoing. |
IMA203CD8 GEN2 in Cohort C:
First clinical data set on IMA203CD8 shows an enhanced pharmacology profile with a differentiated response pattern compared to IMA203
GEN1
| · | At data cut-off on September 30, 2023, a total of 12 PRAME-positive patients
were infused with IMA203CD8 GEN2 across DL3 (0.2-0.48x109 TCR-T cells/m2 BSA), DL4a (0.481-0.8x109 TCR-T
cells/m2 BSA) and DL4b (0.801-1.2x109 TCR-T cells/m2) in Cohort C with a median total infused dose of
1.17x109 IMA203CD8 TCR-T cells (range 0.64-2.05x109 TCR-T cells). |
| · | All patients were heavily pre-treated with a median
of 3 lines of systemic therapies. |
| · | All patients experienced cytopenia (Grade 1-4) associated with lymphodepletion
as expected. 11 out of 12 patients (92%) experienced a cytokine release syndrome (CRS), of which 8 patients (67%) had Grade 1 or 2 CRS,
2 patients (17%) had Grade 3 CRS and 1 patient (8%) had a Grade 4 CRS. The latter patient also had a reported Grade 4 neurotoxicity. No
ICANS or neurotoxicity was reported for the other patients. No IMA203CD8-related deaths were observed. Dose-limiting toxicities (DLTs)
were reported for 2 of 4 patients treated at DL4b. No DLT was reported for all 4 patients treated at DL3, or all 4 patients treated at
DL4a. DL4a dose cohort is ongoing. |
| · | Initial clinical activity was observed with a cORR of 56% (5/9) and initial
ORR of 58% (7/12) (RECIST 1.1). |
| · | 6 of 7 responses (including two unconfirmed responses with no subsequent
scan available at data cut-off) were ongoing at data cut-off with longest response at >12 months
after infusion. |
| · | mDOR was not reached (min 2.0+ months, max 11.5+ months) at a mFU
of 4.8 months. |
| · | Reduction of tumor size was observed in 11 out of 12 patients, with a deepening
of response from initially stable disease (SD) to partial response (PR) observed in two patients. |
| · | Translational data showed enhanced pharmacology of IMA203CD8 GEN2: trend
towards responses at lower T cell dose and higher tumor burden compared to IMA203 GEN1; IMA203CD8 GEN2 achieved higher peak expansion
(Cmax) when normalized to infused dose and T cells showed higher initial activation levels without exhaustion over time. |
| Immatics Press Release November 8, 2023 | 4 | 8 |
Overview of patient characteristics and anti-tumor
activity across IMA203 clinical trial cohorts
| |
IMA203 GEN1 |
IMA203CD8 GEN2 |
| |
All Comers
(N=45)
|
Melanoma Subgroup
(N=13 out of 45)
|
All Comers
(N=12)
|
| |
Phase 1a |
Cohort A |
Phase 1a + Cohort A |
Cohort C |
| Efficacy population* |
N=27
Thereof N=7 at RP2D
|
N=18 at RP2D |
N=13 at RP2D |
N=12 |
| Dose level |
DL1-4 |
DL4/5 |
DL4/5 |
DL3/DL4a/DL4b |
| ORR |
48%
(13/27)
|
50%
(9/18)
|
62%
(8/13)
|
58%
(7/12)
|
| cORR |
19%
(5/27)
|
47%
(8/17)
|
50%
(6/12)
|
56%
(5/9)
|
| mDOR [months] |
4.4
(2.4, 23.0)
|
Not reached |
Not reached |
Not reached |
| mFU [months] |
Not defined# |
10.8 |
14.4 |
4.8 |
* Patients with at least one available tumor response
assessment post infusion; # All patients were PD at data cut-off; Initial ORR: Objective response rate according to RECIST
1.1 at any post infusion scan; Confirmed ORR (cORR): Confirmed objective response rate according to RECIST 1.1 for patients with at least
two available post infusion scans or patients with progressive disease (PD) at any prior timepoint, patients with ongoing unconfirmed
PR not included in cORR calculation; Duration of response (DOR) in confirmed responders is defined as time from first documented response
until disease progression/death. Patients with ongoing response will be censored at date of data cut-off. Median DOR (mDOR) is analyzed
by using the Kaplan-Meier method; Median Follow-up (mFU) is analyzed by using the reverse Kaplan-Meier method.
The full data analysis including IMA203 GEN1 in
Phase 1a and Cohort A as well as deprioritized Cohort B (IMA203 in combination with a checkpoint inhibitor), is available as part of
the presentation on the company’s website.
Development path for IMA203 GEN1 and IMA203CD8
GEN2 monotherapies
The goal of Immatics’ development strategy
is to make its cell therapies targeting PRAME available to the broadest possible solid cancer patient population with an initial focus
on the US market. To achieve this, Immatics has announced a three-step development strategy for leveraging the full breadth of PRAME,
a target that is highly expressed in various solid cancers.
| 1. | Focus on IMA203 GEN1 in cutaneous melanoma (potentially bundled with uveal melanoma), targeted to enter
a registration-enabling Phase 2 clinical trial in 2024. Discussions with FDA to align on patient population, clinical trial design and
CMC aspects are ongoing under the RMAT designation achieved for IMA203 GEN1 in multiple cancer types including cutaneous and uveal melanoma.
There are up to 3,300 HLA-A*02 and PRAME-positive cutaneous and |
| Immatics Press Release November 8, 2023 | 5 | 8 |
uveal melanoma
last-line patients per year in the US. A next update on the clinical development plan is expected in the first quarter of 2024.
| 2. | In parallel, commence dedicated dose expansion cohorts for signal finding in ovarian and uterine cancer,
preferentially with IMA203CD8 GEN2. Enrollment of patients with these cancer types is already ongoing. There are up to 9,000 HLA-A*02
and PRAME-positive ovarian and uterine last-line cancer patients per year in the US. |
| 3. | The development of a broader tumor-agnostic label in PRAME+ solid cancers, including in NSCLC, triple-negative
breast cancer, and others. This could leverage the full potential of PRAME across multiple solid cancer types. |
Immatics conference call and webcast
Immatics will host a conference
call and webcast today, November 8, 2023, at 8:30 am EST/2:30 pm CET to discuss the clinical data. The presentation can be
accessed directly through this link. A replay of the webcast will be made available shortly after
the conclusion of the call and archived on the Immatics website for at least 90 days.
About IMA203 and target PRAME
ACTengine® IMA203 T cells are directed against
an HLA-A*02-presented peptide derived from preferentially expressed antigen in melanoma (PRAME), a protein frequently expressed in a large
variety of solid cancers, thereby supporting the program’s potential to address a broad cancer patient population. Immatics’
PRAME peptide is present at a high copy number per tumor cell and is homogeneously and specifically expressed in tumor tissue. The peptide
has been identified and characterized by Immatics’ proprietary mass spectrometry-based target discovery platform, XPRESIDENT®.
Through its proprietary TCR discovery and engineering platform XCEPTOR®, Immatics has generated a highly specific T cell receptor
(TCR) against this target for its TCR-based cell therapy approach, ACTengine® IMA203.
ACTengine® IMA203 TCR-T is currently being
evaluated in Phase 1 Cohort A IMA203 GEN1 monotherapy, and Cohort C IMA203CD8 GEN2 monotherapy, where IMA203 engineered T cells are co-transduced
with a CD8αβ co-receptor. As previously reported, Cohort B IMA203 in combination with an immune checkpoint inhibitor has been
deprioritized.
About ACTengine®
ACTengine® is a personalized cell therapy approach
for patients with advanced solid tumors. The patient’s own T cells are genetically engineered to express a novel, proprietary TCR
directed
| Immatics Press Release November 8, 2023 | 6 | 8 |
against a defined cancer target. The modified T
cells are then reinfused into the patient to attack the tumor. The approach is also known as TCR-engineered cell therapy (TCR-T). All
Immatics’ ACTengine® product candidates are manufactured utilizing a proprietary manufacturing process designed to enhance T
cell engraftment and persistence in vivo.
The ACTengine® T cell products are manufactured
at the Evelyn H. Griffin Stem Cell Therapeutics Research Laboratory in collaboration with UTHealth.
- END -
About Immatics
Immatics combines the discovery of true targets
for cancer immunotherapies with the development of the right T cell receptors with the goal of enabling a robust and specific T cell response
against these targets. This deep know-how is the foundation for our pipeline of Adoptive Cell Therapies and TCR Bispecifics as well as
our partnerships with global leaders in the pharmaceutical industry. We are committed to delivering the power of T cells and to unlocking
new avenues for patients in their fight against cancer.
Immatics intends to use
its website www.immatics.com as a means of disclosing material non-public information. For regular
updates, you can also follow us on Twitter, Instagram
and LinkedIn.
Forward-Looking Statements:
Certain statements in
this presentation may be considered forward-looking statements. Forward-looking statements generally relate to future events or the Company’s
future financial or operating performance. For example, statements concerning timing of data read-outs for product candidates, the timing
and outcome of clinical trials, the nature of clinical trials (including whether such clinical trials will be registration-enabling),
the timing of IND or CTA filing for pre-clinical stage product candidates, estimated market opportunities of product candidates, the Company’s
focus on partnerships to advance its strategy, and other metrics are forward-looking statements. In some cases, you can identify forward-looking
statements by terminology such as “may”, “should”, “expect”, “plan”, “target”,
“intend”, “will”, “estimate”, “anticipate”, “believe”, “predict”,
“potential” or “continue”, or the negatives of these terms or variations of them or similar terminology. Such
forward-looking statements are subject to risks, uncertainties, and other factors which could cause actual results to differ materially
from those expressed or implied by such forward looking statements. These forward-looking statements are based upon estimates and assumptions
that, while considered reasonable, Immatics and its management, are inherently uncertain. New risks and uncertainties may emerge from
time to time, and it is not possible to predict all risks and uncertainties. Factors that may cause actual results to differ
| Immatics Press Release November 8, 2023 | 7 | 8 |

materially from current
expectations include, but are not limited to, various factors beyond management's control including general economic conditions and other
risks, uncertainties and factors set forth in the Company’s Annual report on Form 20-F and other filings with the Securities and
Exchange Commission (SEC). Nothing in this press release should be regarded as a representation by any person that the forward-looking
statements set forth herein will be achieved or that any of the contemplated results of such forward-looking statements will be achieved.
You should not place undue reliance on forward-looking statements, which speak only as of the date they are made. The Company undertakes
no duty to update these forward-looking statements. All the scientific and clinical data presented within this press release are –
by definition prior to completion of the clinical trial and a clinical study report – preliminary in nature and subject to further
quality checks including customary source data verification.
For more information,
please contact:
Media
Eva Mulder
or Charlotte Spitz
Trophic Communications
Phone: +31
65 2331 579
immatics@trophic.eu
Investor
Relations
Sabrina Schecher,
Ph.D.
Senior Director,
Investor Relations
Phone: +49
89 262002433
InvestorRelations@immatics.com
| Immatics Press Release November 8, 2023 | 8 | 8 |
Exhibit 99.2

© Immatics. Not for further reproduction or distribution. Delivering the Power of T cells to Cancer Patients © Immatics. Not for further reproduction or distribution. ACTengine® IMA203 / IMA203CD8 TCR - T Monotherapy Targeting PRAME – Phase 1 Interim Data Update Martin Wermke , Professor at the University Hospital Dresden and Coordinating Investigator of the ACTengine ® IMA203 TCR - T trial Cedrik Britten , Chief Medical Officer, Immatics Harpreet Singh , Chief Executive Officer, Immatics November 8, 2023 Additional oral presentation by Martin Wermke at the Society for Melanoma Research Congress on November 08 , 2023 Data cut - off Sep 30, 2023

Forward - Looking Statement This presentation (“Presentation”) is provided by Immatics N . V . (“Immatics” or the “Company”) for informational purposes only . The information contained herein does not purport to be all - inclusive and none of Immatics, any of its affiliates, any of its or their respective control persons, officers, directors, employees or representatives makes any representation or warranty, express or implied, as to the accuracy, completeness or reliability of the information contained in this Presentation . Forward - Looking Statements . Certain statements in this presentation may be considered forward - looking statements . Forward - looking statements generally relate to future events or the Company’s future financial or operating performance . For example, statements concerning timing of data read - outs for product candidates, the timing and outcome of clinical trials, the nature of clinical trials (including whether such clinical trials will be registration - enabling), the timing of IND or CTA filing for pre - clinical stage product candidates, estimated market opportunities of product candidates, the Company’s focus on partnerships to advance its strategy, and other metrics are forward - looking statements . In some cases, you can identify forward - looking statements by terminology such as “may”, “should”, “expect”, “plan”, “target”, “intend”, “will”, “estimate”, “anticipate”, “believe”, “predict”, “potential” or “continue”, or the negatives of these terms or variations of them or similar terminology . Such forward - looking statements are subject to risks, uncertainties, and other factors which could cause actual results to differ materially from those expressed or implied by such forward looking statements . These forward - looking statements are based upon estimates and assumptions that, while considered reasonable, Immatics and its management, are inherently uncertain . New risks and uncertainties may emerge from time to time, and it is not possible to predict all risks and uncertainties . Factors that may cause actual results to differ materially from current expectations include, but are not limited to, various factors beyond management's control including general economic conditions and other risks, uncertainties and factors set forth in the Company’s Annual report on Form 20 - F and other filings with the Securities and Exchange Commission (SEC) . Nothing in this presentation should be regarded as a representation by any person that the forward - looking statements set forth herein will be achieved or that any of the contemplated results of such forward - looking statements will be achieved . You should not place undue reliance on forward - looking statements, which speak only as of the date they are made . The Company undertakes no duty to update these forward - looking statements . No Offer or Solicitation . This communication is for informational purposes only and does not constitute, or form a part of, an offer to sell or the solicitation of an offer to sell or an offer to buy or the solicitation of an offer to buy any securities, and there shall be no sale of securities, in any jurisdiction in which such offer, solicitation or sale would be unlawful prior to registration or qualification under the securities laws of any such jurisdiction . No offer of securities shall be made except by means of a prospectus meeting the requirements of Section 10 of the Securities Act of 1933 , as amended, or in an offering exempt from registration . Certain information contained in this Presentation relates to or is based on studies, publications, surveys and the Company’s own internal estimates and research . In addition, all of the market data included in this presentation involves a number of assumptions and limitations, and there can be no guarantee as to the accuracy or reliability of such assumptions . Finally, while the Company believes its internal research is reliable, such research has not been verified by any independent source . All the scientific and clinical data presented within this presentation are – by definition prior to completion of the clinical trial and a clinical study report – preliminary in nature and subject to further quality checks including customary source data verification . 2

Realizing the Full Multi - Cancer Opportunity of PRAME ACTengine® IMA203 (TCR Cell Therapy) and TCER® IMA402 (TCR Bispecific) 3 ACTengine® IMA203 (TCR Cell Therapy) 1 PRAME target prevalence is based on TCGA (for SCLC: in - house) RNAseq data combined with a proprietary mass spec - guided RNA expre ssion threshold; 2 Uveal melanoma target prevalence is based on IMADetect® qPCR testing of screening biopsies from clinical trial patients (n=33); NSCLC: Non - small cell lung cancer, TNBC: Triple - negative breast cancer, HNSCC: Head and neck squamous cell carcinoma; HCC: Hepatocellular carcinoma Phase 1b dose expansion ongoing Dose escalation of Phase 1/2 trial ongoing TCER® IMA402 (TCR Bispecific) Focus today Indication % PRAME positive patients 1 Uterine Carcinoma Uterine Carcinosarcoma Sarcoma Subtypes Cut. Melanoma Uveal Melanoma 2 Ovarian Carcinoma Squamous NSCLC TNBC Small Cell Lung Cancer Kidney Carcinoma Cholangiocarcinoma HNSCC Esophageal Carcinoma Breast Carcinoma Adeno NSCLC HCC Bladder Carcinoma 97% 100% up to 100% ≥ 95% ≥ 91% 84% 68% 63% 45% up to 40% 33% 27% 27% 26% 25% 18% 18% Focus today

ACTengine® IMA203 / IMA203CD8 TCR - T Monotherapy Two Assets with Distinct Opportunities and Near - Term Catalysts 4 GEN1: IMA203 in Melanoma at RP2D GEN2: IMA203CD8 in Solid Tumors Initial Clinical Data • Complete dose escalation • Signal finding in non - melanoma indications, such as ovarian cancer, uterine cancer, NSCLC, triple - negative breast cancer and others Development Path Clinical Data Cell Product Manufacturing • 7 - day manufacturing process, plus 7 - day release testing • RP2D defined at 1 - 10x10 9 total TCR - T cells • Manufacturing success rate: >95% • Well tolerated • 50% (6/12) confirmed objective response rate ( cORR ) • Durability with ongoing responses at 15+ months; mDOR not reached at mFU of 14.4 months • Manageable tolerability • 56% (5/9) confirmed objective response rate ( cORR ) • Durable response at 12+ months; mDOR not reached at mFU of 4.8 months • 6 out of 7 responses ongoing at data cut - off • Enhanced pharmacology with differentiated response pattern Development Path • FDA RMAT designation for multiple PRAME+ cancers including cutaneous & uveal melanoma • IMA203 GEN1 in melanoma targeted to enter registration - enabling Phase 2 trial in 2024 • Update on clinical development plan in 1Q 2024 mDOR : median Duration of Response; mFU : median Follow - up ; RP2D: Recommended Phase 2 Dose Data cut - off Sep 30, 2023

ACTengine® IMA203 / IMA203CD8 TCR - T Trial in Advanced Solid Tumors Overview D ose Level 1 - 4 ( total N=27): Patients in DL4 (N=7) treated at RP2D Phase 1b Dose Expansion Phase 1a Dose Escalation Efficacy population shown: patients treated with IMA203 (Cohort A) or IMA203CD8 (Cohort C) and with at least one available tu mor response assessment post infusion; RP2D: Recommended Phase 2 Dose of 1 - 10x10 9 total TCR - T cells; IMA203 DL4: 0.2 - 1.2x10 9 TCR - T cells/m 2 BSA, IMA203 DL5: 1.201 x 4.7x10 9 TCR - T cells/m 2 BSA; IMA203CD8 DL3: 0.2 - 0.48x10 9 TCR - T cells/m 2 BSA, IMA203CD8 DL4a: 0.481 - 0.8x10 9 TCR - T cells/m 2 BSA, IMA203CD8 DL4b: 0.801 - 1.2x10 9 TCR - T cells/m 2 Data cut - off Sep 30, 2023 Phase 1a and Cohort A data set in appendix; Cohort B deprioritized, detailed analysis in appendix GEN1 : IMA203 GEN2 : IMA203CD8 Functional CD8 TCR - T cells only Functional CD8 and CD4 TCR - T cells Today’s update focuses on 13 melanoma patients treated at RP2D with IMA203 GEN1 and 12 all comers patients treated with IMA203CD8 GEN2 Melanoma Patients at RP2D: Total N=13 (5 Ph1a + 8 Cohort A) Cohort C (N=12): Dose Level 3/4a/4b Dose escalation ongoing Cohort A (total N=18) : Dose Level 4/5 All patients treated at RP2D 5

Overview of Patient Characteristics and Responses 6 * Patients with at least one available tumor response assessment post infusion; # All patients were PD at data cut - off; Initial ORR: Objective response rate according to RECIST 1.1 at any post infusion scan; Confirmed ORR ( cORR ): Confirmed objective response rate according to RECIST 1.1 for patients with at least two available post infusion scans or patients with progressive disease (PD ) a t any prior timepoint, patients with ongoing unconfirmed PR not included in cORR calculation; Duration of response (DOR) in confirmed responders is defined as time from first documented response until disease progression/death. Patients with ongoing response wil l be censored at date of data cut - off. Median DOR is analyzed by using the Kaplan - Meier method; Median Follow - up is analyzed by using the reverse Kaplan - Meier method; DOR: Duration of Response; FU: Follow - up IMA203 GEN1 IMA203CD8 GEN2 All Comers (N=45) Melanoma Subgroup (N=13 of 45) All Comers (N=12) Phase 1a Cohort A Phase 1a + Cohort A Cohort C Efficacy population* N=27 Thereof N=7 at RP2D N=18 at RP2D N=13 at RP2D N=12 Prior lines of systemic treatment ( median, min, max) 4 (1, 8) 3 (0, 10) 4 (0, 7) 3 (1, 5) LDH at baseline >1 x ULN [% of patients] 66.7 50.0 53.8 50.0 Baseline tumor burden Median target lesion sum of diameter [mm] (min, max) 133.0 (29, 219.7) 58.9 (21, 207.3) 52.0 (21.0, 178.7) 79.8 (20.0, 182.0) Dose level DL1 - 4 DL4/5 DL4/5 DL3/DL4a/DL4b ORR 48% (13/27) 50% (9/18) 62% (8/13) 58% (7/12) cORR 19% (5/27) 47% (8/17) 50% (6/12) 56% (5/9) mDOR [months] 4.4 (2.4, 23.0) Not reached Not reached Not reached mFU [months] Not defined # 10.8 14.4 4.8 Data cut - off Sep 30, 2023 Heavily Pretreated Patient Population across Clinical Trial Cohorts

ACTengine® IMA203 TCR - T Interim Update Delivering a Meaningful Benefit to Patients with an Unmet Medical Need 7 IMA203 GEN1 Monotherapy Phase 1a & Cohort A – Focus on Melanoma at RP2D IMA203CD8 GEN2 Monotherapy Cohort C – First Data Set on 2 nd Generation Summary & Next Development Steps

