Autolus Therapeutics plc (Nasdaq: AUTL), a clinical-stage
biopharmaceutical company developing next-generation programmed T
cell therapies, announces the online publication of four abstracts
submitted to the American Society of Hematology (ASH) Annual
Meeting, to be held from December 7-10, 2024, in San Diego.
“The FELIX study’s rich data set continues to
provide important information in shaping our understanding of the
use of obe-cel to treat adult r/r B-ALL patients,” said Dr.
Christian Itin, Chief Executive Officer of Autolus. “We
are presenting additional data at ASH that suggests deep molecular
remission that may predict better outcomes; shows the impact of
bridging therapy on outcomes; highlights the costs associated with
managing CRS and ICANS; and how using hematotoxicity scores can
help identify patients who are more likely benefit from treatment
with obe-cel.”
Abstract 194508 – Oral
presentation: Title: Obecabtagene autoleucel
(obe-cel) for Adult Relapsed/Refractory B-Cell Acute Lymphoblastic
Leukemia (R/R B-ALL): Deep Molecular Remission May Predict Better
OutcomesSession Name: 613. Acute
Lymphoblastic Leukemias: Therapies Excluding Allogeneic
Transplantation: Risk Stratification and CAR-T
TherapiesSession date and time: Monday, December
9, 2024; 4:30 PM - 6:00 PM PTPresentation Time:
5:00 PMSession room: Marriott Marquis San Diego
Marina, Marriott Grand Ballroom 5-6Publication
Number: 963Presenting Author: Dr.
Elias Jabbour, Professor, Department of Leukemia, Division of
Cancer Medicine, MD Anderson Cancer Center, Houston, TX
Summary: In this session we
report on the correlation between depth of measurable residual
disease (MRD)-negative remission and clinical outcomes in patients
treated with obe-cel. Data demonstrated that 84% of responders for
whom MRD by next-generation sequencing (NGS) could be analyzed
achieved MRD <10–6 leukemic cells which was associated with more
durable responses, and higher event free survival (EFS) and overall
survival (OS) rates than those observed in patients with MRD ≥10–4
and between 10–4 and 10–6 leukemic cells. Patients who did not
achieve MRD <10–6 had poorer outcomes.
Abstract 201514 – Poster
presentation:Title: Obecabtagene autoleucel
(obe-cel) for Adult Relapsed/Refractory B-Cell Acute Lymphoblastic
Leukemia (R/R B-ALL) in the Open-Label, Multi-Center, Global,
Single-Arm, Phase Ib/II FELIX study: The Impact of Bridging
Therapies on CAR T-Cell Expansion and
PersistenceSession Name: 704. Cellular
Immunotherapies: Early Phase Clinical Trials and Toxicities: Poster
II. Session date and time: Sunday, December
8, 2024; 6:00 PM - 8:00 PM PTSession room: San
Diego Convention Center, Halls G-HPublication
Number: 3458Presenting Author: Dr.
Jae H Park, Leukemia Specialist & Cellular Therapist, Memorial
Sloan Kettering Cancer Center, New York, NY, USA
Summary: Patients in the FELIX
study received bridging therapy (BT) (chemotherapy with or without
Inotuzumab ozogamicin (INO) or Tyrosine kinase inhibitors (TKI),
single-agent INO, single-agent TKI, steroids, or rituximab) per
investigator decision; use of blinatumomab as a BT agent was not
permitted. Analysis of BT indicated that INO is effective in
reducing disease burden prior to obe-cel infusion. No apparent
differences in expansion and long-term persistence of obe-cel were
observed based on any of the BT evaluated, suggesting that
long-term persistence of obe-cel is possible irrespective of BT and
independent of initial tumor burden at LD. Reduction in tumor
burden at LD through BT with INO led to more favorable survival
outcomes compared with BT without INO, while maintaining a
tolerable safety profile. A limitation of this study is the small
number of patients who received BT with INO. Further studies
comparing BT with INO-containing therapies or chemotherapy are
warranted.
