In the MCL cohort of TRANSCEND NHL 001,
Breyanzi delivered responses in 85.3% of patients with a one-time
infusion while demonstrating a consistent safety profile across
clinical trials
Breyanzi is the only CAR T cell therapy
approved by the FDA for four distinct subtypes of non-Hodgkin
lymphoma, bringing this personalized therapy to the broadest array
of patients with B-cell malignancies
Bristol Myers Squibb (NYSE: BMY) today announced the U.S. Food
and Drug Administration (FDA) has granted approval for Breyanzi®
(lisocabtagene maraleucel; liso-cel), a CD19-directed chimeric
antigen receptor (CAR) T cell therapy, for the treatment of adult
patients with relapsed or refractory mantle cell lymphoma (MCL) who
have received at least two prior lines of systemic therapy,
including a Bruton tyrosine kinase (BTK) inhibitor. This FDA
approval marks the fourth distinct subtype of non-Hodgkin lymphoma
for which Breyanzi is approved, making it the CAR T cell therapy
available to treat the broadest array of B-cell malignancies. In
relapsed or refractory MCL, Breyanzi is delivered as a one-time
infusion* with a single dose containing 90 to 110 x 106
CAR-positive viable T cells. Please see the Important Safety
Information section below, including Boxed WARNINGS for
Breyanzi regarding Cytokine Release Syndrome (CRS), Neurologic
Toxicities, and Secondary Hematological Malignancies.
This press release features multimedia. View
the full release here:
https://www.businesswire.com/news/home/20240523741069/en/
Product image for download (Photo:
Bristol Myers Squibb)
“With Breyanzi, we are delivering on the promise of cell therapy
by offering a definitive treatment option for some of the most
difficult-to-treat lymphomas,” said Bryan Campbell, senior vice
president, Head of Commercial, Cell Therapy, Bristol Myers Squibb.
“We are proud of the advances we are making to bring our
differentiated CAR T cell therapy to the most patients across
indications and lines of therapy to ensure treatment options that
provide improved outcomes are available when most needed.”
MCL is a rare but aggressive form of non-Hodgkin lymphoma, and
many patients relapse or become resistant to frontline therapies.
Currently, MCL is considered an incurable disease, and response
rates and duration of response tend to decrease with each
additional relapse.
“There have been few advances in the treatment of relapsed or
refractory MCL, and prognosis worsens for patients after each
subsequent relapse, often leaving them with high disease burden and
difficulty achieving deep and durable responses,” said Michael
Wang, M.D., lead investigator and Puddin Clarke Endowed Professor,
Department of Lymphoma and Myeloma, Division of Cancer Medicine,
University of Texas MD Anderson Cancer Center, Houston, Texas. “The
approval of Breyanzi offers an important new CAR T treatment option
with high rates of lasting responses and a consistent safety
profile, which is critically important for these patients who
currently have limited options to treat this aggressive
disease.”
The approval of Breyanzi is based on results from the MCL cohort
of TRANSCEND NHL 001, which enrolled adults with relapsed or
refractory MCL who had previously received at least two or more
prior lines of therapy, including a BTK inhibitor. Based on the
U.S. Prescribing Information (USPI), in patients treated with
Breyanzi and evaluated for efficacy (n=68), 85.3% (95% CI:
74.6-92.7) responded to treatment, with 67.6% (95% CI: 55.2-78.5)
achieving a complete response (CR). Responses were assessed per the
2014 Lugano classification and required bone marrow biopsy to
confirm CR. Responses were rapid and durable with a median time to
response of one month (range: 0.7-3) and median duration of
response of 13.3 months (95% CI: 6.0-23.3) with a median follow-up
of 22.2 months (95% CI: 16.7-22.8). More than half (51.4%; 95% CI:
37.5-63.7) of responders remained in response at 12 months, and
38.8% (95% CI: 25-52.4) of responders remained in response at 18
months. Results from the primary analysis published in the Journal
of Clinical Oncology (JCO) (n=83; DL1 + DL2) showed an overall
response rate of 83.1% (95% CI: 73.3-90.5) and a CR rate of 72.3%
(95% CI: 61.4 to 81.6). Median duration of response was 15.7 months
(95% CI: 6.2 to 24.0) and progression-free survival was 15.3 months
(95% CI: 6.6 to 24.9).
Breyanzi has exhibited a consistent safety profile across
clinical trials (n=702) with any grade cytokine release syndrome
(CRS) occurring in 54% of patients, including Grade >3 CRS in 3.2% of patients. The median time to
onset was 5 days (range: 1 to 63 days). Any grade neurologic events
(NEs) were reported in 31% of patients, including Grade
>3 in 10% of patients. The median
time to onset of NEs was 8 days (range: 1 to 63 days). NEs resolved
in 88% of patients with a median duration of 7 days (range: 1 to
119 days). The safety profile of Breyanzi allows for the option of
outpatient treatment and management of patients. Breyanzi was
administered in the inpatient and outpatient setting in the MCL
cohort of TRANSCEND NHL 001.