8 Data cut - off Sep 30, 2023 IMA203 GEN1 in All Melanoma Patients at RP2D – Most Frequent Adverse Events • Expected cytopenia (Grade 1 - 4) associated with lymphodepletion in all patients • Mostly mild to moderate cytokine release syndrome (CRS) • 63% (10/16) with Grade 1 CRS • 31% (5/16) with Grade 2 CRS • 6% (1/16) with Grade 3 CRS (Phase 1a patient; recovered to Grade 2 after 3 days, no need for vasopressors and/or ventilation) • No dose - dependent increase of CRS • O ne non - serious, mild (Grade 1) ICANS 2 in DL5 • No dose - limiting toxicity • No IMA203 - related deaths • For full IMA203 GEN1 monotherapy safety profile (generally consistent with safety in melanoma subset), see appendix 1 Three cutaneous melanoma patients treated with IMA203 and pending post infusion scan included in safety population, but not e ff icacy population; 2 I CANS: Immune Effector Cell - Associated N eurotoxicity S yndrome ; CRS and ICANS graded by CARTOX criteria ( Neelapu et al ., 2018) N=16 Patients in Safety Population 1 IMA203 GEN1 monotherapy continues to be well tolerated at total doses between 1 - 10x10 9 TCR - T cells (RP2D)
# # # # # # # # # # IMA203 GEN1 in All Melanoma Patients at RP2D (N=13) – BOR and Response over Time Durable Responses 15+ Months after Treatment 9 Data cut - off Sep 30, 2023 Ongoing ORR 62% (8/13) cORR 50% (6/12) Initial ORR: Objective response rate according to RECIST 1.1 at any post infusion scan; Confirmed ORR ( cORR ): Confirmed objective response rate according to RECIST 1.1 for patients with at least two available post infusion scans or pat ients with progressive disease (PD) at any prior timepoint, patients with ongoing unconfirmed PR not included in cORR calculation; Duration of response (DOR) in confirmed responders is defined as time from first documented response until disease progression/death. Patients with ongoing response will be censored at date of data cut - off. Median DOR is analyzed by using the Kaplan - Meier method; Median Follow - up is analyzed by using the reverse Kaplan - Meier method; PD: Progressive Disease; SD: Stable Disease; PR: Partial Response; cPR : Confirmed Partial Response; BL: Baseline; BOR: Best Overall Response; DOR: Duration of Response; Scans at approximately week 6, month 3 and then every 3 months # Patients in Phase 1a Median DOR, min, max DOR Not reached, 2.2+, 14.7+ months Median Follow - up 14.4 months

10 High Medical Need in Cutaneous and Uveal Melanoma Clinically and Commercially Attractive Features of IMA203 Cutaneous Melanoma Uveal Melanoma Patient Population 2L+ CPI - refractory, BRAF/MEK inhibitor - refractory if BRAF mutation+ 2L+ Kimmtrak - refractory, CPI/chemotherapy - refractory IMA203 Opportunity ~3,000 HLA - A*02:01 and PRAME - positive cutaneous melanoma patients annually in the US 1 ~300 HLA - A*02:01 and PRAME - positive uveal melanoma patients annually in the US 2 Well tolerated Mostly mild to moderate CRS, infrequent & mild ICANS Promising anti - tumor activity ( cORR , mDOR ) Leukapharesis as source for cell product, no surgery required Short manufacturing time of 7 days plus 7 days of QC release testing Low dose IL - 2 post IMA203 infusion with better tolerability profile than high dose IL - 2 CPI: Checkpoint inhibitor; 1 Based on annual mortality of ~7,700 cutaneous melanoma patients in the US, HLA - A*02:01 prevalence of 41% in the US and PRAME pr evalence of 95% (TCGA RNAseq data combined with proprietary MS - guided RNA expression threshold); 2 Based on annual mortality of ~800 uveal melanoma patients in the US, HLA - A*02:01 prevalence of 41% in the US and PRAME prevalen ce of 91% (IMADetect® qPCR testing of screening biopsies from clinical trial patients (n=33)) ≥95% of cutaneous melanoma patients are PRAME - positive Data cut - off Sep 30, 2023 IMA203 GEN1 in Melanoma Targeted to Enter Registration - Enabling Phase 2 Trial in 2024

ACTengine® IMA203 TCR - T Interim Update Delivering a Meaningful Benefit to Patients with an Unmet Medical Need 11 IMA203 GEN1 Monotherapy Phase 1a & Cohort A – Focus on Melanoma at RP2D IMA203CD8 GEN2 Monotherapy Cohort C – First Data Set on 2 nd Generation Summary & Next Development Steps

IMA203CD8 GEN2 – IMA203 TCR - T Monotherapy Leveraging CD8 and CD4 cells Differentiated Pharmacology Compared to 1 st - Generation TCR - only Approaches • IMA203CD8 GEN2 designed to broaden the clinical potential of IMA203 TCR - T monotherapy by adding functional CD4 T cells via co - transduction of CD8 αβ alongside PRAME TCR • Activated CD4 T cells aid activity of other immune cells by releasing cytokines and acquire cytotoxic functions • Functional CD4 T cells mediate longer anti - tumor activity than CD8 T cells and potentiate the anti - tumor activity of the cell product in preclinical studies 1 • Data from CD19 CAR - T - treated leukaemia patients suggest a relevant role of engineered CD4 T cells in long - term durability 2 TUMOR CELL DEATH CD4 T CELL Cytotoxic Activity CD8 T CELL T cell Help Cytotoxic Activity 12 1 Internal data not shown here, published in Bajwa et al. 2021, Journal for Immunotherapy of Cancer; 2 M elenhorst et al. 2022 Nature , Bai et al. 202,2 Science Advances CD8 PRAME TCR

IMA203CD8 GEN2 in Cohort C (N=12) – Most Frequent Adverse Events Manageable Tolerability in 12 Patients Treated with IMA203CD8 at 3 Escalating Dose Levels 1 • Expected cytopenia (Grade 1 - 4) associated with lymphodepletion in all patients • Cytokine release syndrome (CRS) in 92% (11/12) of patients: Trend towards more severe CRS at higher doses, in all cases well manageable • 67 % (8/12) with Grade 1 or 2 CRS (4 in DL3, 3 in DL4a, 1 in DL4b) • 17% (2/12) with Grade 3 CRS (2 in DL4b; patient C - DL4b - 04, see also description below) • 8% (1/12) with Grade 4 CRS (1 in DL4b, patient C - DL4b - 01, see also description below ) • One patient with neurotoxicity (see below), no ICANS 2 or neurotoxicity reported for the other patients • Dose - limiting toxicities (DLTs) at Dose Level 4b were observed in 2 of 4 patients 1) In patient C - DL4b - 01 treated with highest possible dose at DL4b, high biological activity ( in vivo T cell expansion) observed; patient developed Grade 4 neurotoxicity and Grade 4 CRS on day 6 after infusion, combined with Grade 3 Hemophagocytic Lymphohistiocytosis (HLH) 2) Patient C - DL4b - 04 treated at DL4b developed Grade 3 CRS with transient Grade 3 liver enzyme (ALT) increase that resolved to Grad e 2 within 10 days; no need for vasopressors or ventilation at any time • No high - grade CRS, no neurotoxicity and no DLTs were reported for 4 patients treated at DL3 and 4 patients treated at DL4a • No IMA203CD8 - related deaths • Expanded DL4a dose cohort ongoing 13 1 N=4 DL3, N=4 DL4a, N=4 DL4b, DL3: 0.2 - 0.48x10 9 TCR - T cells/m 2 BSA, DL4 is split into a DL4a (0.481 - 0.8x10 9 TCR - T cells/m 2 BSA) and DL4b (0.801 - 1.2x10 9 TCR - T cells/m 2 BSA); 2 I CANS: Immune Effector Cell - Associated N eurotoxicity S yndrome ; CRS and ICANS graded by CARTOX criteria ( Neelapu et al ., 2018) IMA203CD8 GEN2 monotherapy shows a manageable tolerability profile Data cut - off Sep 30, 2023

IMA203CD8 GEN2 in Cohort C (N=12 # ) – BOR and Response over Time Deepening of Response from SD to PR in 2 Patients, 6 Responses Ongoing 14 • 6 out of 7 responses ongoing • 11/12 patients show tumor shrinkage • Deepening of response from SD to PR in two patients (C - DL4a - 01, C - DL4a - 03) • Ongoing durable response 12+ months after infusion Median DOR, min, max DOR Not reached, 2.0+, 11.5+ months Median Follow - up 4.8 months ORR 58% (7/12) cORR 56% (5/9) Initial ORR: Objective response rate according to RECIST 1.1 at any post infusion scan; Confirmed ORR ( cORR ): Confirmed objective response rate according to RECIST 1.1 for patients with at least two available post infusion scans or pat ients with progressive disease (PD) at any prior timepoint, patients with ongoing unconfirmed PR not included in cORR calculation; Duration of response (DOR) in confirmed responders is defined as time from first documented response until disease progressio n/d eath. Patients with ongoing response will be censored at date of data cut - off. Median DOR is analyzed by using the Kaplan - Meier method; Median Follow - up is analyzed by using the reverse Kaplan - Meier method; PD: Progressive Disease; SD: Stable Disease; PR: Partial Response; cPR : Confirmed Partial Response; BL: Baseline; BOR: Best Overall Response; DOR: Duration of Response # Patient C - DL4a - 04 was PD ~6 weeks after infusion, not shown due to non - evaluable target lesions at tumor assessment Scans at approximately week 6, month 3 and then every 3 months Ongoing Data cut - off Sep 30, 2023 * Clinical tumor progress after 4.9 months post infusion, investigator information *

IMA203CD8 GEN2: Translational Data Shows Enhanced Pharmacology Cohort A IMA203 GEN1 (All Patients at RP2D) vs Cohort C IMA203CD8 GEN2 15 Trend towards responses at lower cell dose and higher tumor burden with IMA203CD8 Higher peak expansion ( C max ) of IMA203CD8 T cells when normalized to infused dose Higher activation levels in IMA203CD8 T cells at week 1… …without exhaustion over time Initial translational data indicates higher biological and clinical activity of IMA203CD8 GEN2 % PD - 1 of specific T cells at week1: for patient A - DL5 - 05 data not available for week 1 0 5×10 5 1×10 6 1.5×10 6 2×10 6 2.5×10 6 V e c t o r c o p i e s / μ g g D N A p=0.0010 PR cPR PD/SD Cohort A IMA203 GEN1 Cohort C IMA203CD8 GEN2 Data cut - off Sep 30, 2023

ACTengine® IMA203 TCR - T Interim Update Delivering a Meaningful Benefit to Patients with an Unmet Medical Need 16 IMA203 GEN1 Monotherapy Phase 1a & Cohort A – Focus on Melanoma at RP2D IMA203CD8 GEN2 Monotherapy Cohort C – First Data Set on 2 nd Generation Summary & Next Development Steps

ACTengine® IMA203 / IMA203CD8 TCR - T Monotherapy Targeting PRAME Summary of GEN1 and GEN2 Clinical Data and Planned Next Steps 17 Next Step Alignment with FDA on patient population, trial design, CMC targeting registration - enabling Phase 2 trial in melanoma • Well tolerated, mostly mild to moderate CRS, infrequent & mild ICANS • 50% (6/12) cORR , mDOR not reached at mFU of 14.4 months • Durability with ongoing responses at 15+ months in some patients • RP2D defined at 1 - 10x10 9 total TCR - T cells • FDA RMAT designation received in multiple PRAME expressing cancers including cutaneous and uveal melanoma • Enhanced primary and secondary pharmacology when compared to GEN1 • Manageable tolerability (2 DLTs at DL4b, dose escalation ongoing) • Initial clinical activity observed with differentiated response pattern • 56% (5/9) cORR • 6 out of 7 responses ongoing at data cut - off, durable response at 12+ months • SD converting to PR over time (N=2) • Enhanced biological efficacy with PRs at lower T cell:tumor cell ratio compared to IMA203 GEN1 IMA203 GEN1 Monotherapy in Melanoma at RP2D IMA203CD8 GEN2 Monotherapy IMA203 GEN1 Monotherapy in Melanoma at RP2D Next Step Complete dose escalation and further dose expansion with focus on non - melanoma patients Data cut - off Sep 30, 2023

PRAME mRNA expression in IMA203 GEN1 Phase 1a and Cohort A responders at RP2D (n=13) PRAME mRNA expression in IMA203CD8 GEN2 Cohort C responders (n=7) Potential of IMA203 in Additional Solid Cancer Indications Based on PRAME Expression in IMA203 GEN1 and IMA203CD8 GEN2 Responders 18 % PRAME - positive patients 1 PRAME target expression distribution (blue histogram) based on TCGA RNAseq data, patient data (black dots) based on IMADetect ® q PCR testing of screening biopsies; 1 PRAME target prevalence is based on TCGA RNAseq data combined with a proprietary MS - guided RNA expression threshold; 2 PRAME target prevalence in uveal melanoma based on IMADetect® qPCR testing of screening biopsies from clinical trial patients ( n=33) demonstrates substantial higher prevalence of 91% compared to prevalence based on TCGA data of 50%, TCGA: early & late - stage primary tumor samples, Immatics clinical trials: late - stage/metastatic tumor samples, Role of PRAME in metastasis of uveal melanoma: Field et al. 2016 Clinical Cancer Research; MS: mass spectrometry Data cut - off Sep 30, 2023 ≥ 95% ≥ 91% (50% 2 ) 97% 100% 84% 68% 63% 27% Immatics’ current MS - guided mRNA threshold for patient selection Selected indications Clinical activity shown No clinical activity expected Potential opportunity to see clinical activity

ACTengine® IMA203 / IMA203CD8 TCR - T Monotherapy Targeting PRAME Leveraging the Full Breath of PRAME in Three Steps 19 Development Strategy Step 1 IMA203 GEN1 in cutaneous melanoma (potentially bundled with uveal melanoma) as first tumor type targeted to enter registration - enabling trial Signal finding in ovarian cancer and uterine cancer in dedicated dose expansion cohorts, preferentially with IMA203CD8 GEN2 Pursue tumor - agnostic label in PRAME+ solid cancers to leverage full breadth of PRAME - including NSCLC, triple - negative breast cancer and others Step 2 Step 3 2024 2024

Upcoming 2024 Catalysts for ACTengine® and TCER® Clinical Lead Assets Projected Cash Runway Well into 2026 to Reach Multiple Value Inflections Points 20 IMA203 GEN1 • Update on clinical development plan in 1Q 2024 • Targeted registration - enabling Phase 2 trial for ACTengine® IMA203 GEN1 in melanoma IMA203CD8 GEN2 • Interim data update with longer follow - up planned ACTengine® IMA203 / IMA203CD8 (PRAME) First clinical data update from dose escalation in ongoing Phase 1 trial planned TCER® IMA401 (MAGEA4/8) First clinical data update from dose escalation in ongoing Phase 1/2 trial planned Initial focus indications: Ovarian cancer, uterine cancer, lung cancer, melanoma and others TCER® IMA402 (PRAME) Updates planned across the entire clinical portfolio throughout 2024

University Hospital Dresden University Hospital Bonn University Hospital Würzburg Columbia University University of Pittsburgh MD Anderson Cancer Center University Hospital Hamburg Dr. D . Araujo Dr. A . Tsimberidou Dr. A. Jazaeri Dr. S . Patel Dr. W. Alsdorf Dr. T . Holderried Dr. M . C hatterjee Dr. J . Luke Germany United States Dr. M . Wermke … and the Investigators at the Clinical Sites Dr. R . Reshef 21 We are Immensely Grateful to the Patients, Their Families … Dr. L. Hernandez - Aya University of Miami Health System

Delivering s the Power of T cells to Cancer Patients © Immatics. Not for further reproduction or distribution. www.immatics.com Q&A

Appendix – Additional Data 1. Patient Flow and PRAME Expression in Pre - Treatment Tumor Biopsies 2. Dose Escalation and Cohort A IMA203 GEN1 3. Cohort B IMA203 GEN1 + Nivolumab 4. Cohort C IMA203 GEN2 5. Manufacturing and in vivo Engraftment Data IMA203 GEN1 and IMA203CD8 GEN2

ACTengine® IMA203/IMA203CD8 TCR - T Monotherapy – Patient Flow 24 HLA - A*02 Testing Blood sample; Central lab Treatment & Observation Phase Long Term Follow - up Screening & Manufacturing Phase Manufacturing by Immatics Infusion of ACTengine® IMA203 TCR - T Product Lymphodepletion * Target Profiling IMADetect® Biopsy or archived tissue Low dose IL - 2 ** Safety and efficacy monitoring for 12 months Leukapheresis x x Expression Antigen 1 3 2 Short process time of 14 days * 30 mg/m 2 Flu darabine and 500 mg/m 2 Cy clophosphamide for 4 days; ** 1m IU daily days 1 - 5 and twice daily days 6 - 10 7 - day manufacturing process applying CD8/CD4 T cell selection 7 - day QC release testing Cut. Melanoma Uveal Melanoma Uterine Carcinoma Ovarian Carcinoma 95% (58/61) 91% (30/33) 89% (8/9) 82% (23/28) Patient screening data from Immatics’ clinical trials:

PRAME Expression in Pre - Treatment Tumor Biopsies Comparable PRAME Expression Levels in Patients Treated in Phase 1a Dose Escalation, Cohort A and C 25 Data cut - off Sep 30, 2023 PRAME RNA expression in pre - treatment biopsies relative to threshold Immatics’ mass spectrometry - guided mRNA threshold

PRAME Expression in Pre - Treatment Tumor Biopsies Responders in Cohort A IMA203 GEN1 and Cohort C IMA203CD8 GEN2 26 Indication No significant difference in PRAME expression between Cohort A and C responders Best Overall Response PRAME RNA expression in pre - treatment biopsies relative to threshold Immatics’ mass spectrometry - guided mRNA threshold A - DL5 - 01 A - DL4 - 02 A - DL5 - 03 A - DL5 - 06 A - DL4 - 03 A - DL5 - 07 A - DL4 - 01 A - DL5 - 05 A - DL5 - 10 C - DL3 - 04 C - DL4a - 02 C - DL4b - 04 C - DL4a - 01 C - DL4a - 03 C - DL4b - 02 A - DL3 - 02 Immatics ’ mass spectrometry - guided mRNA threshold A - DL5 - 01 A - DL4 - 02 A - DL5 - 03 A - DL5 - 06 A - DL4 - 03 A - DL5 - 07 A - DL4 - 01 A - DL5 - 05 A - DL5 - 10 C - DL3 - 04 C - DL4a - 02 C - DL4b - 04 C - DL4a - 01 C - DL4a - 03 C - DL4b - 02 A - DL3 - 02 IMA203 achieved objective responses at all expression levels above threshold Mann - Whitney U test Data cut - off Sep 30, 2023

Appendix – Additional Data 1. Patient Flow and PRAME Expression in Pre - Treatment Tumor Biopsies 2. Dose Escalation and Cohort A IMA203 GEN1 3. Cohort B IMA203 GEN1 + Nivolumab 4. Cohort C IMA203 GEN2 5. Manufacturing and in vivo Engraftment Data IMA203 GEN1 and IMA203CD8 GEN2

IMA203 GEN1 – Melanoma as First Indication for Pivotal Development 28 * Patients with at least one post treatment tumor response assessment Patient characteristics All comers Cohort A Melanoma pts Ph1a & Cohort A at RP2D Ovarian cancer pts Ph1a & Cohort A at RP2D Efficacy population* 18 13 4 Prior lines of treatment Median (min, max) 3 (0, 10) 4 (0, 7) 4.5 (3, 10) LDH at baseline >1 x ULN [% of patients] 50.0 53.9 100.0 Baseline tumor burden Target lesion sum of diameter [mm] (median, min, max) 58.9 (21.0, 207.3) 52.0 (21.0, 178.7) 108.8 (50.6, 207.3) Patient Numbers* ALL Melanoma Ovarian Cancer Synovial Sarcoma H&N Cancer Others Phase 1a RP2D 7 5 0 0 0 2 Cohort A RP2D 18 8 4 3 1 2 All 8 cut. melanoma patients were CPI - refractory and 5 of 8 were BRAF - inhibitor pretreated • Sub - group analysis per tumor type at target dose includes data from Phase 1a plus Cohort A at RP2D • Melanoma patient number (N=13) and characteristics allow such sub - group analysis for initial assessment of anti - tumor activity • For other tumor types, appropriate patient numbers and characteristics have not yet been achieved All ovarian cancer patients were platinum - resistant IMA203 GEN1 Data cut - off Sep 30, 2023
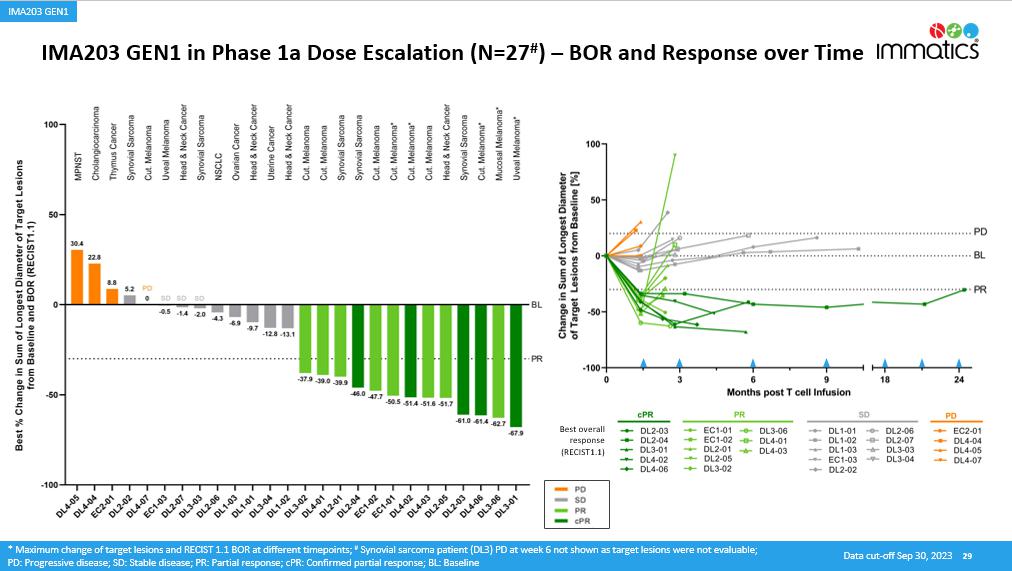
IMA203 GEN1 in Phase 1a Dose Escalation (N=27 # ) – BOR and Response over Time 29 * Maximum change of target lesions and RECIST 1.1 BOR at different timepoints ; # Synovial sarcoma patient (DL3) PD at week 6 not shown as t arget lesions were not evaluable; PD: Progressive disease; SD: Stable disease; PR: Partial response; cPR : Confirmed partial response; BL: Baseline Best overall response (RECIST1.1) IMA203 GEN1 Data cut - off Sep 30, 2023