Abstract
205694 – Poster
presentation:Title: Healthcare Resource
Utilization and Costs Associated with Managing CRS and ICANS in
Patients with Relapsed/Refractory Adult B-Cell Acute Lymphoblastic
Leukemia Receiving Obecabtagene autoleucel (obe-cel)
Session Title: 704. Cellular Immunotherapies:
Early Phase Clinical Trials and Toxicities: Poster III
Session date and time: Monday, December 9,
2024; 6:00 PM - 8:00 PM PTSession room: San Diego
Convention Center, Halls G-HPublication
Number: 4837Presenting Author: Dr.
Bijal D Shah, Associate Member in the Department of Malignant
Hematology Moffitt Cancer Center, Tampa, FL, USA
Summary: A secondary analysis
of the data from the FELIX study was conducted to evaluate
Facility-Related Healthcare Resource Utilization (HCRU) as a result
of cytokine release syndrome (CRS) and immune effector
cell–associated neurotoxicity syndrome (ICANS) and estimate the
overall costs for managing these adverse events (AEs) among
patients with r/r B-ALL. HCRU for patients with treatment-emergent
CRS and/or ICANS was monitored for 6 months post obe-cel
administration. Data from the analysis demonstrated that management
costs for CRS and ICANS events generally increase with severity,
but these events were rare in the FELIX study. Of note,
medication usage (in particular tocilizumab) and
hospitalization/intensive care unit (ICU) costs were key drivers of
overall CRS and/or ICANS management costs.
Abstract 208028 – Poster
presentation:Title: Risk Factors
Associated with Sub-Optimal Outcomes Following Obecabtagene
autoleucel (obe-cel) for Relapsed/Refractory B-Cell Acute
Lymphoblastic Leukemia (R/R B-ALL): What We Have Learned from the
FELIX TrialSession Name: 704. Cellular
Immunotherapies: Early Phase Clinical Trials and Toxicities: Poster
IIISession date and time: Monday, December 9,
2024; 6:00 PM - 8:00 PM PTSession room: San Diego
Convention Center, Halls G-HPublication
Number: 4845Presenting Author: Dr.
Claire Roddie, MD, PhD, FRCPath, Associate Professor Haematology
and Honorary Consultant Haematologist, Cancer Institute, University
College London (UCL)
Summary: Immune effector
cell-associated hematotoxicity is the most common side effect of
CAR T therapy but the pathophysiology of prolonged hematotoxicity
is poorly understood and the lack of consensus for its treatment
presents challenges. The CAR-HEMATOTOX (HT) model was developed in
large B-cell lymphoma for risk-stratifying patients prior to CAR T
therapy for hematotoxicity and outcomes. Using the HT model from
the analysis from the study, the HT score was found to be
correlated with disease burden. Risk-stratification for
hematotoxicity, using pre-lymphodepletion clinical parameters,
together with disease burden, has the potential to be a useful tool
for identifying patients more likely to benefit from obe-cel
treatment and experience reduced toxicity. Patients with high-risk
HT scores had consistently worse outcomes than patients with
low-risk HT scores, leading to the view that further studies are
warranted.
About Autolus Therapeutics
plcAutolus is a clinical-stage biopharmaceutical company
developing next-generation, programmed T cell therapies for the
treatment of cancer and autoimmune disease. Using a broad suite of
proprietary and modular T cell programming technologies, Autolus is
engineering precisely targeted, controlled and highly active T cell
therapies that are designed to better recognize target cells, break
down their defense mechanisms and eliminate these cells. Autolus
has a pipeline of product candidates in development for the
treatment of hematological malignancies, solid tumors and
autoimmune diseases. For more information, please visit
www.autolus.com
About
obe-cel (AUTO1)Obecabtagene autoleucel (obe-cel) is a
B-lymphocyte antigen CD19 (CD19) chimeric antigen receptor (CAR) T
cell investigational therapy designed to overcome the limitations
in clinical activity and safety compared to current CD19 CAR T cell
therapies. Obe-cel is designed with a fast target binding
off-rate to minimize excessive activation of the programmed T
cells. In clinical trials of obe-cel, this “fast off-rate” profile
reduced toxicity and T cell exhaustion, resulting in improved
persistence and leading to high levels of durable remissions in
relapsed/refractory (r/r) Adult B-cell Acute Lymphoblastic Leukemia
(B-ALL) patients. The results of the FELIX trial, a pivotal trial
for adult B-ALL, have been submitted and accepted by the FDA with a
PDUFA target action date of November 16, 2024. In the EU a
regulatory submission to the EMA was accepted in April 2024, while
in the UK, an MAA was submitted to MHRA in July 2024. In
collaboration with Autolus’ academic partner, University College
London, obe-cel is currently being evaluated in a Phase 1 clinical
trial for B-cell non-Hodgkin lymphoma (B-NHL).