“The approval of Breyanzi brings a new CAR T cell therapy option
to patients battling relapsed or refractory MCL,” said Meghan
Gutierrez, chief executive officer, Lymphoma Research Foundation.
“Each advance in treatment represents important progress in
improving outcomes for patients, and this news builds upon this
progress with a new potentially transformative treatment where
there are currently limited options. We are thankful for the
families and the researchers involved in making this approval a
reality for those living with this disease.”
To support this additional indication for Breyanzi, Bristol
Myers Squibb has made continuous investments to increase
manufacturing capacity and is prepared to meet demand for
Breyanzi.
Breyanzi is broadly covered by commercial and government
insurance programs in the U.S. Bristol Myers Squibb offers various
programs and resources to address the needs of patients and
caregivers, and provides support that allows for access to
therapies, including Breyanzi. Bristol Myers Squibb also supports
the patient and physician treatment experience by providing Cell
Therapy 360, a digital service platform, which optimizes access to
relevant information, manufacturing updates, and patient and
caregiver support.
*Treatment process includes leukapheresis, manufacturing,
administration and adverse event monitoring.
About TRANSCEND NHL 001
TRANSCEND NHL 001 (NCT02631044) is an open-label, multicenter,
pivotal, Phase 1, single-arm, seamless-design study to determine
the safety, pharmacokinetics and antitumor activity of Breyanzi in
patients with relapsed or refractory B-cell non-Hodgkin lymphoma,
including diffuse large B-cell lymphoma, high-grade B-cell
lymphoma, primary mediastinal B-cell lymphoma, follicular lymphoma
Grade 3B and mantle cell lymphoma. The primary outcome measures are
treatment-related adverse events, dose-limiting toxicities and
overall response rate. Secondary outcome measures include complete
response rate, duration of response, and progression-free
survival.
About MCL
Mantle cell lymphoma (MCL) is an aggressive, rare form of
non-Hodgkin lymphoma (NHL), representing roughly 3% of all NHL
cases. MCL originates from cells in the “mantle zone” of the lymph
node. MCL occurs more frequently in older adults with an average
age at diagnosis in the mid-60s, and it is more often found in
males than in females. In MCL, relapse after initial treatment is
common, and for most, the disease eventually progresses or
returns.
About Breyanzi
Breyanzi is a CD19-directed CAR T cell therapy with a 4-1BB
costimulatory domain, which enhances the expansion and persistence
of the CAR T cells. Breyanzi is made from a patient’s own T cells,
which are collected and genetically reengineered to become CAR T
cells that are then delivered via infusion as a one-time
treatment.
Breyanzi is approved in the U.S. for the treatment of relapsed
or refractory large B-cell lymphoma (LBCL) after at least one prior
line of therapy, and has received accelerated approval for the
treatment of relapsed or refractory chronic lymphocytic leukemia or
small lymphocytic lymphoma after at least two prior lines of
therapy, and relapsed or refractory follicular lymphoma in the
third-line plus setting. Breyanzi is also approved in Japan, the
European Union (EU), and Switzerland for the second-line treatment
of relapsed or refractory LBCL, and in Japan, the EU, Switzerland,
the UK and Canada for relapsed and refractory LBCL after two or
more lines of systemic therapy.
Bristol Myers Squibb’s clinical development program for Breyanzi
includes clinical studies in other types of lymphoma. For more
information, visit clinicaltrials.gov.
Indications
BREYANZI is a CD19-directed genetically modified autologous T
cell immunotherapy indicated for the treatment of:
- adult patients with large B-cell lymphoma (LBCL), including
diffuse large B-cell lymphoma (DLBCL) not otherwise specified
(including DLBCL arising from indolent lymphoma), high-grade B cell
lymphoma, primary mediastinal large B-cell lymphoma, and follicular
lymphoma grade 3B, who have:
- refractory disease to first-line chemoimmunotherapy or relapse
within 12 months of first-line chemoimmunotherapy; or
- refractory disease to first-line chemoimmunotherapy or relapse
after first-line chemoimmunotherapy and are not eligible for
hematopoietic stem cell transplantation (HSCT) due to comorbidities
or age; or
- relapsed or refractory disease after two or more lines of
systemic therapy.
Limitations of Use: BREYANZI is not
indicated for the treatment of patients with primary central
nervous system lymphoma.