* IMA203 GEN1 in Cohort A (N=18) – BOR and Response over Time Objective Responses across Multiple Solid Cancer T ypes 30 1 Patient received one dose nivolumab erroneously; 2 Progressive disease at month 6 due to unequivocal progression of non - target lesions, target lesions not evaluable due to externa l assessment ; Initial ORR: Objective response rate according to RECIST 1.1 at any post infusion scan; Confirmed ORR ( cORR ): Confirmed objective response rate according to RECIST 1.1 for patients with at least two available post infusion scans or pat ients with progressive disease (PD) at any prior timepoint, patients with ongoing unconfirmed PR not included in cORR calculation; Duration of response (DOR) in confirmed responders is defined as time from first documented response until disease progressio n/d eath. Patients with ongoing response will be censored at date of data cut - off. Median DOR is analyzed by using the Kaplan - Meier method; Median Follow - up is analyzed by using the reverse Kaplan - Meier method; PD: Progressive Disease; SD: Stable Disease; PR: Partial Response; cPR : Confirmed Partial Response; BL: Baseline; BOR: Best Overall Response; DOR: Duration of Response Data cut - off Sep 30, 2023 Median DOR, min, max DOR Not reached, 2.2+, 14.7+ months Median Follow - up 10.8 months Scans at approximately week 6, month 3 and then every 3 months Ongoing ORR 50% (9/18) cORR 47% (8/17) * Response until 5.7 months post infusion, target lesion response assessment not available (external assessment) IMA203 GEN1

31 Data cut - off Sep 30, 2023 IMA203 GEN1 in Cohort A – Most Frequent Adverse Events N=21 Patients in Safety Population 1 • Expected cytopenia (Grade 1 - 4) associated with lymphodepletion in all patients • Mild - moderate cytokine release syndrome (CRS) in 90% (19/21) of patients • 43% (9/21) with Grade 1 CRS • 48% (10/21) with Grade 2 CRS • No dose - dependent increase of CRS • O ne non - serious, mild (Grade 1) ICANS 2 in DL5 • No dose - limiting toxicity • No IMA203 - related deaths 1 Three cutaneous melanoma patients treated with IMA203, and pending post infusion scan included in safety population, but not ef ficacy population; 2 I CANS: Immune Effector Cell - Associated N eurotoxicity S yndrome ; CRS and ICANS graded by CARTOX criteria ( Neelapu et al ., 2018) IMA203 GEN1 monotherapy continues to be well tolerated at total doses between 1 - 10x10 9 TCR - T cells (RP2D) IMA203 GEN1

Adverse event ( System organ class , Preferred term ) ≥ Grade 3 No . % Patients with any adverse event 49 100.0 Adverse Events of Special Interest 2 4.1 Cytokine release syndrome 2 4.1 ICANS 2 0 0.0 Blood and lymphatic system disorders 48 98.0 Neutropenia 36 73.5 Lymphopenia 27 55.1 Leukopenia 26 53.1 Anaemia 24 49.0 Thrombocytopenia 17 34.7 Cytopenia 1 2.0 Leukocytosis 1 2.0 Lymphocytosis 1 2.0 Investigations 9 18.4 Neutrophil count decreased 4 8.2 Alanine aminotransferase increased 2 4.1 Aspartate aminotransferase increased 2 4.1 White blood cell count decreased 2 4.1 Blood alkaline phosphatase increased 1 2.0 Blood creatinine increased 1 2.0 Blood fibrinogen decreased 1 2.0 Infections and infestations 7 14.3 Appendicitis 1 2.0 COVID - 19 1 2.0 Enterococcal infection 1 2.0 Infection 1 2.0 Orchitis 1 2.0 Sepsis 4,5 1 2.0 Septic shock 4 1 2.0 Urinary tract infection 1 2.0 Respiratory, thoracic and mediastinal disorders 6 12.2 Hypoxia 3 6.1 Bronchial obstruction 1 2.0 Laryngeal inflammation 1 2.0 Pleural effusion 1 2.0 Respiratory failure 1 2.0 Vascular disorders 6 12.2 Hypertension 4 8.2 Hypotension 2 4.1 Adverse event ( System organ class , Preferred term ) ≥ Grade 3 No . % table continued… General disorders and administration site conditions 4 8.2 Condition aggravated 4 1 2.0 Fatigue 1 2.0 Pyrexia 1 2.0 Swelling face 1 2.0 Metabolism and nutrition disorders 4 8.2 Hypokalaemia 3 6.1 Failure to thrive 1 2.0 Hypophosphataemia 1 2.0 Gastrointestinal disorders 2 4.1 Abdominal pain 1 2.0 Diarrhoea 1 2.0 Vomiting 1 2.0 Injury, poisoning and procedural complications 2 4.1 Humerus fracture 1 2.0 Infusion related reaction 1 2.0 Renal and urinary disorders 2 4.1 Acute kidney injury 1 2.0 Proteinuria 1 2.0 Skin and subcutaneous tissue disorders 2 4.1 Rash maculo - papular 2 4.1 Cardiac disorders 1 2.0 Atrial fibrillation 3 1 2.0 Endocrine disorders 1 2.0 Inappropriate antidiuretic hormone secretion 1 2.0 Eye disorders 1 2.0 Ulcerative keratitis 1 2.0 Hepatobiliary disorders 1 2.0 Cholangitis 1 2.0 Immune system disorders 1 2.0 Contrast media allergy 1 2.0 Musculoskeletal and connective tissue disorders 1 2.0 Muscle spasms 1 2.0 Nervous system disorders 1 2.0 Headache 1 2.0 Reproductive system and breast disorders 1 2.0 Vaginal haemorrhage 1 2.0 Tolerability Data – IMA203 GEN1 across All Dose Levels Phase 1a Dose Escalation and Cohort A – All ≥Grade 3 Adverse Events (N=49) 32 • Well tolerated at doses as high as ~10x10 9 TCR - T cells • No AE ≥Grade 3 was observed with a frequency ≥10% when excluding expected cytopenia associated with lymphodepletion • No IMA203 - related Grade 5 Adverse Events All treatment - emergent adverse events (TEAEs) with ≥ Grade 3 regardless of relatedness to study treatment that occurred in at least 1 patient (except for ICANS, where only Grade 1 - 2 occurred ; listed for completeness due to being an adverse event of special interest) are presented . Adverse events were coded using the Medical Dictionary for Regulatory Activities . Grades were determined according to National Cancer Institute Common Terminology Criteria of Adverse Events, version 5 . 0 . Grades for CRS and ICANS were determined according to CARTOX criteria ( Neelapu et al . , 2018 ) . Patients are counted only once per adverse event and severity classification . Based on interim data extracted from open clinical database ( 30 - Sep - 2023 ) ; 1 Two patients with disease progression after first IMA 203 infusion received exploratory second IMA 203 infusion . They had these ≥ Grade 3 TEAEs only after second infusion, which are included in the table : First patient : Abdominal pain, Cytokine release syndrome, Diarrhoea , Hypokalaemia , Proteinuria ; Second patient : Humerus fracture, Muscle spasms, Neutropenia, Thrombocytopenia ; 2 ICANS : Immune effector cell - associated neurotoxicity syndrome ; 3 DLT : Dose limiting toxicity in phase 1 a at DL 2 reported on March 17 , 2021 ; 4 Fatal Adverse events were not considered related to any study drug ; 5 Patient died from sepsis of unknown origin and did not receive IMA 203 TCR - T cells . TEAEs by maximum severity for all patients in Phase 1a dose escalation and Cohort A dose expansion (N=49) 1 IMA203 GEN1 Data cut - off Sep 30, 2023

Tolerability Data – IMA203 GEN1 at RP2D Phase 1a DL4 and Cohort A – All ≥Grade 3 Adverse Events (N=28) 33 • IMA203 was well tolerated at doses as high as ~10x10 9 TCR - T cells • Most frequent ≥Grade 3 AEs were expected cytopenia associated with lymphodepletion • No IMA203 - related Grade 5 AEs All treatment - emergent adverse events (TEAEs) with ≥ Grade 3 regardless of relatedness to study treatment that occurred in at least 1 patient (except for ICANS, where only Grade 1 - 2 occurred ; listed for completeness due to being an adverse event of special interest) are presented . Adverse events were coded using the Medical Dictionary for Regulatory Activities . Grades were determined according to National Cancer Institute Common Terminology Criteria of Adverse Events, version 5 . 0 . Grades for CRS and ICANS were determined according to CARTOX criteria ( Neelapu et al . , 2018 ) . Patients are counted only once per adverse event and severity classification . Based on interim data extracted from open clinical database ( 30 - Sep - 2023 ) ; 1 One patient in Phase 1 a DL 4 with disease progression after first IMA 203 infusion received exploratory second IMA 203 infusion and had these ≥ Grade 3 TEAEs only after second infusion, which are included in the table : Humerus fracture, Muscle spasms, Neutropenia, Thrombocytopenia ; 2 ICANS : Immune effector cell - associated neurotoxicity syndrome ; 3 Fatal Adverse events were not considered related to any study drug Adverse event ( System organ class , Preferred term ) ≥ Grade 3 No . % Patients with any adverse event 28 100.0 Adverse Events of Special Interest 1 3.6 Cytokine release syndrome 1 3.6 ICANS 2 0 0.0 Blood and lymphatic system disorders 27 96.4 Neutropenia 18 64.3 Anaemia 14 50.0 Leukopenia 13 46.4 Lymphopenia 11 39.3 Thrombocytopenia 9 32.1 Leukocytosis 1 3.6 Lymphocytosis 1 3.6 Investigations 7 25.0 Neutrophil count decreased 4 14.3 Alanine aminotransferase increased 2 7.1 Aspartate aminotransferase increased 2 7.1 White blood cell count decreased 2 7.1 Blood alkaline phosphatase increased 1 3.6 Infections and infestations 3 10.7 Infection 1 3.6 Septic shock 3 1 3.6 Urinary tract infection 1 3.6 Respiratory, thoracic and mediastinal disorders 3 10.7 Hypoxia 2 7.1 Laryngeal inflammation 1 3.6 Vascular disorders 3 10.7 Hypotension 2 7.1 Hypertension 1 3.6 Metabolism and nutrition disorders 2 7.1 Failure to thrive 1 3.6 Hypokalaemia 1 3.6 Hypophosphataemia 1 3.6 Eye disorders 1 3.6 Ulcerative keratitis 1 3.6 Adverse event ( System organ class , Preferred term ) ≥ Grade 3 No . % table continued… General disorders and administration site conditions 1 3.6 Pyrexia 1 3.6 Hepatobiliary disorders 1 3.6 Cholangitis 1 3.6 Injury, poisoning and procedural complications 1 3.6 Humerus fracture 1 3.6 Musculoskeletal and connective tissue disorders 1 3.6 Muscle spasms 1 3.6 Nervous system disorders 1 3.6 Headache 1 3.6 Skin and subcutaneous tissue disorders 1 3.6 Rash maculo - papular 1 3.6 TEAEs by maximum severity for all patients in Ph1a dose escalation DL4 and Ph1b Cohort A dose expansion ( RP2D, N=28) 1 Data cut - off Sep 30, 2023 IMA203 GEN1

Biological Data Consistent with Clinical Data – IMA203 GEN1 IMA203 T cell Levels and Tumor Infiltration across Patients in Phase 1a and Cohort A 34 Data cut - off Sep 30, 2023 Mann - Whitney U test; 1 T cell infiltration for 22 patients (11 non - responder, 11 responder) with 6 - week post infusion biopsy available (1 patient with ~4 - week, 3 patients with ~13 - week post infusion biopsy); PD: Progressive Disease; SD: Stable Disease; PR: Partial Response; cPR : Confirmed Partial R esponse Persistence over time Peak expansion ( C max ) 2 6 1 0 1 4 1 8 1×10 -1 1×10 0 1×10 1 1×10 2 1×10 3 1×10 4 1×10 5 1×10 6 1×10 7 2 0 6 0 1 0 0 1 4 0 1 8 0 2 0 0 4 0 0 6 0 0 8 0 0 1 0 0 0 Days post infusion V e c t o r c o p i e s / μ g g D N A Phase 1A (n=27) Cohort A (n=18) Tumor Infiltration IMA203 T cells found in all evaluable tumor tissues, level of infiltration associated with objective responses 1 Increased levels of IMA203 T cells in the blood of patients in Cohort A following increase of cell dose and switch to T cell enrichment process Phase 1A Cohort A 0 5×10 5 1×10 6 1.5×10 6 2×10 6 2.5×10 6 V e c t o r c o p i e s / μ g g D N A PR cPR PD/SD (n=27) (n=18) p<0.0001 n=45 IMA203 GEN1

Melanoma Patients – Phase 1a and Cohort A IMA203 GEN1 (N=13) Cohort Patient ID Indication No of prior treatment lines Prior treatments Total infused dose TCR - T cells 1 [x10 9 ] BOR BOR (Max % change of target lesions) Comment Reason for Progression Cohort A A - DL5 - 01 Uveal Melanoma 1 ARRY614 + Nivolumab 4.16 cPR - 69.4 Ongoing response 16.0 months post infusion Cohort A A - DL4 - 03 Cut. Melanoma 7 Dabrafenib + Trametinib Pembrolizumab Dabrafenib + Trametinib Vemurafenib + Cobimetinib Dabrafenib + Trametinib Tebentafusp Encorafenib + Binimetinib 1.30 cPR - 78.3 Ongoing response 15.8 months post infusion Cohort A A - DL5 - 03 Cut. Melanoma 3 Interferon Pembrolizumab Ipilimumab + Nivolumab 5.12 cPR - 65.1 Ongoing response 12.2 months post infusion Cohort A A - DL5 - 10 Uveal Melanoma 1 SEAGEN CD40 Agonist 2.68 cPR - 40.8 Ongoing response 3.4 months post infusion Phase 1a DL4 - 02 Cut. Melanoma 5 Dabrafenib + Trametinib Ipilimumab + Nivolumab Nivolumab Ipilimumab + Nivolumab Vemurafenib + Cobimetinib 1.07 cPR - 51.4 Response until 4.4 months post infusion New lesions, progressing non - target lesions Phase 1a DL4 - 06 Cut. Melanoma 4 Pembrolizumab Pembrolizumab Ipilimumab + Nivolumab Nivolumab 1.21 cPR - 61.4 Response until 3.7 months post infusion New lesions Phase 1a DL4 - 01 Cut. Melanoma 7 Interferon NY - ESO - 1, Tyrosinase, MAGE - A3. TPTE, LIP - Merit - study (experimental therapy) Nivolumab Pembrolizumab Ipilimumab + Nivolumab Decortin + Infiliximab Nivolumab + Ipilimumab + Mekinist + Infiliximab 1.16 PR - 39.0 Unconfirmed response until 2.8 months post infusion New lesions, progressing target lesions Phase 1a DL4 - 03 Cut. Melanoma 7 Vemurafenib + Cobimetinib Nivolumab Dabrafenib + Trametinib Ipilimumab + Nivolumab Encorafenib + Binimetinib Pembrolizumab Encorafenib + Binimetinib 1.72 PR - 51.6 Unconfirmed response until 2.4 months post infusion Progressing target lesions Cohort A A - DL4 - 04 Melanoma (Unk. Primary) 2 Ipilimumab + Nivolumab Nivolumab 1.73 SD 0.0 Disease stabilization until 5.7 months post infusion Non - target lesion progression and a new lesion Cohort A A - DL4 - 05 Cut. Melanoma 5 Nivolumab Nivolumab (re - exposure) Nivolumab + Ipilimumab Dabrafenib + Trametinib Nivolumab 1.63 SD 11.4 Disease stabilization until 5.8 months post infusion New lesions, target lesion progression Cohort A A - DL5 - 12 Uveal Melanoma 3 Tyrosinase peptides Nivolumab + Ipilimumab + Denosumab Tebentafusp 4.50 SD - 22.6 Ongoing disease stabilization 2.2 months post infusion Phase 1a DL4 - 07 Cut. Melanoma 6 Interferon alpha Pembrolizumab Ipilimumab + Nivolumab Nivolumab LXH254 + Ribociclib DKY709 Helios 2.09 PD 0.0 Progressive disease 1.4 months post infusion New lesions, progressing non - target lesions Cohort A A - DL4 - 06 Uveal Melanoma 0 NA 2.56 PD - 6.3 Progressive disease 1.3 months post infusion New target lesion 35 1 Transduced viable CD8 T cells; PD: Progressive Disease; Efficacy population shown ( Patients with at least one available tumor response assessment post infusion) ; SD: Stable Disease; PR: Partial Response; cPR : Confirmed Partial Response; BL: Baseline; BOR: Best Overall Response Data cut - off Sep 30, 2023 IMA203 GEN1

Indications beyond Melanoma – Cohort A IMA203 GEN1 (N=10) 36 Patient ID Indication No of prior treatment lines Prior treatments Total infused dose TCR - T cells 1 [x10 9 ] BOR BOR (Max % change of target lesions) Comment Reason for Progression A - DL4 - 01 Head & Neck Cancer 1 Paclitaxel + Carboplatin 1.92 cPR - 33.3 Response until 5.7 months post infusion Non - target lesion progression A - DL5 - 07 Synovial Sarcoma 2 Melphalan + TNF alpha Doxorubicin + Ifosphamid 6.01 cPR - 44.3 Ongoing response 4.4 months post infusion A - DL5 - 05 Ovarian Cancer 3 Adriamycin + Cytoxan + Taxol Carboplatin + Taxol Carboplatin + Doxil 8.84 cPR - 61.7 Response until 4.4 months post infusion New lesions, target and non - target lesion progression A - DL4 - 02 Ovarian Cancer 10 Carboplatin + Taxol Taxol Gemcitabine + Carboplatin Olaparib Letrozole Rubaparib UPCC 03118 Bevacizumab + Cyclophosphamide Carboplatin Doxorubicin 1.97 cPR - 41.0 Response until 3.8 months post infusion Non - target lesion progression A - DL5 - 06 Synovial Sarcoma 1 Adriamycin + Ifosfamide + Trabectedin 3.94 PR - 74.8 Response until 2.8 months post infusion Target and non - target lesion progression A - DL5 - 08 Small Cell Lung Cancer (SCLC) 4 Cisplatin + Etoposid Carboplatin + Etoposid+ Atelizumab Topotecan Paclitaxel 5.09 SD - 1.8 Disease stabilization until 3.0 months post infusion New lesions, target lesion progression A - DL5 - 02 Pancreatic NET 3 Lanreotid Streptozocin + 5 - Fluorouracil Everolismus 5.12 SD - 21.8 Disease stabilization until 2.3 months post infusion Non - target lesion progression A - DL5 - 04* Ovarian Cancer 5 Paclitaxel + Carboplatin Niraparib Doxorubicin + Liposomal + Carboplatin 2020 - 0808 ZN - C3 + Gemcitabine 2020 - 0755 COM 701 + BMS - 986207 + Nivolumab 4.68 PD 50.8 Progressive disease at 1.2 months post infusion New lesions, target - and non - target lesion progression A - DL5 - 09 Ovarian Cancer 4 Paclitaxel + Carboplatin Bevacizumab Doxurubicin + Carboplatin AVB - 001 Cell infusion 6.36 PD - 2.4 Progressive disease at 1.5 months post infusion New target lesion A - DL5 - 11 Synovial Sarcoma 5 Adriamycin + Isofamide Pazobanib NY - ESO1 - TCR T - Cells Pazobanib BRD9 PROTAC CFT8634 9.36 SD - 26.4 Clinical progression 2.0 months post infusion Clinical progression 1 Transduced viable CD8 T cells; PD: Progressive Disease; * Ovarian cancer patient A - DL5 - 04 erroneously received one dose of nivolumab and is part of intent - to - treat population (shown here) but not per - protocol population. SD: Stable Disease; PR: Partial Response; cPR : Confirmed Partial Response; BL: Baseline; BOR: Best Overall Response Data cut - off Sep 30, 2023 IMA203 GEN1

Appendix – Additional Data 1. Patient Flow and PRAME Expression in Pre - Treatment Tumor Biopsies 2. Dose Escalation and Cohort A IMA203 GEN1 3. Cohort B IMA203 GEN1 + Nivolumab 4. Cohort C IMA203 GEN2 5. Manufacturing and in vivo Engraftment Data IMA203 GEN1 and IMA203CD8 GEN2