About obe-cel
FELIX clinical trialAutolus’ Phase 1b/2 clinical
trial of obe-cel enrolled adult patients with r/r B-precursor ALL.
The trial had a Phase 1b component prior to proceeding to the
single arm, Phase 2 clinical trial. The primary endpoint was
overall response rate, and the secondary endpoints included
duration of response, MRD negative complete remission rate and
safety. The trial enrolled over 100 patients across 30 of the
leading academic and non-academic centers in the United
States, United Kingdom and Europe. [NCT04404660]
Forward-Looking StatementsThis
press release contains forward-looking statements within the
meaning of the "safe harbor" provisions of the Private Securities
Litigation Reform Act of 1995. Forward-looking statements are
statements that are not historical facts, and in some cases can be
identified by terms such as "may," "will," "could," "expects,"
"plans," "anticipates," and "believes." These statements include,
but are not limited to, statements regarding Autolus’ development
and commercialization of its product candidates, timing of data
announcements and regulatory submissions, its cash resources and
the market opportunity for obe-cel. Any forward-looking statements
are based on management's current views and assumptions and involve
risks and uncertainties that could cause actual results,
performance, or events to differ materially from those expressed or
implied in such statements. These risks and uncertainties include,
but are not limited to, the risks that Autolus’ preclinical or
clinical programs do not advance or result in approved products on
a timely or cost effective basis or at all; the results of early
clinical trials are not always being predictive of future results;
the cost, timing and results of clinical trials;that many product
candidates do not become approved drugs on a timely or cost
effective basis or at all; the ability to enroll patients in
clinical trials; and possible safety and efficacy concerns. For a
discussion of other risks and uncertainties, and other important
factors, any of which could cause Autolus’ actual results to differ
from those contained in the forward-looking statements, see the
section titled "Risk Factors" in Autolus' Annual Report on Form
10-K filed with the Securities and Exchange Commission, or the SEC,
on March 21, 2024 as well as discussions of potential risks,
uncertainties, and other important factors in Autolus' subsequent
filings with the Securities and Exchange Commission. All
information in this press release is as of the date of the release,
and Autolus undertakes no obligation to publicly update any
forward-looking statement, whether as a result of new information,
future events, or otherwise, except as required by law. You should,
therefore, not rely on these forward-looking statements as
representing Autolus’ views as of any date subsequent to the date
of this press release.
Contact:
Olivia Manser+44 (0) 7780 471
568o.manser@autolus.com
Julia Wilson+44 (0) 7818
430877j.wilson@autolus.com
Susan A. NoonanS.A. Noonan
Communications+1-917-513-5303susan@sanoonan.com
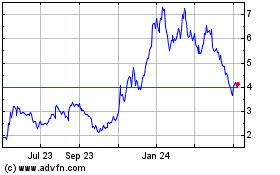
Autolus Therapeutics (NASDAQ:AUTL)
Historical Stock Chart
From Jan 2025 to Feb 2025
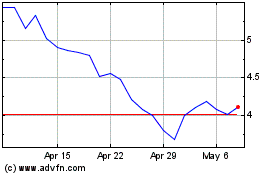
Autolus Therapeutics (NASDAQ:AUTL)
Historical Stock Chart
From Feb 2024 to Feb 2025