Cohort B: ACTengine® IMA203 TCR - T + Nivolumab Summary • IMA203 TCR - T combined with nivolumab was well tolerated with no unexpected adverse events or additive toxicities • The combination therapy showed clinical activity with one durable objective response exceeding 12 months post infusion and tumor shrinkage in 4 of 6 evaluable patients • No synergistic anti - tumor effects were observed: • Clinical activity in combination cohort was lower compared to IMA203 monotherapy (Cohort A), but comparison is confounded by more unfavorable patient characteristics and lower applied median cell dose in IMA203 + nivolumab combination cohort • Trend towards lower T cell infiltration as well as increased terminal differentiation and signs of exhaustion of IMA203 T cel ls in combination with nivolumab • Data set is too small and heterogenous to draw firm conclusions • Patient case study could indicate potential for clinical benefit of IMA203 TCR - T treatment in combination with checkpoint inhibitors in patients with PD - 1/PD - L1 upregulation » IMA203 in combination with nivolumab deprioritized due to • high monotherapy activity in Cohort A IMA203 and Cohort C IMA203CD8 • lack of synergistic anti - tumor effects 38 Analysis of per - protocol population treated with IMA203 + nivolumab Data cut - off Sep 30, 2023 IMA203 + Nivo

Patient Flow – Cohort B IMA203 + Nivolumab 39 HLA - A*02 Testing Blood sample; Central lab Treatment & Observation Phase Long Term Follow - up Screening & Manufacturing Phase Manufacturing by Immatics Infusion of ACTengine® IMA203 TCR - T Product Lymphodepletion * Target Profiling IMADetect ® Biopsy or archived tissue Low dose IL - 2 ** Safety and efficacy monitoring for 12 months Leukapheresis x x Expression Antigen 1 3 2 Short process time of 14 days * 30 mg/m 2 Flu darabine and 500 mg/m 2 Cy clophosphamide for 4 days; ** 1m IU daily days 1 - 5 and twice daily days 6 - 10; ***Nivolumab at Day 14, or Day 21 post IMA203 infusion. Two weeks after the first infusion of nivolumab and thereafter approximately every 4 weeks, patients receive nivolumab for up to 1 year 7 - day manufacturing process 7 - day QC release testing Nivolumab*** IMA203 + Nivo

PRAME Expression in Pre - Treatment Tumor Biopsies Comparable PRAME Expression Levels in Patients Treated in Cohort A and B 40 Data cut - off Sep 30, 2023 PRAME RNA expression in pre - treatment biopsies relative to threshold Immatics’ mass spectrometry - guided mRNA threshold IMA203 + Nivo Mann - Whitney U test

Patient Characteristics Dose Escalation vs. Cohort A IMA203 vs. Cohort B IMA203 + Nivolumab 41 • Heavily pre - treated, metastatic last - line patients that have exhausted all available SOC treatments • Patients in IMA203+Nivo cohort had more prior lines of treatment and higher tumor burden while receiving lower cell numbers compared to IMA203 monotherapy cohort (i.e. lower E:T ratio in IMA203+Nivo cohort) 1 *Efficacy population in Phase 1a and Cohort A: patients with at least one available tumor response assessment post infusion ; **Efficacy per - protocol population Cohort B: patients received IMA203 + nivolumab and have at least one available tumor response assessment post infusion or reported clinical PD; 1 Demonstrated to be associated with durable response: Locke et al. 2020 Blood Advances Phase 1a Dose Escalation Phase 1b Dose Expansion All pts* Cohort A IMA203 * Cohort B IMA203+Nivo ** Patients treated 27 18 6 Age Median (min, max) 55.0 (18, 72) 52.5 (31, 79) 51.5 (38, 63) Prior lines of treatment Median (min, max) 4.0 (1,8) 3.0 (0, 10) 5.5 (0, 8) LDH at baseline >1 x ULN [% of patients] 66.7 50.0 66.7 Baseline tumor burden Target lesion sum of diameter [mm] Median (min, max) 133.0 (29.0, 219.7) 58.9 (21.0, 207.3) 117.3 (37.0, 280.2) Dose Level DL1 - 4 DL4/5 DL4 Total infused dose Median transduced viable CD8 T cells infused [x10 9 ] (min, max) 0.41 (0.08, 2.09) 4.33 (1.30, 9.36) 2.24 (0.66, 2.71) Data cut - off Sep 30, 2023 IMA203 + Nivo

Most Frequent Adverse Events – Cohort B IMA203 + Nivolumab (N=7) 1 Manageable Treatment - Emergent Adverse Events (TEAEs) • Expected cytopenia (Grade 1 - 4) associated with lymphodepletion in all patients • Low - moderate (Grade 1 - 2) cytokine release syndrome (CRS) in 100% (7/7) of patients • 57% (4/7) of patients had Grade 1 CRS • 43% (3/7) of patients had Grade 2 CRS • Low - grade ICANS 2 in 14% (1/7) of patients • No events indicating immune - mediated adverse reactions in association with nivolumab • No hints that combination with nivolumab increased number or severity of observed TEAEs 42 1 One patient treated with IMA203 + nivolumab withdrew consent 1.1 months post infusion (prior to first scan) and is included s afe ty per - protocol population, but not efficacy per - protocol population; 2 I CANS: Immune Effector Cell - Associated Neurotoxicity Syndrome; CRS and ICANS graded by CARTOX criteria ( Neelapu et al ., 2018) IMA203 TCR - T in combination with nivolumab was well tolerated, no unexpected or additive toxicities compared to IMA203 TCR - T monotherapy Data cut - off Sep 30, 2023 IMA203 + Nivo

Detailed Tolerability Data – Cohort B IMA203 + Nivolumab (N=7) 1 All ≥Grade 3 Adverse Events (N=7) 43 Adverse event ≥ Grade 3 ( System organ class , preferred term) No. % Patients with any adverse event 7 100.0 Adverse events of special interest 0 0.0 Cytokine release syndrome 0 0.0 Immune effector cell - associated neurotoxicity syndrome 0 0.0 Blood and lymphatic system disorders 7 100.0 Neutropenia 7 100.0 Anaemia 6 85.7 Lymphopenia 6 85.7 Thrombocytopenia 3 42.9 Leukopenia 2 28.6 Febrile neutropenia 1 14.3 General disorders and administration site conditions 2 28.6 Pyrexia 2 28.6 Investigations 1 14.8 Aspartate aminotransferase increased 1 14.3 TEAEs by maximum severity for all patients in Cohort B IMA203 + Nivolumab (N=7) All treatment - emergent adverse events (TEAEs) with ≥ Grade 3 regardless of relatedness to study treatment that occurred in at least 1 patient (except for ICANS and CRS, where only lower grades occurred ; listed for completeness due to being adverse events of special interest) are presented . Adverse events were coded using the Medical Dictionary for Regulatory Activities . Grades were determined according to National Cancer Institute Common Terminology Criteria of Adverse Events, version 5 . 0 . Grades for CRS and ICANS were determined according to CARTOX criteria ( Neelapu et al . , 2018 ) . Patients are counted only once per adverse event and severity classification . Based on interim data extracted from open clinical database ( 30 - Sep - 2023 ) • IMA203 TCR - T in combination with nivolumab was well tolerated • No unexpected or additive toxicities compared to IMA203 TCR - T monotherapy • Most frequent ≥Grade 3 AEs were expected cytopenia associated with lymphodepletion • No IMA203 - related Grade 5 AEs 1 One patient treated with IMA203 + nivolumab withdrew consent 1.1 months post infusion (prior to first scan) and is included s afe ty per - protocol population, but not efficacy per - protocol population; Data cut - off Sep 30, 2023 IMA203 + Nivo

Best Overall Response & Durability – Cohort B IMA203 + Nivolumab (N=6) Ongoing Durable Response 12+ Months post Treatment 44 1 Initial ORR: Objective response rate according to RECIST 1.1 at any post infusion scan; 2 Confirmed ORR ( cORR ): Confirmed objective response rate according to RECIST 1.1 for patients with at least two available post infusion scans or patients with progressive disease (PD) at any prior timepoint, patients with ongoing unconfi rme d PR not included in cORR calculation; PD: Progressive Disease; SD: Stable Disease; PR: Partial Response; cPR : Confirmed Partial Response; BL: Baseline; BOR: Best Overall Response; CPI: Checkpoint Inhibitor . * Maximum change of target lesions at time of tumor progression. ORR 1 33% (2/6) cORR 2 17% (1/6) Data cut - off Sep 30, 2023 Pt B - DL 4 - 05 not shown due to clinical progression prior to 1 st post infusion scan, response assessment not available, considered as non - responder for ORR and cORR • Tumor shrinkage in 4 of 6 patients • Ongoing long - term durable response 12+ months post treatment in melanoma patient • All cut. melanoma patients were CPI - refractory • Tumor burden of patient B - DL4 - 04 was among the highest we ever treated with tumor regression in multiple lesions observed (see patient case) • Patient B - DL4 - 07 with significant reduction of target lesions but progression of non - target lesion in the brain, thus PD in BOR analysis Scans at approximately week 6, month 3 and then every 6 months Ongoing IMA203 + Nivo

Particularly Hard - to - Treat Patient Population – Cohort B IMA203 + Nivolumab 45 Patient ID Indication No of prior treatment lines Prior treatments Total infused dose TCR - T cells [x10 9 ] BOR BOR (Max % change of target lesions) Comment Reason for Progression B - DL4 - 06 Uveal Melanoma 0 NA 2.22 cPR - 81.2 Ongoing response 12 months post infusion On trial B - DL4 - 04 Melanoma (Unk. Primary) 6 Nivolumab/NKTR - 214, N ivolumab/Ipilimumab, Encorafenib/Binimetinib, CLXH254C12210 (Panrafi+ERKI) Encorafenib/Binimetinib/Pembrolizumab, Carboplatin/Paclitaxel 2.42 PR - 35.6 Unconfirmed response until 2.6 months post infusion Unequivocal progression of non - target lesion in the adrenal gland B - DL4 - 01 Cut. Melanoma 6 Dabrafenib/Trametinib, Nivolumab/Ipilimumab, Nivolumab Encorafenib / Binimetinib Nivolumab/Ipilimumab, Nivolumab 2.17 SD - 13.3* Disease stabilization until 2.7 months post infusion Unequivocal progression of non - target lesion in the lung and new lung lesion B - DL4 - 03 Thymus cancer 2 Carboplatin/Paclitaxel, Doxorubicin/Cisplatin/Cyclophosphamide 0.66 SD 5.5 Disease stabilization until 3.0 months post infusion Target Lesion progression B - DL4 - 07 Cut. Melanoma 5 Pembrolizumab, Dabrafenib/Trametinib, Nivolumab/Ipilimumab, Nivolumab, Encorafinib/Binimetinib 2.71 PD - 48.6* Progressive disease at 1.4 months post infusion Unequivocal progression of non - target lesion in the brain B - DL4 - 05 Rhabdomyosarcoma 8 Adriamycine/Ifosfamide/Vincristine, Ifosfamide/Doxorubicin, Ifosfamide/Doxorubicin, Etoposide/Topotecan/Carboplatin/Cyclophosphamide Trofosfamide/Etoposide/Idarubicine Doxorubicin/Ifosfamide, Carboplatin/Topotecan, Vincristine 2.25 PD NA Clinical progression at 0.9 months post infusion (prior to first scan) Clinical progression (persistent rise in LDH, growing lymph node) B - DL4 - 02 Fibrosarcoma 5 Vincristin / Ifosfamid /Doxorubicin, Epirubicin / Ifosfamid , Gemcitabin /Docetaxel, Pazopanib, Trabectedin 1.07 NA NA Withdrawal of consent 1.1 months post infusion (prior to first scan); safety population NA * Maximum change of target lesions at time of tumor progression. Patient case Data cut - off Sep 30, 2023 IMA203 + Nivo

IMA203 T cell Levels – Molecular Immunomonitoring Cohort A IMA203 vs. Cohort B IMA203 + Nivolumab 46 Statistical test: Mann - Whitney U 2 6 1 0 1 4 1 8 1×10 -1 1×10 0 1×10 1 1×10 2 1×10 3 1×10 4 1×10 5 1×10 6 1×10 7 2 0 4 0 6 0 8 0 1 0 0 2 0 0 4 0 0 6 0 0 8 0 0 Days post infusion V e c t o r c o p i e s / μ g g D N A Cohort A (n=18) Cohort B (n=6) Cohort A Cohort B 0 5×10 5 1×10 6 1.5×10 6 2×10 6 2.5×10 6 V e c t o r c o p i e s / μ g g D N A p=0.0472 PR cPR PD SD (n=18) (n=6) Peak expansion (C max ) normalized to cell dose Comparable cell dose - dependent engraftment and peripheral blood kinetics of IMA203 T cells in Cohort A and C while lower tumor infiltration in combination with nivolumab Persistence over time Peak expansion (C max ) Tumor infiltration Cohort A Cohort B 1×10 0 1×10 1 1×10 2 1×10 3 1×10 4 1×10 5 I M A 2 0 3 T c e l l i n f i l t r a t i o n [ v e c t o r c o p i e s / µ g g D N A ] PR cPR SD (n=4) (n=4) p=0.0286 Cohort A Cohort B 0 2×10 5 4×10 5 6×10 5 8×10 5 V e c t o r c o p i e s / μ g g D N A p=0.6261 PR cPR PD SD (n=18) (n=6) Data cut - off Sep 30, 2023 IMA203 + Nivo

IMA203 T cell Activation and Differentiation Cohort A IMA203 vs. Cohort B IMA203 + Nivolumab 47 Trend towards increased terminal differentiation of IMA203 T cells and exhaustion surrogate receptor expression in combination with nivolumab Statistical Test: Mann Whitney; *TEMRA (CCR7 - CD45RA+), CD39 - CD69 - , and TIM - 3: for patients B - DL4 - 05, A - DL5 - 04, A - DL5 - 09, A - DL5 - 10, and A - DL5 - 12 data not available for week 8 TEMRA * Terminal differentiation CD39 - CD69 - Stem - like phenotype TIM - 3 Exhaustion surrogate receptor Data cut - off Sep 30, 2023 Cohort A: n=18 Cohort B: n=6 IMA203 + Nivo

Kinetics of PD - 1 + Frequency on IMA203 T Cells 48 Cohort A IMA203 vs. Cohort B IMA203 + Nivolumab Sustained PD - 1 expression on IMA203 T cells after initial activation observed in few patients *Patient B - DL4 - 04 did not have available samples for analysis of week 1 and month 6 Cohort A Cohort B Cohort A: n=18 Cohort B: n=6 Data cut - off Sep 30, 2023 IMA203 + Nivo

Patient Case B - DL4 - 04: Tumor Reduction in Multiple Large Metastatic Lesions Observed Sustained Clinical Benefit in Patient despite PD at Week 11 49 Pre - treatment Post - treatment, week 11 = bladder 1 Per treating physician; CT scans courtesy of treating physician Clinical benefit observed despite formally being a patient with early PD after unconfirmed PR according to RECIST 1.1 50 - year - old male patient with h ighly refractory malignant melanoma (unknown primary, BRAFV600E mutation) and lesions in multiple organs entering IMA203 Cohort B • 6 prior lines of systemic therapies, LDH at baseline 2.9 xULN • 5 target lesions (liver, lung, left adrenal gland, 2 lymph nodes) • 280.2 mm target lesion sum among the patients with highest tumor burden we have treated so far • 4 non - target lesions (liver, lung, right adrenal gland, large pelvic tumor bulk) » Tumor regression in multiple lesions after IMA203 + nivolumab treatment, pelvic tumor bulk reduced from 11.5 cm to ~3.5 cm 1 » Treatment provided sustained improvement of tumor - related symptoms 1 » Patient was PD (pararenal metastases) at week 11 and switched to pembrolizumab + lenvatinib treatment 1 . As of data cut off patient is still alive ~13 months post IMA203 + nivolumab treatment 1 » Patient case study could indicate potential clinical benefit of IMA203 + checkpoint inhibitors in patients with PD - 1/PD - L1 upregulation Liver lesion ( target ) Pelvic lesion (non - target) Large pelvic lesion compressing the bladder and colon prior to treatment Data cut - off Sep 30, 2023 IMA203 + Nivo

Appendix – Additional Data 1. Patient Flow and PRAME Expression in Pre - Treatment Tumor Biopsies 2. Dose Escalation and Cohort A IMA203 GEN1 3. Cohort B IMA203 GEN1 + Nivolumab 4. Cohort C IMA203 GEN2 5. Manufacturing and in vivo Engraftment Data IMA203 GEN1 and IMA203CD8 GEN2

Tolerability Data – Cohort C IMA203CD8 GEN2 51 Adverse event ≥ Grade 3 ( System organ class , preferred term) No. % Patients with any adverse event 12 100.0 Adverse events of special interest 3 25.0 Cytokine release syndrome 1 3 25.0 Immune effector cell - associated neurotoxicity syndrome 0 0.0 Blood and lymphatic system disorders 11 91.7 Neutropenia 9 75.0 Anaemia 8 66.7 Lymphopenia 8 66.7 Thrombocytopenia 4 33.3 Leukopenia 2 16.7 Investigations 4 33.3 Aspartate aminotransferase increased 2 16.7 Neutrophil count decreased 2 16.7 Alanine aminotransferase increased 1 8.3 Blood alkaline phosphatase increased 1 8.3 Blood bilirubin increased 1 8.3 Gamma - glutamyltransferase increased 1 8.3 Metabolism and nutrition disorders 2 16.7 Hypermagnesaemia 1 8.3 Hypoalbuminaemia 1 8.3 Hypophosphataemia 1 8.3 Nervous system disorders 2 16.7 Neurotoxicity 2 1 8.3 Syncope 1 8.3 Immune system disorders 1 8.3 Haemophagocytic lymphohistiocytosis 2 1 8.3 Infections and infestations 1 8.3 Infection 1 8.3 All treatment - emergent adverse events (TEAEs) with ≥ Grade 3 regardless of relatedness to study treatment that occurred in at least 1 patient ( except for ICANS, where no event was documented; listed for completeness due to being an adverse event of special interest) are presented. Adverse events were coded using the Medical Dictionary for Regulatory Activities. Grades were determined according to National Cancer Institute Common Terminology Criteria of Adverse Events, version 5.0. Grades for CRS and ICANS were determined according to CARTOX criteria ( Neelapu et al., 2018). Patients are counted only once per adverse event and severity classification. Based on interim data extracted from open clinical database (30 - Sep - 2023) ; 1 DLT: Dose limiting toxicity in patient DL4b - 04. 2 DLTs in patient DL4b - 01 All ≥Grade 3 Adverse Events (N=12) TEAEs by maximum severity for all patients in Cohort C (N= 12 ) • Manageable tolerability • Most frequent ≥Grade 3 AEs were expected cytopenia associated with lymphodepletion • No IMA203CD8 - related Grade 5 Adverse Events • Dose escalation ongoing IMA203CD8 GEN2 Data cut - off Sep 30, 2023

Patients Treated in Cohort C IMA203CD8 52 Patient ID Indication No of prior treatment lines Prior treatments Total infused dose TCR - T cells 1 [x10 9 ] BOR BOR (Max % change of target lesions) Comment Reason for Progression C - DL3 - 02 Cut. Melanoma 3 Ipilimumab + Nivolumab Nivolumab Binimetinib 0.93 cPR - 74.4 Ongoing response 12.8 months post infusion C - DL4a - 01 Uveal Melanoma 4 Transarterial chemo - embolization right liver Ipilimumab + Nivolumab Pembrolizumab Tebentafusp 0.94 cPR - 45.0 Ongoing response (after initial SD) 7.8 months post infusion C - DL4a - 02 Cut. Melanoma 3 Interferon Pembrolizumab Ipilimumab + Nivolumab 1.07 cPR - 62.3 Ongoing response 5.3 months post infusion C - DL3 - 04 Synovial Sarcoma 3 Adriamycin + Ifosfamide Doxorubicin + Dacarbazine Pazopanib 1.00 cPR - 42.2 Response until 4.9 months post infusion 2 New lesions, target and non - target lesion progression 2 C - DL4b - 02 Cut. Melanoma 3 Pembrolizumab Ipilimumab + Nivolumab Nivolumab 1.78 cPR - 36.0 Ongoing response 3.4 months post infusion C - DL4a - 03 Synovial Sarcoma 2 Doxorubicin Ifosfamid 1.56 PR - 36.7 Ongoing unconfirmed response (after initial SD) 4.8 months post infusion C - DL4b - 04 Synovial Sarcoma 1 Doxorubicin + Ifosfamide + Mesna 2.05 PR - 54.5 Ongoing unconfirmed response 2.4 months post infusion C - DL3 - 01 Synovial Sarcoma 5 Doxorubicin + Ifosfamid Doxorubicin + Ifosfamid Doxorubicin Trabectedin Ifosfamid 0.89 SD - 1.1 Disease stabilization until 2.8 months post infusion New lesions, target and non - target lesion progression C - DL3 - 03 Cut. Melanoma 3 Ipilimumab + Nivolumab Dabrafenib + Trametinib Pembrolizumab + Dabrafenib + Trametinib 0.64 SD - 36.7 Disease stabilization until 2.8 months post infusion New target lesion C - DL4b - 01 Cut. Melanoma 4 CMP - 100 + Nivolumab Encorafenib + Binimetinib Ipilimumab + Nivolumab Encorafenib + Binimetinib 1.89 SD - 7.6 Disease stabilization until 2.2 months post infusion Non - target lesion progression C - DL4b - 03 Synovial Sarcoma 3 Doxorubicin + Ifosfamide Votrient Pazopanib 1.49 SD - 23.5 Ongoing disease stabilization 2.9 months post infusion C - DL4a - 04 Uterine Cancer 2 Carboplatin + Paclitaxel Pembrolizumab + Lenvatinib 1.27 PD NA Progressive disease 1.7 months post infusion New lesions, target and non - target lesion progression 1 Transduced viable CD8 T cells; 2 I nvestigator information; PD: Progressive Disease; SD: Stable Disease; PR: Partial Response; cPR : Confirmed Partial Response; BL: Baseline; BOR: Best Overall Response Data cut - off Sep 30, 2023 IMA203CD8 GEN2

Appendix – Additional Data 1. Patient Flow and PRAME Expression in Pre - Treatment Tumor Biopsies 2. Dose Escalation and Cohort A IMA203GEN1 3. Cohort B IMA203 GEN1 + Nivolumab 4. Cohort C IMA203 GEN2 5. Manufacturing and in vivo Engraftment Data IMA203 GEN1 and IMA203CD8 GEN2

Favorable TCR - T Product Characteristics and High TCR - T Levels in Patients Manufacturing Improvements Implemented in Phase 1b Enhance Key Features of the Cell Product 54 Increased peak IMA203 T cell levels in patients Robust TCR - T product features DL4 only, normalized to cell dose Data cut - off Sep 30 , 2023 *Current: T cell enrichment process using monocyte depletion (negative selection) or CD8/CD4 positive selection; prior: manuf act uring process without specific T cell enrichment Current manufacturing success rate of >95% to reach RP2D of 1 - 10x10 9 TCR - T cells for IMA203 0 1×10 6 2×10 6 3×10 6 V e c t o r c o p i e s / μ g g D N A p<0.0001 IMA203 GEN1 current (n=19) IMA203 GEN1 prior (n=26) IMA203CD8 GEN2 current (n=12) 0 20 40 60 80 100 % T C R + ( o f C D 3 + C D 8 + c e l l s ) p<0.0001 IMA203 GEN1 prior (n=26) IMA203 GEN1 current (n=22) IMA203CD8 GEN2 current (n=12) 0 20 40 60 80 100 % C D 8 + ( o f v i a b l e C D 3 + c e l l s ) p=0.0382 IMA203 GEN1 prior (n=26) IMA203 GEN1 current (n=22) IMA203CD8 GEN2 current (n=12) Manufacturing process * IMA203 GEN1 IMA203CD8 GEN2

Delivering s the Power of T cells to Cancer Patients © Immatics. Not for further reproduction or distribution. www.immatics.com
Exhibit 99.3

© Immatics. Not for further reproduction or distribution. Delivering the Power of T cells to Cancer Patients © Immatics. Not for further reproduction or distribution. Immatics Corporate Presentation November 08, 2023

Forward - Looking Statement This presentation (“Presentation”) is provided by Immatics N . V . (“Immatics” or the “Company”) for informational purposes only . The information contained herein does not purport to be all - inclusive and none of Immatics, any of its affiliates, any of its or their respective control persons, officers, directors, employees or representatives makes any representation or warranty, express or implied, as to the accuracy, completeness or reliability of the information contained in this Presentation . Forward - Looking Statements . Certain statements in this presentation may be considered forward - looking statements . Forward - looking statements generally relate to future events or the Company’s future financial or operating performance . For example, statements concerning timing of data read - outs for product candidates, the timing and outcome of clinical trials, the nature of clinical trials (including whether such clinical trials will be registration - enabling), the timing of IND or CTA filing for pre - clinical stage product candidates, estimated market opportunities of product candidates, the Company’s focus on partnerships to advance its strategy, and other metrics are forward - looking statements . In some cases, you can identify forward - looking statements by terminology such as “may”, “should”, “expect”, “plan”, “target”, “intend”, “will”, “estimate”, “anticipate”, “believe”, “predict”, “potential” or “continue”, or the negatives of these terms or variations of them or similar terminology . Such forward - looking statements are subject to risks, uncertainties, and other factors which could cause actual results to differ materially from those expressed or implied by such forward looking statements . These forward - looking statements are based upon estimates and assumptions that, while considered reasonable, Immatics and its management, are inherently uncertain . New risks and uncertainties may emerge from time to time, and it is not possible to predict all risks and uncertainties . Factors that may cause actual results to differ materially from current expectations include, but are not limited to, various factors beyond management's control including general economic conditions and other risks, uncertainties and factors set forth in the Company’s Annual report on Form 20 - F and other filings with the Securities and Exchange Commission (SEC) . Nothing in this presentation should be regarded as a representation by any person that the forward - looking statements set forth herein will be achieved or that any of the contemplated results of such forward - looking statements will be achieved . You should not place undue reliance on forward - looking statements, which speak only as of the date they are made . The Company undertakes no duty to update these forward - looking statements . No Offer or Solicitation . This communication is for informational purposes only and does not constitute, or form a part of, an offer to sell or the solicitation of an offer to sell or an offer to buy or the solicitation of an offer to buy any securities, and there shall be no sale of securities, in any jurisdiction in which such offer, solicitation or sale would be unlawful prior to registration or qualification under the securities laws of any such jurisdiction . No offer of securities shall be made except by means of a prospectus meeting the requirements of Section 10 of the Securities Act of 1933 , as amended, or in an offering exempt from registration . Certain information contained in this Presentation relates to or is based on studies, publications, surveys and the Company’s own internal estimates and research . In addition, all of the market data included in this presentation involves a number of assumptions and limitations, and there can be no guarantee as to the accuracy or reliability of such assumptions . Finally, while the Company believes its internal research is reliable, such research has not been verified by any independent source . All the scientific and clinical data presented within this presentation are – by definition prior to completion of the clinical trial and a clinical study report – preliminary in nature and subject to further quality checks including customary source data verification . 2

Therapeutic Opportunity Potential for addressing large patient populations with high prevalence targets in solid tumors Two Clinical - Stage Modalities Pipeline of TCR - T and TCR Bispecific product candidates in clinical & preclinical development Building a Leading TCR Therapeutics Company 3 Intro Differentiated Platforms Unique technologies to identify true cancer targets and right TCRs Clinical PoC for Cell Therapy Anti - tumor activity and durability of response across multiple solid tumors in early TCR - T clinical development

Upcoming 2024 Catalysts for ACTengine® and TCER® Clinical Lead Assets Projected Cash Runway Well into 2026 to Reach Multiple Value Inflections Points 4 IMA203 GEN1 • Update on clinical development plan in 1Q 2024 • Targeted registration - enabling Phase 2 trial for ACTengine® IMA203 GEN1 in melanoma IMA203CD8 GEN2 • Interim data update with longer follow - up planned ACTengine® IMA203 / IMA203CD8 (PRAME) First clinical data update from dose escalation in ongoing Phase 1 trial planned TCER® IMA401 (MAGEA4/8) First clinical data update from dose escalation in ongoing Phase 1/2 trial planned Initial focus indications: Ovarian cancer, uterine cancer, lung cancer, melanoma and others TCER® IMA402 (PRAME) Updates planned across the entire clinical portfolio throughout 2024 Intro

Our TCR - based Approaches Leverage the Full Target Space beyond the Cancer Cell Surface 5 Intro
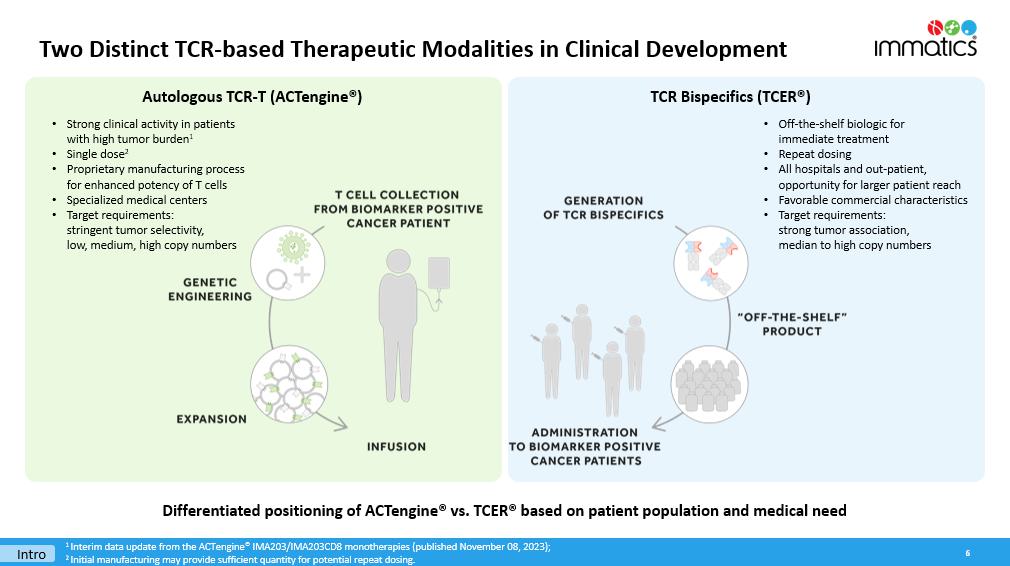
Two Distinct TCR - based Therapeutic Modalities in Clinical Development 6 Differentiated positioning of ACTengine® vs. TCER® based on patient population and medical need Intro 1 Interim data update from the ACTengine® IMA203/IMA203CD8 monotherapies (published November 08, 2023); 2 Initial manufacturing may provide sufficient quantity for potential repeat dosing. Autologous TCR - T (ACTengine®) TCR Bispecifics (TCER®) • Strong clinical activity in patients with high tumor burden 1 • Single dose 2 • Proprietary manufacturing process for enhanced potency of T cells • Specialized medical centers • Target requirements: stringent tumor selectivity, low, medium, high copy numbers • Off - the - shelf biologic for immediate treatment • Repeat dosing • All hospitals and out - patient, opportunity for larger patient reach • Favorable commercial characteristics • Target requirements: strong tumor association, median to high copy numbers
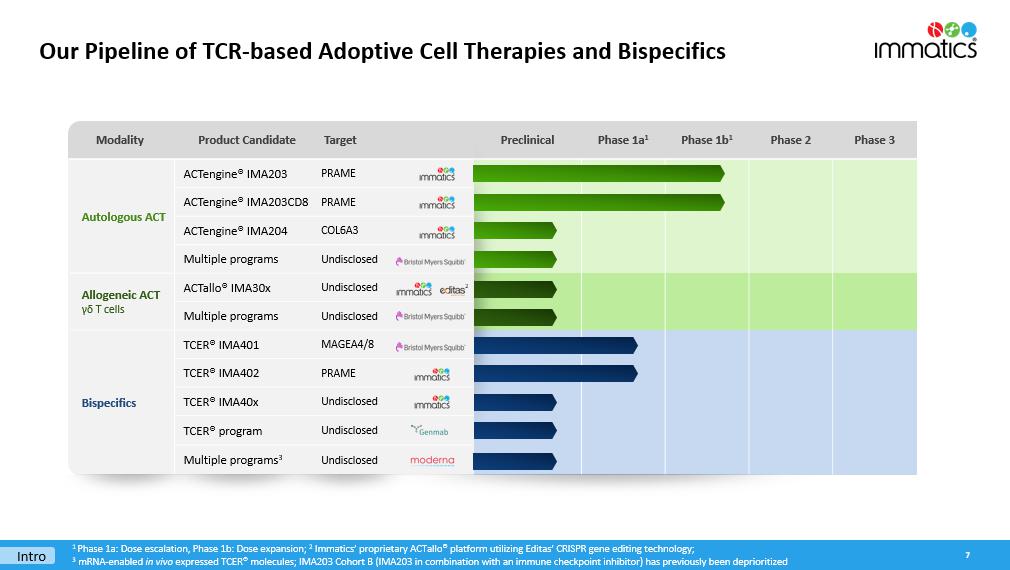
Modality Product Candidate Target Preclinical Phase 1a 1 Phase 1b 1 Phase 2 Phase 3 Autologous ACT ACTengine® IMA203 PRAME ACTengine® IMA203CD8 PRAME ACTengine® IMA204 COL6A3 Multiple programs Undisclosed Allogeneic ACT γδ T cells ACTallo® IMA30x Undisclosed Multiple programs Undisclosed Bispecifics TCER® IMA401 MAGEA4/8 TCER® IMA402 PRAME TCER® IMA40x Undisclosed TCER® program Undisclosed Multiple programs 3 Undisclosed Our Pipeline of TCR - based Adoptive Cell Therapies and Bispecifics 7 Intro 1 Phase 1a: Dose escalation, Phase 1b: Dose expansion ; 2 I mmatics ’ proprietary ACTallo® platform utilizing Editas’ CRISPR gene editing technology; 3 mRNA - enabled in vivo expressed TCER® molecules ; IMA203 Cohort B (IMA203 in combination with an immune checkpoint inhibitor) has previously been deprioritized 2

Immatics & Moderna – A Strategic Multi - Platform R&D Collaboration Combining Immatics’ Target and TCR Platforms with Moderna’s mRNA Technology 8 TCER® mRNA Approach Development of mRNA - enabled in vivo expressed half - life extended TCER® molecules targeting cancer - specific HLA - presented peptides Option for global P&L sharing for most advanced TCER® program TCR - T + mRNA Vaccine Combo mRNA Cancer Vaccines Development of mRNA cancer vaccines by leveraging Moderna’s mRNA technology and Immatics’ target discovery platform XPRESIDENT® and bioinformatics and AI platform XCUBE Ρ Economics • $ 120 million upfront cash payment plus research funding • >$1.7 billion potential development, regulatory & commercial milestones • Potential for tiered royalties on global net sales of TCER® products and certain cancer vaccine products commercialized under the agreement Evaluation of Immatics’ IMA203 TCR - T therapy targeting PRAME in combination with Moderna’s PRAME mRNA - based cancer vaccine 1 Within the collaboration, preclinical activities conducted by Immatics will be managed by the Immatics Discovery Unit, a rece ntl y created internal division at Immatics integrating its technology platforms into one interdisciplinary team focused on all early - stage preclinical pipeline and collaboration programs.; 1 Each Party will retain full ownership of its investigational compound Intro

Strategic Collaborations Synergistic Expertise that Can Foster Transformative Innovations across Various Modalities Research collaboration to develop bispecific immunotherapies $54 M upfront, up to $550 M aggregated milestone payments per program, up to double - digit tiered royalties; Co - promotion option Research collaboration to develop autologous TCR - T therapies $75 M (2019) + $20 M (2022) upfront , up to $505 M aggregated milestone payments per program, tiered royalties; Co - development/Co - fund option; Opt - in right for 1 st program exercised by BMS in 2Q 2023 for $15 M option exercise fee Research collaboration to develop off - the - shelf allogeneic γδ - based TCR - T/ CAR - T programs $60 M upfront up to $700 M milestone payments per program, low double - digit tiered royalties Clinical co - development collaboration to develop Immatics’ TCR Bispecific program TCER® IMA401 $150 M upfront , up to $770 M aggregated milestone payments, double - digit tiered royalties; Co - promotion option in the US 2022 2021 2018 2019 9 Intro 2023 Multi - platform R&D collaboration t o develop in vivo expressed TCER® molecules, mRNA cancer vaccines and combo of TCR - T + mRNA vaccine $120 M upfront , >$1.7 B potential aggregated milestone payments, tiered royalties; Option for global P&L sharing for most advanced TCER®

Potential for Large Patient Populations across Multiple Solid Cancers 10 Uterine Carcinoma – 97 % Uterine Carcinosarcoma – 100% Sarcoma Subtypes – up to 100% Cut. Melanoma ≥ 95% Uveal Melanoma 1 ≥ 91% Ovarian Carcinoma – 84% Squamous NSCLC – 68% TNBC – 63% Small Cell Lung Cancer – 45% Kidney Carcinoma – up to 40% Cholangiocarcinoma – 33% HNSCC – 27% Esophageal Carcinoma – 27% Breast Carcinoma – 26% Adeno NSCLC – 25% HCC – 18 % Bladder Carcinoma – 18% Squamous NSCLC – 52% Sarcoma Subtypes – up to 60% HNSCC – 36% Bladder Carcinoma – 29 % Uterine Carcinosarcoma – 29% Esophageal Carcinoma – 23% Ovarian Carcinoma – 23% Melanoma – 18 % I MA203 / IMA402 PRAME IMA401 MAGEA4/8 IMA204 COL6A3 Exon 6 Intro ACTengine® and TCER® targets demonstrate high prevalence in m ultiple s olid cancers Target prevalence for selected solid cancer indications are based on TCGA (for SCLC: in - house) RNAseq data combined with a propr ietary mass spec - guided RNA expression threshold ; 1 Uveal melanoma target prevalence is based on IMADetect® qPCR testing of screening biopsies from clinical trial patients (n=33 ) Pancreatic Carcinoma – 76% Breast Carcinoma – 77% Stomach Carcinoma – 67% Sarcoma – 63% Colorectal Carcinoma – 60% Esophageal Carcinoma – 60% Squamous NSCLC – 55% Adeno NSCLC – 57% HNSCC – 56% Uterine Carcinosarcoma – 50% Mesothelioma – 44% Cholangiocarcinoma – 36% Melanoma – 35% Bladder Carcinoma – 34% Ovarian Carcinoma – 31%

Realizing the Full Multi - Cancer Opportunity of PRAME ACTengine® IMA203 (TCR - T) and TCER® IMA402 (TCR Bispecific) 11 ACTengine® IMA203 (TCR - T) Cancer Cell Death PRAME is one of the most promising and most prevalent, clinically validated solid tumor targets known to date Leverage the full potential of targeting PRAME by continued evaluation of the best suited therapeutic modality (ACTengine® vs. TCER® or both) for each cancer type Intro Phase 1b dose expansion ongoing TCER® IMA402 (TCR Bispecific) 1 PRAME target prevalence is based on TCGA (for SCLC: in - house) RNAseq data combined with a proprietary mass spec - guided RNA expre ssion threshold; 2 Uveal melanoma target prevalence is based on IMADetect® qPCR testing of screening biopsies from clinical trial patients (n=33); NSCLC: Non - small cell lung cancer, TNBC: Triple - negative breast cancer, HNSCC: Head and neck squamous cell carcinoma; HCC: Hepatocellular carcinoma Indication % PRAME positive patients 1 Uterine Carcinoma Uterine Carcinosarcoma Sarcoma Subtypes Cut. Melanoma Uveal Melanoma 2 Ovarian Carcinoma Squamous NSCLC TNBC Small Cell Lung Cancer Kidney Carcinoma Cholangiocarcinoma HNSCC Esophageal Carcinoma Breast Carcinoma Adeno NSCLC HCC Bladder Carcinoma 97% 100% up to 100% ≥ 95% ≥ 91% 84% 68% 63% 45% up to 40% 33% 27% 27% 26% 25% 18% 18% Dose escalation of Phase 1/2 trial ongoing

ACTengine® IMA203 – TCR - T Targeting PRAME 12

The Multi - Cancer Opportunity of PRAME One of the Most Promising Solid Tumor Targets for TCR - based Therapies Known To Date 13 High prevalence High target density Homogeneous expression “Clean” expression profile Clinical proof - of - concept s qNSCLC Ovarian Cancer PRAME fulfills all properties of an ideal target for TCR - based therapies PRAME RNA detection in tumor samples (ISH) ISH: in situ hybridization, sqNSCLC : squamous n on - small cell lung cancer IMA203 78025�&(// 7�&(// ,> � Ͳ � Ύ ϬϮ ͗ Ϭϭ WZ�D�� d �Z WZ�D�� W Ğ Ɖ ƟĚĞ

ACTengine® IMA203 Targeting PRAME – Mechanism of Action Immatics’ Leading TCR - T Approach 14 IMA203

ACTengine® IMA203/IMA203CD8 TCR - T Monotherapy – Patient Flow 15 HLA - A*02 Testing Blood sample; Central lab Treatment & Observation Phase Long Term Follow - up Screening & Manufacturing Phase Manufacturing by Immatics Infusion of ACTengine® IMA203 TCR - T Product Lymphodepletion * Target Profiling IMADetect® Biopsy or archived tissue Low dose IL - 2 ** Safety and efficacy monitoring for 12 months Leukapheresis x x Expression Antigen 1 3 2 Short process time of 14 days * 30 mg/m 2 Flu darabine and 500 mg/m 2 Cy clophosphamide for 4 days; ** 1m IU daily days 1 - 5 and twice daily days 6 - 10 7 - day manufacturing process applying CD8/CD4 T cell selection 7 - day QC release testing Cut. Melanoma Uveal Melanoma Uterine Carcinoma Ovarian Carcinoma 95% (58/61) 91% (30/33) 89% (8/9) 82% (23/28) Patient screening data from Immatics’ clinical trials: IMA203

IMA203 GEN1 – Melanoma as First Indication for Pivotal Development 16 * Patients with at least one post treatment tumor response assessment Patient characteristics All comers Cohort A Melanoma pts Ph1a & Cohort A at RP2D Ovarian cancer pts Ph1a & Cohort A at RP2D Efficacy population* 18 13 4 Prior lines of treatment Median (min, max) 3 (0, 10) 4 (0, 7) 4.5 (3, 10) LDH at baseline >1 x ULN [% of patients] 50.0 53.9 100.0 Baseline tumor burden Target lesion sum of diameter [mm] (median, min, max) 58.9 (21.0, 207.3) 52.0 (21.0, 178.7) 108.8 (50.6, 207.3) Patient Numbers* ALL Melanoma Ovarian Cancer Synovial Sarcoma H&N Cancer Others Phase 1a RP2D 7 5 0 0 0 2 Cohort A RP2D 18 8 4 3 1 2 All 8 cut. melanoma patients were CPI - refractory and 5 of 8 were BRAF - inhibitor pretreated • Sub - group analysis per tumor type at target dose includes data from Phase 1a plus Cohort A at RP2D • Melanoma patient number (N=13) and characteristics allow such sub - group analysis for initial assessment of anti - tumor activity • For other tumor types, appropriate patient numbers and characteristics have not yet been achieved All ovarian cancer patients were platinum - resistant Data cut - off Sep 30, 2023 IMA203

ACTengine® IMA203 / IMA203CD8 TCR - T Monotherapy Two Assets with Distinct Opportunities and Near - Term Catalysts 17 GEN1: IMA203 in Melanoma at RP2D GEN2: IMA203CD8 in Solid Tumors Initial Clinical Data • Complete dose escalation • Signal finding in non - melanoma indications, such as ovarian cancer, uterine cancer, NSCLC, triple - negative breast cancer and others Development Path Clinical Data Cell Product Manufacturing • 7 - day manufacturing process, plus 7 - day release testing • RP2D defined at 1 - 10x10 9 total TCR - T cells • Manufacturing success rate: >95% • Well tolerated • 50% (6/12) confirmed objective response rate ( cORR ) • Durability with ongoing responses at 15+ months; mDOR not reached at mFU of 14.4 months • Manageable tolerability • 56% (5/9) confirmed objective response rate ( cORR ) • Durable response at 12+ months; mDOR not reached at mFU of 4.8 months • 6 out of 7 responses ongoing at data cut - off • Enhanced pharmacology with differentiated response pattern Development Path • FDA RMAT designation for multiple PRAME+ cancers including cutaneous & uveal melanoma • IMA203 GEN1 in melanoma targeted to enter registration - enabling Phase 2 trial in 2024 • Update on clinical development plan in 1Q 2024 mDOR : median Duration of Response; mFU : median Follow - up ; RP2D: Recommended Phase 2 Dose Data cut - off Sep 30, 2023 IMA203

ACTengine® IMA203 / IMA203CD8 TCR - T Trial in Advanced Solid Tumors Overview D ose Level 1 - 4 ( total N=27): Patients in DL4 (N=7) treated at RP2D Phase 1b Dose Expansion Phase 1a Dose Escalation Efficacy population shown: patients treated with IMA203 (Cohort A) or IMA203CD8 (Cohort C) and with at least one available tu mor response assessment post infusion; RP2D: Recommended Phase 2 Dose of 1 - 10x10 9 total TCR - T cells; IMA203 DL4: 0.2 - 1.2x10 9 TCR - T cells/m 2 BSA, IMA203 DL5: 1.201 x 4.7x10 9 TCR - T cells/m 2 BSA; IMA203CD8 DL3: 0.2 - 0.48x10 9 TCR - T cells/m 2 BSA, IMA203CD8 DL4a: 0.481 - 0.8x10 9 TCR - T cells/m 2 BSA, IMA203CD8 DL4b: 0.801 - 1.2x10 9 TCR - T cells/m 2 Data cut - off Sep 30, 2023 Phase 1a and Cohort A data set in appendix; Cohort B deprioritized, summary analysis in appendix GEN1 : IMA203 GEN2 : IMA203CD8 Functional CD8 TCR - T cells only Functional CD8 and CD4 TCR - T cells Today’s update focuses on 13 melanoma patients treated at RP2D with IMA203 GEN1 and 12 all comers patients treated with IMA203CD8 GEN2 Melanoma Patients at RP2D: Total N=13 (5 Ph1a + 8 Cohort A) Cohort C (N=12): Dose Level 3/4a/4b Dose escalation ongoing Cohort A (total N=18) : Dose Level 4/5 All patients treated at RP2D 18 IMA203

Overview of Patient Characteristics and Responses 19 * Patients with at least one available tumor response assessment post infusion; # All patients were PD at data cut - off; Initial ORR: Objective response rate according to RECIST 1.1 at any post infusion scan; Confirmed ORR ( cORR ): Confirmed objective response rate according to RECIST 1.1 for patients with at least two available post infusion scans or patients with progressi ve disease (PD) at any prior timepoint, patients with ongoing unconfirmed PR not included in cORR calculation; Duration of response (DOR) in confirmed responders is defined as time from first documented response until disease progression/death. Pat ien ts with ongoing response will be censored at date of data cut - off. Median DOR is analyzed by using the Kaplan - Meier method; Median Follow - up is analyzed by using the reverse Kaplan - Meier method; DOR: Duration of Response; FU: Follow - up IMA203 GEN1 IMA203CD8 GEN2 All Comers (N=45) Melanoma Subgroup (N=13 of 45) All Comers (N=12) Phase 1a Cohort A Phase 1a + Cohort A Cohort C Efficacy population* N=27 Thereof N=7 at RP2D N=18 at RP2D N=13 at RP2D N=12 Prior lines of systemic treatment ( median, min, max) 4 (1, 8) 3 (0, 10) 4 (0, 7) 3 (1, 5) LDH at baseline >1 x ULN [% of patients] 66.7 50.0 53.8 50.0 Baseline tumor burden Median target lesion sum of diameter [mm] (min, max) 133.0 (29, 219.7) 58.9 (21, 207.3) 52.0 (21.0, 178.7) 79.8 (20.0, 182.0) Dose level DL1 - 4 DL4/5 DL4/5 DL3/DL4a/DL4b ORR 48% (13/27) 50% (9/18) 62% (8/13) 58% (7/12) cORR 19% (5/27) 47% (8/17) 50% (6/12) 56% (5/9) mDOR [months] 4.4 (2.4, 23.0) Not reached Not reached Not reached mFU [months] Not defined # 10.8 14.4 4.8 Data cut - off Sep 30, 2023 Heavily Pretreated Patient Population across Clinical Trial Cohorts IMA203

ACTengine® IMA203 TCR - T Interim Update Delivering a Meaningful Benefit to Patients with an Unmet Medical Need 20 IMA203 GEN1 Monotherapy Phase 1a & Cohort A – Focus on Melanoma at RP2D IMA203CD8 GEN2 Monotherapy Cohort C – First Data Set on 2 nd Generation Summary & Next Development Steps IMA203

21 Data cut - off Sep 30, 2023 IMA203 GEN1 in All Melanoma Patients at RP2D – Most Frequent Adverse Events • Expected cytopenia (Grade 1 - 4) associated with lymphodepletion in all patients • Mostly mild to moderate cytokine release syndrome (CRS) • 63% (10/16) with Grade 1 CRS • 31% (5/16) with Grade 2 CRS • 6% (1/16) with Grade 3 CRS (Phase 1a patient; recovered to Grade 2 after 3 days, no need for vasopressors and/or ventilation) • No dose - dependent increase of CRS • O ne non - serious, mild (Grade 1) ICANS 2 in DL5 • No dose - limiting toxicity • No IMA203 - related deaths • full IMA203 GEN1 monotherapy safety profile (generally consistent with safety in melanoma subset), see next slide 1 Three cutaneous melanoma patients treated with IMA203 and pending post infusion scan included in safety population, but not e ff icacy population; 2 I CANS: Immune Effector Cell - Associated N eurotoxicity S yndrome ; CRS and ICANS graded by CARTOX criteria ( Neelapu et al ., 2018) N=16 Patients in Safety Population 1 IMA203 GEN1 monotherapy continues to be well tolerated at total doses between 1 - 10x10 9 TCR - T cells (RP2D) IMA203

Adverse event ( System organ class , Preferred term ) ≥ Grade 3 No . % Patients with any adverse event 49 100.0 Adverse Events of Special Interest 2 4.1 Cytokine release syndrome 2 4.1 ICANS 2 0 0.0 Blood and lymphatic system disorders 48 98.0 Neutropenia 36 73.5 Lymphopenia 27 55.1 Leukopenia 26 53.1 Anaemia 24 49.0 Thrombocytopenia 17 34.7 Cytopenia 1 2.0 Leukocytosis 1 2.0 Lymphocytosis 1 2.0 Investigations 9 18.4 Neutrophil count decreased 4 8.2 Alanine aminotransferase increased 2 4.1 Aspartate aminotransferase increased 2 4.1 White blood cell count decreased 2 4.1 Blood alkaline phosphatase increased 1 2.0 Blood creatinine increased 1 2.0 Blood fibrinogen decreased 1 2.0 Infections and infestations 7 14.3 Appendicitis 1 2.0 COVID - 19 1 2.0 Enterococcal infection 1 2.0 Infection 1 2.0 Orchitis 1 2.0 Sepsis 4,5 1 2.0 Septic shock 4 1 2.0 Urinary tract infection 1 2.0 Respiratory, thoracic and mediastinal disorders 6 12.2 Hypoxia 3 6.1 Bronchial obstruction 1 2.0 Laryngeal inflammation 1 2.0 Pleural effusion 1 2.0 Respiratory failure 1 2.0 Vascular disorders 6 12.2 Hypertension 4 8.2 Hypotension 2 4.1 Adverse event ( System organ class , Preferred term ) ≥ Grade 3 No . % table continued… General disorders and administration site conditions 4 8.2 Condition aggravated 4 1 2.0 Fatigue 1 2.0 Pyrexia 1 2.0 Swelling face 1 2.0 Metabolism and nutrition disorders 4 8.2 Hypokalaemia 3 6.1 Failure to thrive 1 2.0 Hypophosphataemia 1 2.0 Gastrointestinal disorders 2 4.1 Abdominal pain 1 2.0 Diarrhoea 1 2.0 Vomiting 1 2.0 Injury, poisoning and procedural complications 2 4.1 Humerus fracture 1 2.0 Infusion related reaction 1 2.0 Renal and urinary disorders 2 4.1 Acute kidney injury 1 2.0 Proteinuria 1 2.0 Skin and subcutaneous tissue disorders 2 4.1 Rash maculo - papular 2 4.1 Cardiac disorders 1 2.0 Atrial fibrillation 3 1 2.0 Endocrine disorders 1 2.0 Inappropriate antidiuretic hormone secretion 1 2.0 Eye disorders 1 2.0 Ulcerative keratitis 1 2.0 Hepatobiliary disorders 1 2.0 Cholangitis 1 2.0 Immune system disorders 1 2.0 Contrast media allergy 1 2.0 Musculoskeletal and connective tissue disorders 1 2.0 Muscle spasms 1 2.0 Nervous system disorders 1 2.0 Headache 1 2.0 Reproductive system and breast disorders 1 2.0 Vaginal haemorrhage 1 2.0 IMA203 GEN1 across All Dose Levels – Tolerability Data Phase 1a Dose Escalation and Cohort A – All ≥Grade 3 Adverse Events (N=49) 22 • Well tolerated at doses as high as ~10x10 9 TCR - T cells • No AE ≥Grade 3 was observed with a frequency ≥10% when excluding expected cytopenia associated with lymphodepletion • No IMA203 - related Grade 5 Adverse Events All treatment - emergent adverse events (TEAEs) with ≥ Grade 3 regardless of relatedness to study treatment that occurred in at least 1 patient (except for ICANS, where only Grade 1 - 2 occurred ; listed for completeness due to being an adverse event of special interest) are presented . Adverse events were coded using the Medical Dictionary for Regulatory Activities . Grades were determined according to National Cancer Institute Common Terminology Criteria of Adverse Events, version 5 . 0 . Grades for CRS and ICANS were determined according to CARTOX criteria ( Neelapu et al . , 2018 ) . Patients are counted only once per adverse event and severity classification . Based on interim data extracted from open clinical database ( 30 - Sep - 2023 ) ; 1 Two patients with disease progression after first IMA 203 infusion received exploratory second IMA 203 infusion . They had these ≥ Grade 3 TEAEs only after second infusion, which are included in the table : First patient : Abdominal pain, Cytokine release syndrome, Diarrhoea , Hypokalaemia , Proteinuria ; Second patient : Humerus fracture, Muscle spasms, Neutropenia, Thrombocytopenia ; 2 ICANS : Immune effector cell - associated neurotoxicity syndrome ; 3 DLT : Dose limiting toxicity in phase 1 a at DL 2 reported on March 17 , 2021 ; 4 Fatal Adverse events were not considered related to any study drug ; 5 Patient died from sepsis of unknown origin and did not receive IMA 203 TCR - T cells . TEAEs by maximum severity for all patients in Phase 1a dose escalation and Cohort A dose expansion (N=49) 1 Data cut - off Sep 30, 2023

# # # # # # # # # # IMA203 GEN1 in All Melanoma Patients at RP2D (N=13) – BOR and Response over Time Durable Responses 15+ Months after Treatment 23 Data cut - off Sep 30, 2023 Ongoing ORR 62% (8/13) cORR 50% (6/12) Initial ORR: Objective response rate according to RECIST 1.1 at any post infusion scan; Confirmed ORR ( cORR ): Confirmed objective response rate according to RECIST 1.1 for patients with at least two available post infusion scans or pat ients with progressive disease (PD) at any prior timepoint, patients with ongoing unconfirmed PR not included in cORR calculation; Duration of response (DOR) in confirmed responders is defined as time from first documented response until disease progression/death. Patients with ongoing response will be censored at date of data cut - off. Median DOR is analyzed by using the Kaplan - Meier method; Median Follow - up is analyzed by using the reverse Kaplan - Meier method; PD: Progressive Disease; SD: Stable Disease; PR: Partial Response; cPR : Confirmed Partial Response; BL: Baseline; BOR: Best Overall Response; DOR: Duration of Response; Scans at approximately week 6, month 3 and then every 3 months # Patients in Phase 1a Median DOR, min, max DOR Not reached, 2.2+, 14.7+ months Median Follow - up 14.4 months IMA203

24 High Medical Need in Cutaneous and Uveal Melanoma Clinically and Commercially Attractive Features of IMA203 Cutaneous Melanoma Uveal Melanoma Patient Population 2L+ CPI - refractory, BRAF/MEK inhibitor - refractory if BRAF mutation+ 2L+ Kimmtrak - refractory, CPI/chemotherapy - refractory IMA203 Opportunity ~3,000 HLA - A*02:01 and PRAME - positive cutaneous melanoma patients annually in the US 1 ~300 HLA - A*02:01 and PRAME - positive uveal melanoma patients annually in the US 2 Well tolerated Mostly mild to moderate CRS, infrequent & mild ICANS Promising anti - tumor activity ( cORR , mDOR ) Leukapharesis as source for cell product, no surgery required Short manufacturing time of 7 days plus 7 days of QC release testing Low dose IL - 2 post IMA203 infusion with better tolerability profile than high dose IL - 2 CPI: Checkpoint inhibitor; 1 Based on annual mortality of ~7,700 cutaneous melanoma patients in the US, HLA - A*02:01 prevalence of 41% in the US and PRAME pr evalence of 95% (TCGA RNAseq data combined with proprietary MS - guided RNA expression threshold); 2 Based on annual mortality of ~800 uveal melanoma patients in the US, HLA - A*02:01 prevalence of 41% in the US and PRAME prevalen ce of 91% (IMADetect® qPCR testing of screening biopsies from clinical trial patients (n=33)) ≥95% of cutaneous melanoma patients are PRAME - positive Data cut - off Sep 30, 2023 IMA203 GEN1 in Melanoma Targeted to Enter Registration - Enabling Phase 2 Trial in 2024 IMA203

ACTengine® IMA203 TCR - T Interim Update Delivering a Meaningful Benefit to Patients with an Unmet Medical Need 25 IMA203 GEN1 Monotherapy Phase 1a & Cohort A – Focus on Melanoma at RP2D IMA203CD8 GEN2 Monotherapy Cohort C – First Data Set on 2 nd Generation Summary & Next Development Steps IMA203

IMA203CD8 GEN2 – IMA203 TCR - T Monotherapy Leveraging CD8 and CD4 cells Differentiated Pharmacology Compared to 1 st - Generation TCR - only Approaches • IMA203CD8 GEN2 designed to broaden the clinical potential of IMA203 TCR - T monotherapy by adding functional CD4 T cells via co - transduction of CD8 αβ alongside PRAME TCR • Activated CD4 T cells aid activity of other immune cells by releasing cytokines and acquire cytotoxic functions • Functional CD4 T cells mediate longer anti - tumor activity than CD8 T cells and potentiate the anti - tumor activity of the cell product in preclinical studies 1 • Data from CD19 CAR - T - treated leukaemia patients suggest a relevant role of engineered CD4 T cells in long - term durability 2 TUMOR CELL DEATH CD4 T CELL Cytotoxic Activity CD8 T CELL T cell Help Cytotoxic Activity 26 1 Internal data not shown here, published in Bajwa et al. 2021 Journal for Immunotherapy of Cancer; 2 M elenhorst et al. 2022 Nature , Bai et al. 2022 Science Advances CD8 PRAME TCR IMA203CD8
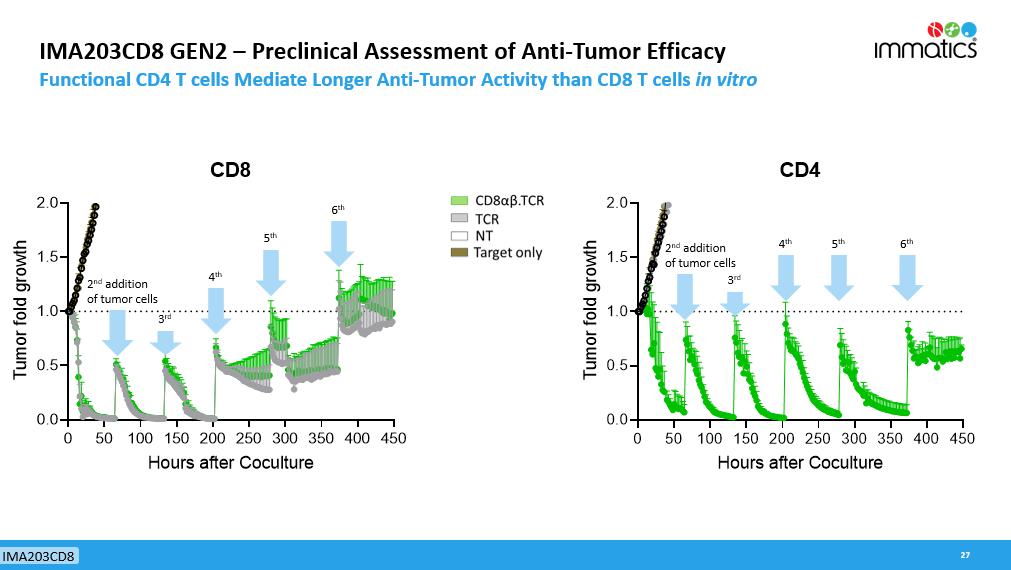
IMA203CD8 GEN2 – Preclinical Assessment of Anti - Tumor Efficacy Functional CD4 T cells Mediate Longer Anti - Tumor Activity than CD8 T cells in vitro 27 0 50 100 150 200 250 300 350 400 450 0.0 0.5 1.0 1.5 2.0 CD8 Hours after Coculture T u m o r f o l d g r o w t h 0 50 100 150 200 250 300 350 400 450 0.0 0.5 1.0 1.5 2.0 CD4 Hours after Coculture T u m o r f o l d g r o w t h 2 nd addition of tumor cells 3 rd 4 th 5 th 6 th 2 nd addition of tumor cells 3 rd 4 th 5 th 6 th IMA203CD8

IMA203CD8 GEN2 in Cohort C (N=12) – Most Frequent Adverse Events Manageable Tolerability in 12 Patients Treated with IMA203CD8 at 3 Escalating Dose Levels 1 • Expected cytopenia (Grade 1 - 4) associated with lymphodepletion in all patients • Cytokine release syndrome (CRS) in 92% (11/12) of patients: Trend towards more severe CRS at higher doses, in all cases well manageable • 67 % (8/12) with Grade 1 or 2 CRS (4 in DL3, 3 in DL4a, 1 in DL4b) • 17% (2/12) with Grade 3 CRS (2 in DL4b; patient C - DL4b - 04, see also description below) • 8% (1/12) with Grade 4 CRS (1 in DL4b, patient C - DL4b - 01, see also description below ) • One patient with neurotoxicity (see below), no ICANS 2 or neurotoxicity reported for the other patients • Dose - limiting toxicities (DLTs) at Dose Level 4b were observed in 2 of 4 patients 1) In patient C - DL4b - 01 treated with highest possible dose at DL4b, high biological activity ( in vivo T cell expansion) observed; patient developed Grade 4 neurotoxicity and Grade 4 CRS on day 6 after infusion, combined with Grade 3 Hemophagocytic Lymphohistiocytosis (HLH) 2) Patient C - DL4b - 04 treated at DL4b developed Grade 3 CRS with transient Grade 3 liver enzyme (ALT) increase that resolved to Grad e 2 within 10 days; no need for vasopressors or ventilation at any time • No high - grade CRS, no neurotoxicity and no DLTs were reported for 4 patients treated at DL3 and 4 patients treated at DL4a • No IMA203CD8 - related deaths • Expanded DL4a dose cohort ongoing 28 1 N=4 DL3, N=4 DL4a, N=4 DL4b, DL3: 0.2 - 0.48x10 9 TCR - T cells/m 2 BSA, DL4 is split into a DL4a (0.481 - 0.8x10 9 TCR - T cells/m 2 BSA) and DL4b (0.801 - 1.2x10 9 TCR - T cells/m 2 BSA); 2 I CANS: Immune Effector Cell - Associated N eurotoxicity S yndrome ; CRS and ICANS graded by CARTOX criteria ( Neelapu et al ., 2018) IMA203CD8 GEN2 monotherapy shows a manageable tolerability profile Data cut - off Sep 30, 2023 IMA203CD8

Tolerability Data – Cohort C IMA203CD8 GEN2 29 Adverse event ≥ Grade 3 ( System organ class , preferred term) No. % Patients with any adverse event 12 100.0 Adverse events of special interest 3 25.0 Cytokine release syndrome 1 3 25.0 Immune effector cell - associated neurotoxicity syndrome 0 0.0 Blood and lymphatic system disorders 11 91.7 Neutropenia 9 75.0 Anaemia 8 66.7 Lymphopenia 8 66.7 Thrombocytopenia 4 33.3 Leukopenia 2 16.7 Investigations 4 33.3 Aspartate aminotransferase increased 2 16.7 Neutrophil count decreased 2 16.7 Alanine aminotransferase increased 1 8.3 Blood alkaline phosphatase increased 1 8.3 Blood bilirubin increased 1 8.3 Gamma - glutamyltransferase increased 1 8.3 Metabolism and nutrition disorders 2 16.7 Hypermagnesaemia 1 8.3 Hypoalbuminaemia 1 8.3 Hypophosphataemia 1 8.3 Nervous system disorders 2 16.7 Neurotoxicity 2 1 8.3 Syncope 1 8.3 Immune system disorders 1 8.3 Haemophagocytic lymphohistiocytosis 2 1 8.3 Infections and infestations 1 8.3 Infection 1 8.3 All treatment - emergent adverse events (TEAEs) with ≥ Grade 3 regardless of relatedness to study treatment that occurred in at least 1 patient ( except for ICANS, where no event was documented; listed for completeness due to being an adverse event of special interest) are presented. Adverse events were coded using the Medical Dictionary for Regulatory Activities. Grades were determined according to National Cancer Institute Common Terminology Criteria of Adverse Events, version 5.0. Grades for CRS and ICANS were determined according to CARTOX criteria ( Neelapu et al., 2018). Patients are counted only once per adverse event and severity classification. Based on interim data extracted from open clinical database (30 - Sep - 2023) ; 1 DLT: Dose limiting toxicity in patient DL4b - 04. 2 DLTs in patient DL4b - 01; All ≥Grade 3 Adverse Events (N=12) TEAEs by maximum severity for all patients in Cohort C (N= 12 ) • Manageable tolerability • Most frequent ≥Grade 3 AEs were expected cytopenia associated with lymphodepletion • No IMA203CD8 - related Grade 5 Adverse Events • Dose escalation ongoing Data cut - off Sep 30, 2023
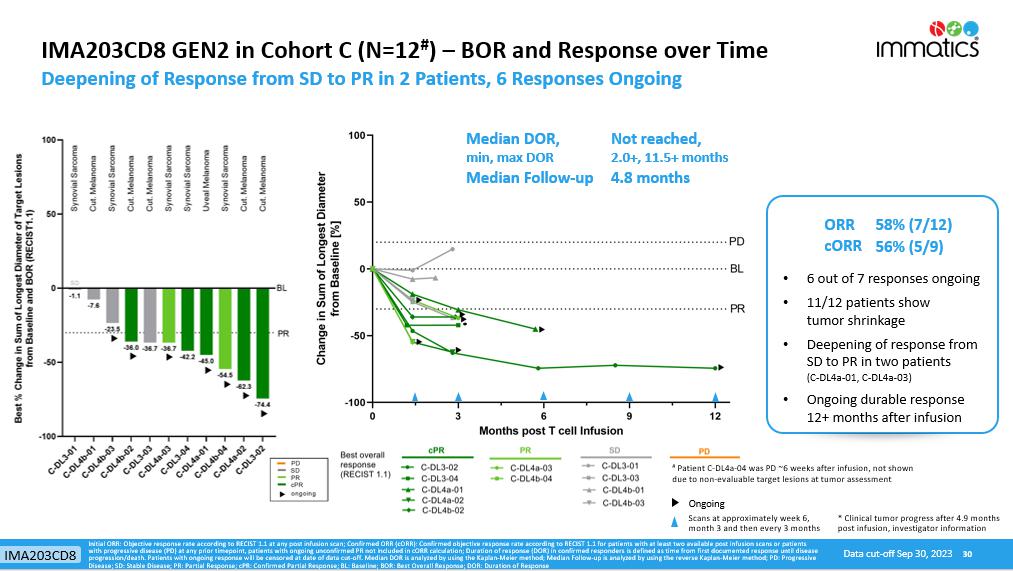
IMA203CD8 GEN2 in Cohort C (N=12 # ) – BOR and Response over Time Deepening of Response from SD to PR in 2 Patients, 6 Responses Ongoing 30 • 6 out of 7 responses ongoing • 11/12 patients show tumor shrinkage • Deepening of response from SD to PR in two patients (C - DL4a - 01, C - DL4a - 03) • Ongoing durable response 12+ months after infusion Median DOR, min, max DOR Not reached, 2.0+, 11.5+ months Median Follow - up 4.8 months ORR 58% (7/12) cORR 56% (5/9) Initial ORR: Objective response rate according to RECIST 1.1 at any post infusion scan; Confirmed ORR ( cORR ): Confirmed objective response rate according to RECIST 1.1 for patients with at least two available post infusion scans or pat ients with progressive disease (PD) at any prior timepoint, patients with ongoing unconfirmed PR not included in cORR calculation; Duration of response (DOR) in confirmed responders is defined as time from first documented response until disease progression/death. Patients with ongoing response will be censored at date of data cut - off. Median DOR is analyzed by using the Kaplan - Meier method; Median Follow - up is analyzed by using the reverse Kaplan - Meier method; PD: Progressive Disease; SD: Stable Disease; PR: Partial Response; cPR : Confirmed Partial Response; BL: Baseline; BOR: Best Overall Response; DOR: Duration of Response # Patient C - DL4a - 04 was PD ~6 weeks after infusion, not shown due to non - evaluable target lesions at tumor assessment Scans at approximately week 6, month 3 and then every 3 months Ongoing Data cut - off Sep 30, 2023 * Clinical tumor progress after 4.9 months post infusion, investigator information * IMA203CD8

IMA203CD8 GEN2: Translational Data Shows Enhanced Pharmacology Cohort A IMA203 GEN1 (All Patients at RP2D) vs Cohort C IMA203CD8 GEN2 31 Trend towards responses at lower cell dose and higher tumor burden with IMA203CD8 Higher peak expansion ( C max ) of IMA203CD8 T cells when normalized to infused dose Higher activation levels in IMA203CD8 T cells at week 1… …without exhaustion over time Initial translational data indicates higher biological and clinical activity of IMA203CD8 GEN2 % PD - 1 of specific T cells at week1: for patient A - DL5 - 05 data not available for week 1 0 5×10 5 1×10 6 1.5×10 6 2×10 6 2.5×10 6 V e c t o r c o p i e s / μ g g D N A p=0.0010 PR cPR PD/SD Cohort A IMA203 GEN1 Cohort C IMA203CD8 GEN2 Data cut - off Sep 30, 2023 IMA203CD8

ACTengine® IMA203 TCR - T Interim Update Delivering a Meaningful Benefit to Patients with an Unmet Medical Need 32 IMA203 GEN1 Monotherapy Phase 1a & Cohort A – Focus on Melanoma at RP2D IMA203CD8 GEN2 Monotherapy Cohort C – First Data Set on 2 nd Generation Summary & Next Development Steps IMA203

ACTengine® IMA203 / IMA203CD8 TCR - T Monotherapy Targeting PRAME Summary of GEN1 and GEN2 Clinical Data and Planned Next Steps 33 Next Step Alignment with FDA on patient population, trial design, CMC targeting registration - enabling Phase 2 trial in melanoma • Well tolerated, mostly mild to moderate CRS, infrequent & mild ICANS • 50% (6/12) cORR , mDOR not reached at mFU of 14.4 months • Durability with ongoing responses at 15+ months in some patients • RP2D defined at 1 - 10x10 9 total TCR - T cells • FDA RMAT designation received in multiple PRAME expressing cancers including cutaneous and uveal melanoma • Enhanced primary and secondary pharmacology when compared to GEN1 • Manageable tolerability (2 DLTs at DL4b, dose escalation ongoing) • Initial clinical activity observed with differentiated response pattern • 56% (5/9) cORR • 6 out of 7 responses ongoing at data cut - off, durable response at 12+ months • SD converting to PR over time (N=2) • Enhanced biological efficacy with PRs at lower T cell:tumor cell ratio compared to IMA203 GEN1 IMA203 GEN1 Monotherapy in Melanoma at RP2D IMA203CD8 GEN2 Monotherapy IMA203 GEN1 Monotherapy in Melanoma at RP2D Next Step Complete dose escalation and further dose expansion with focus on non - melanoma patients Data cut - off Sep 30, 2023 IMA203

PRAME mRNA expression in IMA203 GEN1 Phase 1a and Cohort A responders at RP2D (n=13) PRAME mRNA expression in IMA203CD8 GEN2 Cohort C responders (n=7) Potential of IMA203 in Additional Solid Cancer Indications Based on PRAME Expression in IMA203 GEN1 and IMA203CD8 GEN2 Responders 34 % PRAME - positive patients 1 PRAME target expression distribution (blue histogram) based on TCGA RNAseq data, patient data (black dots) based on IMADetect ® q PCR testing of screening biopsies; 1 PRAME target prevalence is based on TCGA RNAseq data combined with a proprietary MS - guided RNA expression threshold; 2 PRAME target prevalence in uveal melanoma based on IMADetect® qPCR testing of screening biopsies from clinical trial patients ( n=33) demonstrates substantial higher prevalence of 91% compared to prevalence based on TCGA data of 50%, TCGA: early & late - stage primary tumor samples, Immatics clinical trials: late - stage/metastatic tumor samples, Role of PRAME in metastasis of uveal melanoma: Field et al. 2016 Clinical Cancer Research; MS: mass spectrometry Data cut - off Sep 30, 2023 ≥ 95% ≥ 91% (50% 2 ) 97% 100% 84% 68% 63% 27% Immatics’ current MS - guided mRNA threshold for patient selection Selected indications Clinical activity shown No clinical activity expected Potential opportunity to see clinical activity IMA203

ACTengine® IMA203 / IMA203CD8 TCR - T Monotherapy Targeting PRAME Leveraging the Full Breath of PRAME in Three Steps 35 Development Strategy Step 1 IMA203 GEN1 in cutaneous melanoma (potentially bundled with uveal melanoma) as first tumor type targeted to enter registration - enabling trial Signal finding in ovarian cancer and uterine cancer in dedicated dose expansion cohorts, preferentially with IMA203CD8 GEN2 Pursue tumor - agnostic label in PRAME+ solid cancers to leverage full breadth of PRAME - including NSCLC, triple - negative breast cancer and others Step 2 Step 3 2024 2024 IMA203

ACTengine® IMA203 TCR - T Product Manufacturing Enhancing Manufacturing Process and Capabilities Leukapheresis 1 - Week Manufacturing Process 1 - Week QC Release Testing Infusion - ready Manufacturing of ACTengine® IMA203 TCR - T & other future autologous /allogeneic candidates Expected to be operational in 2024 Approx. 100,000 sq ft in Houston area, TX – modular and flexible design Early - stage and registration - directed clinical trials as well as initial commercial supply State - of - the - art research & GMP manufacturing facility Short manufacturing turnaround time 36 IMA203

Selected Indications Incidence R/R Incidence PRAME Positive Patient Population Based on R/R Incidence; PRAME and HLA - A*02:01+ Cut. Melanoma 99,800 7,700 95% 2,999 Uveal Melanoma 1,500 800 91% 298 Ovarian Carcinoma 19,900 12,800 84% 4,408 Uterine Carcinoma 62,700 10,700 97% 4,255 Uterine Carcinosarcoma 3,300 1,900 100% 779 Squamous NSCLC 57,000 34,600 68% 9,646 Small Cell Lung Cancer 31,900 19,400 45% 3 ,579 Adeno NSCLC 91,200 55,300 25% 5,668 HNSCC 66,500 15,100 27% 1,672 Breast Carcinoma 290,600 43,800 26% TNBC: 63% 4,669 Synovial Sarcoma 1,000 400 100% 164 Cholangiocarcinoma 8,000 7,000 33% 9 47 IMA203 TCR - T Has the Potential to Reach a Large Patient Population ~39,000 Patients per Year in the US only 37 Incidences based on public estimates and Immatics internal model; Relapsed/refractory (R/R) or last - line patient population approximated by annual mortality; Estimated 41% HLA - A*02:01 positive population in the US; PRAME target prevalence is based on TCGA (for SCLC: in - house) RNAseq data combined with a proprietary mass spec - guided RNA expression threshold ; Uveal melanoma target prevalence is based on IMADetect® qPCR testing of screening biopsies from clinical trial patients (n= 33) Multiple opportunities to broaden patient reach and patient benefit: » Expand beyond US population » Expand into other indications such as kidney, esophageal, bladder, other liver cancers, other sarcoma subtypes through indication - specific or indication - agonistic label expansion » Move into earlier lines of therapy (R/R Incidence Incidence ) » Inclusion of patients with lower PRAME - threshold TOTAL ~ 39 ,000 annually in the US IMA203

ACTengine® IMA204 – TCR - T Targeting COL6A3 Exon 6 38

ACTengine® IMA204 First - in - Class TCR - T Targeting Tumor Stroma Key Features 39 HLA - A*02 - presented peptide derived from COL6A3 exon 6 Naturally and specifically presented on tumors at high target density 1 : 100 - 700 copies/cell Novel tumor stroma target identified and validated by XPRESIDENT® quant. mass spectrometry platform High - affinity, specific TCR targeting COL6A3 exon 6 Affinity - maturated, CD8 - independent TCR High functional avidity 2 : ~0.01ng/ml Identified and characterized by XCEPTOR® TCR discovery and engineering platform CD8 - independent, next - generation TCR engages both, CD8 and CD4 T cells In vitro anti - tumor activity against target - positive cell lines in CD8 and CD4 T cells Complete tumor eradication in in vivo mouse models Pancreatic Carcinoma – 76% Breast Carcinoma – 77% Stomach Carcinoma – 67% Sarcoma – 63% Colorectal Carcinoma – 60% Esophageal Carcinoma – 60% Squamous NSCLC – 55% Adeno NSCLC – 57% HNSCC – 56% Uterine Carcinosarcoma – 50% Mesothelioma – 44% Cholangiocarcinoma – 36% Melanoma – 35% Bladder Carcinoma – 34% Ovarian Carcinoma – 31% 1 Target density: peptide copy number per tumor cell, approximate range representing the majority of tumor samples analyzed; 2 Functional avidity: EC50 half maximal effective concentration; 3 Solid cancer indications with 20% or more target expression, Target prevalence for selected cancer indications based on mRNA expression (TCGA and Immatics inhouse data) TARGET TCR PREC LINICAL DATA PATIENT POPULATION 3 IMA204 provides a promising therapeutic opportunity for a broad patient population as monotherapy or in combination with TCR - T cells directed against tumor targets IMA204

ACTengine® IMA204 – High Affinity, CD8 - independent TCR Complete Tumor Eradication in vitro & in vivo 1 by Affinity - enhanced IMA204 TCR CD8 - independent TCR leads to tumor eradication in all mice treated 40 Control IMA204 TCR D7 D16 D22 D29 Affinity maturated CD8 - independent, next - generation TCR engages both CD4 and CD8 T cells without the need of CD8 co - transduction Stroma cells Tumor cells Stroma Target (COL6A3 exon 6) in Ovarian Cancer sample Example of a Tumor Target in same Ovarian Cancer sample 1 In vivo data in collaboration with Jim Riley, University of Pennsylvania, control: non - transduced T cells. TCR avidity and specificity d ata not shown, available in IMA204 presentation on Immatics website. COL6A3 exon 6 prevalently expressed at high target density in tumor stroma across many solid cancers IMA204

ACTallo® – Our Next - generation Off - the - shelf TCR - T 41

ACTallo® – Immatics’ Allogeneic Cell Therapy Approach • Off - the - shelf cell therapy , no need for personalized manufacturing reduced logistics and time to application • Potential for hundreds of doses from one single donor leukapheresis lower cost of goods • Use of healthy donor material provides standardized quality and quantity of starting material • Strategic collaborations combining Immatics’ proprietary ACTallo ® platform with Bristol Myers Squibb’s next - gen technologies and Editas Medicine’s CRISPR gene editing technology to develop next - gen allogeneic γδ TCR - T/CAR - T programs 42 ACTallo® γδ T cell Cell Engineering (gene editing & armoring ) γδ T cell Collection from Healthy Donor Expansion Off - the - shelf Products Patient Treatment

Why γδ T cells? γδ T cells Are Well Suited for an Off - the - shelf Cell Therapy Approach 43 γδ T cells x are abundant in the peripheral blood x show intrinsic anti - tumor activity x naturally infiltrate solid tumors & correlate with favorable prognosis x are HLA - independent, thus do not cause graft - vs - host disease in allogeneic setting x can be expanded to high numbers in a cGMP - compatible manner x can be effectively redirected using αβ TCR or CAR constructs In vitro a nti - tumor activity 0 48 96 144 192 0 5 10 15 Hours F o l d G r o w t h ( U 2 0 S - R F P + ) Tumor cells only T cells (NT) T cells IMA203 TCR + T cells (NT) T cells IMA203 TCR + γδ T cells (control) + tumor cells tumor cells only αβ T cells (control) + tumor cells γδ T cells TCR + + tumor cells αβ T cells TCR + + tumor cells ACTallo® 0 5 10 15 20 25 0.001 0.01 0.1 1 10 100 1000 10000 100000 1000000 Day F o l d e x p a n s i o n o f T c e l l s Expansion Fold - growth (target - positive tumor cells)

TCER® – TCR Bispecifics 44

TCER® – Immatics ’ Next - generation, Half - Life Extended Bispecifics Proprietary TCER® Format Consisting of Three Distinct Elements 45 High - affinity TCR domains targeting XPRESIDENT® - selected tumor - specific peptide - HLA molecules Low - affinity T cell recruiter against CD3/TCR Fc part for half - life extension, favorable stability and manufacturability Next - gen, half - life extended TCER® format designed to safely apply high drug doses for activity in a broad range of tumors achieve optimized scheduling 2 1 3 Cytotoxic lytic granules T umor cell killing A ctivated T cell TCER®

TCER® – Immatics’ Next - generation, Half - Life Extended Bispecifics 46 pHLA targeting TCR x High - affinity (single digit nM ) TCR targeting XPRESIDENT® - selected tumor - specific peptide - HLA molecules x Broad therapeutic window through XPRESIDENT® - guided affinity maturation (>1000x) 1 x Complete tumor eradication in mouse xenograft models at low doses T cell recruiting antibody x Low - affinity (triple digit nM ) T cell recruiter against both TCR & CD3 x Optimized biodistribution aiming for enrichment at tumor site and prevention of CRS 2 x Superior anti - tumor activity in mouse models as compared to widely used CD3 recruiters Next - generation TCER® format x Off - the - shelf b iologic with antibody - like manufacturability 3 and low cost of goods x Superior anti - tumor activity 4 compared to six alternative bispecific formats x Half - life of several days expected in humans Our TCER® format is designed to maximize efficacy while minimizing toxicities in patients 1 As compared to natural TCR; 2 Based on literature data for other low - affinity recruiters (e.g. Harber et al ., 2021, Nature; Trinklein et al ., 2019, mAbs ) ; 3 Production in mammalian cells (CHO cells); 4 Based on preclinical testing TCER® 1 2 3

Potency of Our Proprietary TCR Bispecific Format TCER® 47 • Seven different TCR Bispecific formats were evaluated with a pHLA targeting TCR and the identical T cell recruiting antibody • TCER® format had higher combination of potency and specificity 1 than six alternative TCR Bispecific format designs evaluated Flexible Plug - and - play platform: TCER® format successfully validated for different TCRs & different T cell recruiting antibodies TCER® TCER® 2+1 TCR bispecific format: High potency was linked to a significantly reduced specificity profile Killing of target - positive cells by different TCR Bispecifics 1 Preclinical data on specificty not shown

TCER® Format Is Designed for Optimized Efficacy and Safety Superior Tumor Control Using a Novel, Low - Affinity Recruiter 48 Widely used T cell recruiting Ab (3 variants) medium to high affinity (single to double digit nM ) n = 6 mice/treatment group, n = 10 mice in vehicle group, 2 donors/group Dose: 0.025 mg/kg Proprietary, low - affinity T cell recruiting region demonstrates superior tumor control compared to analogous TCER® molecules designed with higher - affinity variants of a widely used recruiter Immatics’ T cell recruiting Ab low affinity (triple digit nM ) TCER® Tumor Model in Mice 1 1 Hs695T xenograft model in NOG m ice , tumor volume of group means shown

TCER® Format Is Designed for Optimized Efficacy and Safety Reduced Target - Unrelated Recruiter - Mediated Cytokine Release using a Low - Affinity Recruiter 49 TCER® Whole blood cytokine release assay N= 3 HLA - A*02 - positive donors N=16 cytokines tested, 4 exemplary cytokines shown

Our TCER® Portfolio Broad Pipeline of Next - Gen Half - Life Extended TCR Bispecifics 50 TCER® • PRAME peptide presented by HLA - A*02:01 • Start of clinical trial in Aug 2023, first clinical data expected 2024 IMA402 Potential for addressing different indications and large patient populations with novel, off - the - shelf TCR Bispecifics • MAGEA4/8 peptide presented by HLA - A*02:01 • Dose escalation ongoing, first clinical data expected 2024 IMA401 • Undisclosed peptides presented by HLA - A*02:01 and other HLA - types • TCER® engineering and preclinical testing ongoing IMA40x Several innovative programs CLINICAL PRECLINICAL

TCER® IMA401 Targeting MAGEA4/8 Homogeneous Expression, Broad Prevalence and High Copy Number Target 51 MAGEA4 RNA detection in tumor samples (ISH) Indications Target p revalence [%] Squamous non - small cell lung carcinoma 52% Head and neck squamous cell carcinoma 36% Bladder carcinoma 29% Uterine carcinosarcoma 29% Esophageal carcinoma 23% Ovarian carcincoma 23% Melanoma 18% plus several further indications MAGEA4/8 target prevalence in selected cancer indications MAGEA4/8 target prevalences are based on TCGA data combined with a XPRESIDENT® - determined target individual MS - based mRNA expression threshold; 1 Copy number per tumor cell (CpC) measured on a paired - sample basis by AbsQuant®, i.e. comparing MAGEA4 vs. MAGEA4/A8 peptide presentation on same sample, 2 Students paired T test IMA401 p<0.001 2 MAGEA4/8 target is presented at >5 - fold higher target density 1 than a commonly used MAGEA4 target peptide
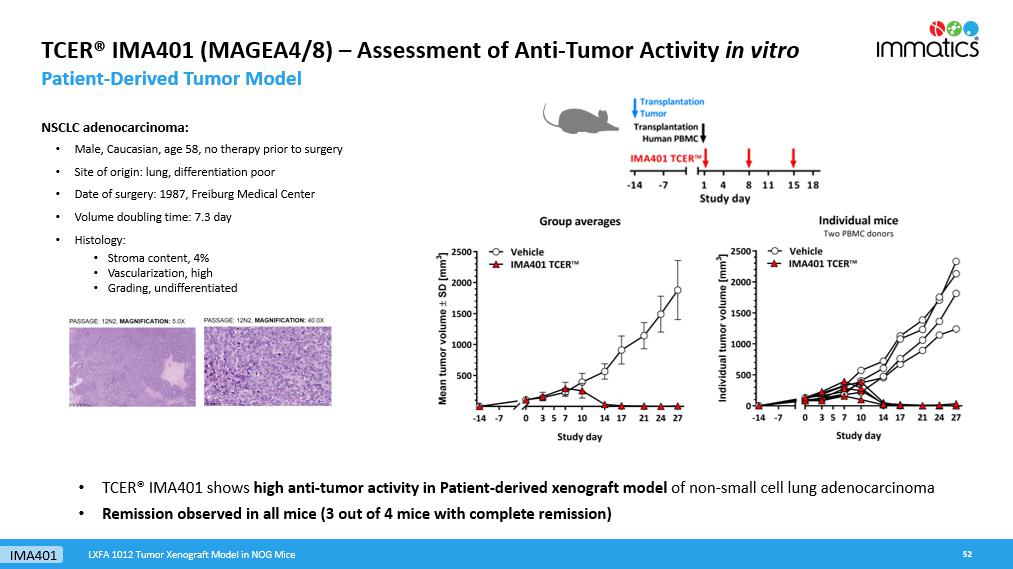
TCER® IMA401 (MAGEA4/8) – Assessment of Anti - Tumor Activity in vitro Patient - Derived Tumor Model 52 NSCLC adenocarcinoma : • M ale, Caucasian, age 58, no therapy prior to surgery • Site of origin: lung, differentiation poor • Date of surgery: 1987, Freiburg Medical Center • Volume doubling time: 7.3 day • Histology: • Stroma content, 4% • Vascularization, high • Grading, undifferentiated • TCER® IMA401 shows high anti - tumor activity in Patient - derived xenograft model of non - small cell lung adenocarcinoma • Remission observed in all mice (3 out of 4 mice with complete remission) LXFA 1012 Tumor Xenograft Model in NOG Mice IMA401
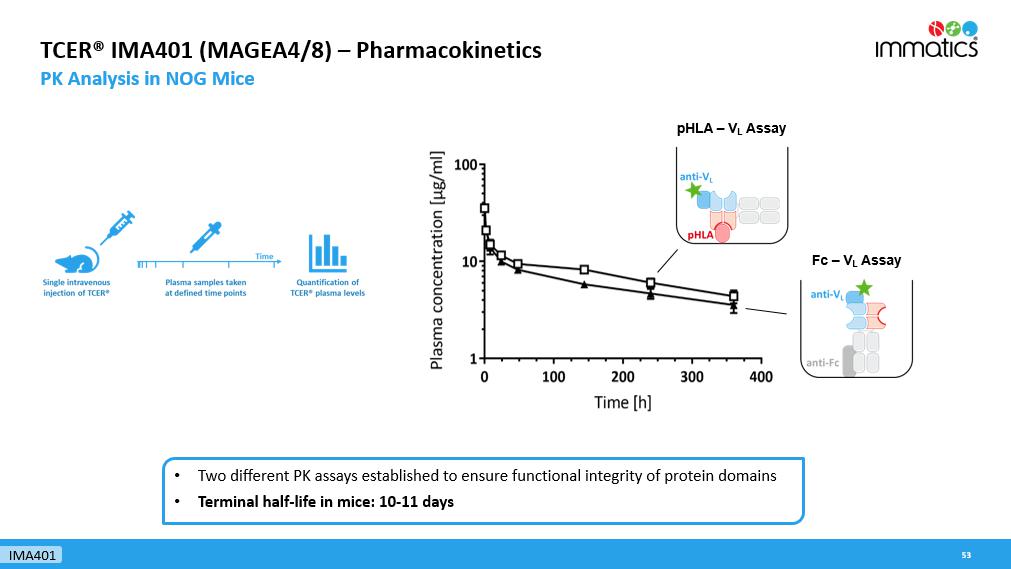
53 TCER® IMA401 (MAGEA4/8) – Pharmacokinetics PK Analysis in NOG Mice • Two different PK assays established to ensure functional integrity of protein domains • Terminal half - life in mice: 10 - 11 days pHLA – V L Assay Fc – V L Assay IMA401

Phase 1 Clinical Trial to Evaluate TCER® IMA401 Targeting MAGEA4/8 54 MTD: maximum tolerated dose, RP2D: recommended phase 2 dose; MABEL: minimum anticipated biological effect level; BLRM: Bayesian logistic regression model; 1 P harmacokinetics data assessed throughout the trial might provide an opportunity to optimize scheduling to a less frequent regimen. 2 Conducted in collaboration with BMS Phase 1a: Dose Escalation Phase 1b: Dose Expansion • Weekly i.v. infusions 1 • Dose escalation decisions based on cohorts of 1 - 6 patients in adaptive design (BLRM model) MTD/ RP2D Adaptive design aimed at accelerating dose escalation • Focus on specific indications planned Potential development option for checkpoint inhibitor combination or other combination therapies 2 Monotherapy expansion cohort Primary Objective • Determine MTD and/or RP2D Secondary Objectives • Safety and tolerability • Initial anti - tumor activity • Pharmacokinetics IMA401

TCER® IMA402 Targeting PRAME – Efficacy Assessment in vitro Tumor Cell Killing at Low Physiological PRAME Peptide Levels 55 0 20 40 60 80 100 120 140 10 -1 10 0 10 1 10 2 10 3 10 4 10 5 IMA402 [pM] Cytotoxicity [%] ~50 PRAME CpCs 0 0 20 40 60 80 100 120 140 10 -1 10 0 10 1 10 2 10 3 10 4 10 5 IMA402 [pM] Cytotoxicity [%] Target-negative 0 0 20 40 60 80 100 120 140 10 -1 10 0 10 1 10 2 10 3 10 4 10 5 IMA402 [pM] Cytotoxicity [%] ~110 PRAME CpCs 0 0 20 40 60 80 100 120 140 10 -1 10 0 10 1 10 2 10 3 10 4 10 5 IMA402 [pM] Cytotoxicity [%] ~250 PRAME CpCs 0 • TCER® IMA402 induces killing of tumor cells with PRAME target copies as low as 50 CpCs • Physiological PRAME levels detected in majority of cancer tissues from patients are 100 – 1000 CpCs • Preclinical activity profile enables targeting of a broad variety of tumor indications, such as lung cancer, breast cancer, ovarian cancer, uterine cancer, melanoma and others IMA402 CpC: Target peptide copy numbers per tumor cell

TCER® IMA402 Achieves Durable Tumor Control of Large Tumors in vivo 56 -29 0 500 1000 1500 2000 2500 0 10 20 30 40 50 60 70 Study day M e d i a n t u m o r v o l u m e [ m m 3 ] Vehicle IMA402 [0.01 mg/kg] IMA402 [0.05 mg/kg] IMA402 [0.25 mg/kg] • Dose - dependent efficacy of IMA402 in cell line - derived in vivo mouse model • Durable shrinkage of large tumors including complete responses over prolonged period • Sufficiently high drug doses are key to achieving desired anti - tumor effect IMA402

Half - life Extended Format of IMA402 Confers Terminal Half - life of >1 Week 57 pHLA – aV L Assay pHLA – aFc Assay • IMA402 shows a terminal serum half - life of ≈ 8 days in mice • IMA402 will be initially dosed weekly in the clinical trial • Dosing frequency may be adapted based on clinical data IMA402

Phase 1/2 Clinical Trial to Evaluate TCER® IMA402 Targeting PRAME First Clinical Data Planned in 2024 58 Phase 1: Dose Escalation Phase 2a: Dose Expansion Adaptive design aimed at accelerating dose escalation • Specific indications plus ongoing basket • Combination therapies • Optional dose/application optimization Expansion cohort Expansion cohort Expansion cohort Trial Overview Phase 1/2 clinical trial to evaluate safety, tolerability and anti - tumor activity of IMA402 • HLA - A*02:01 - positive patients with PRAME - expressing recurrent and/or refractory solid tumors • Initially weekly i.v. infusions • Potential for early adjustment of treatment interval based on PK data of half - life extended TCER® format MTD/ RP2D IMA402 • Basket trial in focus indications to accelerate signal finding • Ovarian cancer, lung cancer, uterine cancer, melanoma, others

Immatics’ Proprietary Target and TCR Discovery Platforms 59

True Cancer Targets & Matching Right TCRs Goal to Maximize Anti - Tumor Activity and Minimize Safety Risks of TCR - based Immunotherapies 60 True Targets via XPRESIDENT® technology platform • are naturally presented on tumor tissues as identified by mass - spec • are absent or presented at only low levels on normal tissues • are presented at high copy numbers to trigger a pharmacological response + Technology Right TCRs via XCEPTOR® technology platform • recognize the target peptide with high affinity and specificity • show selective killing of tumor cells • are developed to be suitable for two different therapeutic modalities, Cell Therapies and TCR Bispecifics

Technology Pool of 200 Prioritized Targets as Foundation for Future Value Generation XPRESIDENT® Target Platform 61 200 Prioritized Targets Grouped in 3 Target Classes: 1. Well known and characterized parent protein (20%) e.g. MAGE family cancer testis antigens 2. Unknown or poorly characterized parent protein (60%) e.g. stroma target COL6A3 exon 6 3. Crypto - targets/Neoantigens (20%) Novel target class which includes RNA - edited peptides & non - classical neoantigens ~50% of our prioritized targets are non - HLA - A*02 restricted, substantially broadening the potential patient reach >2,500 cancer & normal tissues a nalyzed by Quantitative, Ultra - Sensitive Mass Spectrometry pHLA Database based on primary tissues >200 prioritized targets This large data set is leveraged by our bioinformatics & AI - platform XCUBE Ρ – „AI is where the data is ®“

Immatics ’ Unique Capability – Identification of the most Relevant Target Example of MAGEA4/8 Peptide Target 62 1 Copy number per tumor cell (CpC) measured on a paired - sample basis by AbsQuant®, i.e. comparing MAGEA4 vs. MAGEA4/A8 peptide pre sentation on same sample, 2 Students paired T test p<0.001 2 Technology MAGEA4/8 target is presented at >5 - fold higher target density 1 than a commonly targeted MAGEA4 target peptide XPRESIDENT® quantitative information on target density 1 between peptides originating from the same source protein Ranking of pHLA targets Commonly targeted

Development of the Right TCR – XCEPTOR® Technology TCR Discovery and Engineering for ACT and TCR Bispecifics 63 TCR Bispecifics T cell engaging receptor (TCER®) Adoptive Cell Therapy ACTengine® ACTallo ® • Fast, efficient and highly sensitive discovery of highly specific, natural TCRs • Protein engineering capabilities to design and maturate TCRs with increased affinity while retaining specificity • Early de - selection of cross - reactive TCRs by the u nique interplay between Immatics’ target and TCR discovery platforms XPRESIDENT® and XCEPTOR® during TCR discovery 1 and TCR maturation 2 (empowered by our bioinformatics & AI - platform XCUBE Ρ ) Micromolar affinity Nanomolar affinity Technology 1 XPRESIDENT® - guided off - target toxicity screening; 2 XPRESIDENT® - guided similar peptide counterselection

Optimal Target Selection & TCR Specificity for Minimizing Safety Risks Unique Interplay between Technology Platforms Allows Early De - risking for Clinical Development 64 Target peptide presented on tumor cells Selective killing of tumor cells Target peptide presented on normal cells Off - target toxicity On - target (off - tumor) toxicity A different HLA is recognized on normal cells Alloreactivity Similar peptide presented on normal cells 1 XPRESIDENT® - guided screening for on - and off - target toxicities of TCRs based on the extensive database of peptides presented on normal tissues Technology 1 Clinical fatalities have occurred in TCR - T trials using a titin cross - reactive TCR (Cameron et al ., Sci Transl Med)

“AI Is Where the Data Is®” Bioinformatics and AI - Platform XCUBE Ρ 65 Data Engineering Development of data warehouses & user interfaces Data Science Development of statistical & machine learning models Data Processing Processing of mass - spec & next - gen sequencing data 1 THERAPEUTIC KNOWLEDGE XPRESIDENT®/ XCEPTOR® DATA Data Engineering Data Science Data Processing 2 3 1 Cell therapies Bispecifics CDx Therapies Targets Lead Molecules Discovery Characterization Discovery Selection Validation 2 3

Robust IP Portfolio Immatics’ Patent Estate – Territorial Coverage 66 Cancer targets, TCRs and technology protected by: • 5,800 applications and patents filed in all major countries and regions • >115 patent families • >2,400 granted patents, thereof >550 granted patents in the US Technology

Corporate Information & Milestones 67

David Leitner Schuldirektor David Leitner Schuldirektor David Leitner Schuldirektor Harpreet Singh Chief Executive Officer Co - Founder >20 yrs biotech experience Arnd Christ Chief Financial Officer >20 yrs biotech experience ( InflaRx , Medigene , NovImmune , Probiodrug ) Carsten Reinhardt Chief Development Officer >20 yrs pharma & biotech experience ( Micromet , Roche, Fresenius) Cedrik Britten Chief Medical Officer 15 yrs pharma & biotech experience (GSK, BioNTech) Rainer Kramer Chief Business Officer 25 yrs pharma & biotech experience (Amgen, MorphoSys , Jerini , Shire, Signature Dx) Steffen Walter Chief Operating Officer Co - Founder Immatics US >15 yrs biotech experience Edward Sturchio General Counsel >15 yrs pharma & biotech experience ( Abeona Therapeutics, AAA, Novartis, Merck, Schering) ) Jordan Silverstein Head of Strategy >10 yrs biotech experience ( InflaRx , AAA) Toni Weinschenk Chief Innovation Officer Co - Founder >15 yrs biotech experience Experienced Global Leadership Team Across Europe and the US Corporate

Strong, Focused and Highly Integrated Trans - Atlantic Organization 69 Houston, Texas ~ 150 FTEs Cell therapy development & manufacturing Munich, Germany ~ 65 FTEs Various operating functions Tübingen, Germany ~ 215 FTEs Target & TCR discovery and TCR Bispecifics developme nt Corporate FTE status as of December 2022

Delivering s the Power of T cells to Cancer Patients © Immatics. Not for further reproduction or distribution. www.immatics.com Appendix

IMA203 GEN1 in Phase 1a Dose Escalation (N=27 # ) – BOR and Response over Time 71 * Maximum change of target lesions and RECIST 1.1 BOR at different timepoints ; # Synovial sarcoma patient (DL3) PD at week 6 not shown as t arget lesions were not evaluable; PD: Progressive disease; SD: Stable disease; PR: Partial response; cPR : Confirmed partial response; BL: Baseline Best overall response (RECIST1.1) Data cut - off Sep 30, 2023 IMA203 GEN1

* IMA203 GEN1 in Cohort A (N=18) – BOR and Response over Time Objective Responses across Multiple Solid Cancer T ypes 72 1 Patient received one dose nivolumab erroneously; 2 Progressive disease at month 6 due to unequivocal progression of non - target lesions, target lesions not evaluable due to externa l assessment ; Initial ORR: Objective response rate according to RECIST 1.1 at any post infusion scan; Confirmed ORR ( cORR ): Confirmed objective response rate according to RECIST 1.1 for patients with at least two available post infusion scans or pat ients with progressive disease (PD) at any prior timepoint, patients with ongoing unconfirmed PR not included in cORR calculation; Duration of response (DOR) in confirmed responders is defined as time from first documented response until disease progressio n/d eath. Patients with ongoing response will be censored at date of data cut - off. Median DOR is analyzed by using the Kaplan - Meier method; Median Follow - up is analyzed by using the reverse Kaplan - Meier method; PD: Progressive Disease; SD: Stable Disease; PR: Partial Response; cPR : Confirmed Partial Response; BL: Baseline; BOR: Best Overall Response; DOR: Duration of Response Data cut - off Sep 30, 2023 Median DOR, min, max DOR Not reached, 2.2+, 14.7+ months Median Follow - up 10.8 months Scans at approximately week 6, month 3 and then every 3 months Ongoing ORR 50% (9/18) cORR 47% (8/17) * Response until 5.7 months post infusion, target lesion response assessment not available (external assessment) IMA203 GEN1

73 Data cut - off Sep 30, 2023 IMA203 GEN1 in Cohort A – Most Frequent Adverse Events N=21 Patients in Safety Population 1 • Expected cytopenia (Grade 1 - 4) associated with lymphodepletion in all patients • Mild - moderate cytokine release syndrome (CRS) in 90% (19/21) of patients • 43% (9/21) with Grade 1 CRS • 48% (10/21) with Grade 2 CRS • No dose - dependent increase of CRS • O ne non - serious, mild (Grade 1) ICANS 2 in DL5 • No dose - limiting toxicity • No IMA203 - related deaths 1 Three cutaneous melanoma patients treated with IMA203, and pending post infusion scan included in safety population, but not ef ficacy population; 2 I CANS: Immune Effector Cell - Associated N eurotoxicity S yndrome ; CRS and ICANS graded by CARTOX criteria ( Neelapu et al ., 2018) IMA203 GEN1 monotherapy continues to be well tolerated at total doses between 1 - 10x10 9 TCR - T cells (RP2D) IMA203 GEN1

IMA203 GEN1 at RP2D – Tolerability Data Phase 1a DL4 and Cohort A – All ≥Grade 3 Adverse Events (N=28) 74 • IMA203 was well tolerated at doses as high as ~10x10 9 TCR - T cells • Most frequent ≥Grade 3 AEs were expected cytopenia associated with lymphodepletion • No IMA203 - related Grade 5 AEs All treatment - emergent adverse events (TEAEs) with ≥ Grade 3 regardless of relatedness to study treatment that occurred in at least 1 patient (except for ICANS, where only Grade 1 - 2 occurred ; listed for completeness due to being an adverse event of special interest) are presented . Adverse events were coded using the Medical Dictionary for Regulatory Activities . Grades were determined according to National Cancer Institute Common Terminology Criteria of Adverse Events, version 5 . 0 . Grades for CRS and ICANS were determined according to CARTOX criteria ( Neelapu et al . , 2018 ) . Patients are counted only once per adverse event and severity classification . Based on interim data extracted from open clinical database ( 30 - Sep - 2023 ) ; 1 One patient in Phase 1 a DL 4 with disease progression after first IMA 203 infusion received exploratory second IMA 203 infusion and had these ≥ Grade 3 TEAEs only after second infusion, which are included in the table : Humerus fracture, Muscle spasms, Neutropenia, Thrombocytopenia ; 2 ICANS : Immune effector cell - associated neurotoxicity syndrome ; 3 Fatal Adverse events were not considered related to any study drug Adverse event ( System organ class , Preferred term ) ≥ Grade 3 No . % Patients with any adverse event 28 100.0 Adverse Events of Special Interest 1 3.6 Cytokine release syndrome 1 3.6 ICANS 2 0 0.0 Blood and lymphatic system disorders 27 96.4 Neutropenia 18 64.3 Anaemia 14 50.0 Leukopenia 13 46.4 Lymphopenia 11 39.3 Thrombocytopenia 9 32.1 Leukocytosis 1 3.6 Lymphocytosis 1 3.6 Investigations 7 25.0 Neutrophil count decreased 4 14.3 Alanine aminotransferase increased 2 7.1 Aspartate aminotransferase increased 2 7.1 White blood cell count decreased 2 7.1 Blood alkaline phosphatase increased 1 3.6 Infections and infestations 3 10.7 Infection 1 3.6 Septic shock 3 1 3.6 Urinary tract infection 1 3.6 Respiratory, thoracic and mediastinal disorders 3 10.7 Hypoxia 2 7.1 Laryngeal inflammation 1 3.6 Vascular disorders 3 10.7 Hypotension 2 7.1 Hypertension 1 3.6 Metabolism and nutrition disorders 2 7.1 Failure to thrive 1 3.6 Hypokalaemia 1 3.6 Hypophosphataemia 1 3.6 Eye disorders 1 3.6 Ulcerative keratitis 1 3.6 Adverse event ( System organ class , Preferred term ) ≥ Grade 3 No . % table continued… General disorders and administration site conditions 1 3.6 Pyrexia 1 3.6 Hepatobiliary disorders 1 3.6 Cholangitis 1 3.6 Injury, poisoning and procedural complications 1 3.6 Humerus fracture 1 3.6 Musculoskeletal and connective tissue disorders 1 3.6 Muscle spasms 1 3.6 Nervous system disorders 1 3.6 Headache 1 3.6 Skin and subcutaneous tissue disorders 1 3.6 Rash maculo - papular 1 3.6 TEAEs by maximum severity for all patients in Ph1a dose escalation DL4 and Ph1b Cohort A dose expansion ( RP2D, N=28) 1 Data cut - off Sep 30, 2023 IMA203 GEN1

Delivering s the Power of T cells to Cancer Patients © Immatics. Not for further reproduction or distribution. www.immatics.com
Immatics NV (NASDAQ:IMTX)
Historical Stock Chart
From Mar 2024 to Apr 2024
Immatics NV (NASDAQ:IMTX)
Historical Stock Chart
From Apr 2023 to Apr 2024