- adult patients with relapsed or refractory chronic lymphocytic
leukemia (CLL) or small lymphocytic lymphoma (SLL) who have
received at least 2 prior lines of therapy, including a Bruton
tyrosine kinase (BTK) inhibitor and a B-cell lymphoma 2 (BCL-2)
inhibitor. This indication is approved under accelerated approval
based on response rate and duration of response. Continued approval
for this indication may be contingent upon verification and
description of clinical benefit in confirmatory trial(s).
- adult patients with relapsed or refractory follicular lymphoma
(FL) who have received 2 or more prior lines of systemic therapy.
This indication is approved under accelerated approval based on
response rate and duration of response. Continued approval for this
indication may be contingent upon verification and description of
clinical benefit in confirmatory trial(s).
- adult patients with relapsed or refractory mantle cell lymphoma
(MCL) who have received at least 2 prior lines of systemic therapy,
including a Bruton tyrosine kinase (BTK) inhibitor.
Important Safety
Information
WARNING: CYTOKINE RELEASE SYNDROME, NEUROLOGIC TOXICITIES,
AND SECONDARY HEMATOLOGICAL MALIGNANCIES
- Cytokine Release Syndrome (CRS), including fatal or
life-threatening reactions, occurred in patients receiving
BREYANZI. Do not administer BREYANZI to patients with active
infection or inflammatory disorders. Treat severe or
life-threatening CRS with tocilizumab with or without
corticosteroids.
- Neurologic toxicities, including fatal or life-threatening
reactions, occurred in patients receiving BREYANZI, including
concurrently with CRS, after CRS resolution, or in the absence of
CRS. Monitor for neurologic events after treatment with BREYANZI.
Provide supportive care and/or corticosteroids as needed.
- T cell malignancies have occurred following treatment of
hematologic malignancies with BCMA- and CD19-directed genetically
modified autologous T cell immunotherapies, including
BREYANZI.
- BREYANZI is available only through a restricted program
under a Risk Evaluation and Mitigation Strategy (REMS) called the
BREYANZI REMS.
Cytokine Release Syndrome
Cytokine release syndrome (CRS), including fatal or
life-threatening reactions, occurred following treatment with
BREYANZI. In clinical trials of BREYANZI, which enrolled a total of
702 patients with non-Hodgkin lymphoma (NHL), CRS occurred in 54%
of patients, including ≥ Grade 3 CRS in 3.2% of patients. The
median time to onset was 5 days (range: 1 to 63 days). CRS resolved
in 98% of patients with a median duration of 5 days (range: 1 to 37
days). One patient had fatal CRS and 5 patients had ongoing CRS at
the time of death. The most common manifestations of CRS (≥10%)
were fever, hypotension, tachycardia, chills, hypoxia, and
headache.
Serious events that may be associated with CRS include cardiac
arrhythmias (including atrial fibrillation and ventricular
tachycardia), cardiac arrest, cardiac failure, diffuse alveolar
damage, renal insufficiency, capillary leak syndrome, hypotension,
hypoxia, and hemophagocytic lymphohistiocytosis/macrophage
activation syndrome (HLH/MAS).
Ensure that 2 doses of tocilizumab are available prior to
infusion of BREYANZI.
Neurologic Toxicities
Neurologic toxicities that were fatal or life-threatening,
including immune effector cell-associated neurotoxicity syndrome
(ICANS), occurred following treatment with BREYANZI. Serious events
including cerebral edema and seizures occurred with BREYANZI. Fatal
and serious cases of leukoencephalopathy, some attributable to
fludarabine, also occurred.
In clinical trials of BREYANZI, CAR T cell-associated neurologic
toxicities occurred in 31% of patients, including ≥ Grade 3 cases
in 10% of patients. The median time to onset of neurotoxicity was 8
days (range: 1 to 63 days). Neurologic toxicities resolved in 88%
of patients with a median duration of 7 days (range: 1 to 119
days). Of patients developing neurotoxicity, 82% also developed
CRS.
The most common neurologic toxicities (≥5%) included
encephalopathy, tremor, aphasia, headache, dizziness, and
delirium.
CRS and Neurologic Toxicities Monitoring
Monitor patients daily for at least 7 days following BREYANZI
infusion at a REMS-certified healthcare facility for signs and
symptoms of CRS and neurologic toxicities and assess for other
causes of neurological symptoms. Monitor patients for signs and
symptoms of CRS and neurologic toxicities for at least 4 weeks
after infusion and treat promptly. At the first sign of CRS,
institute treatment with supportive care, tocilizumab, or
tocilizumab and corticosteroids as indicated. Manage neurologic
toxicity with supportive care and/or corticosteroid as needed.
Counsel patients to seek immediate medical attention should signs
or symptoms of CRS or neurologic toxicity occur at any time.
BREYANZI REMS
Because of the risk of CRS and neurologic toxicities, BREYANZI
is available only through a restricted program under a Risk
Evaluation and Mitigation Strategy (REMS) called the BREYANZI REMS.
The required components of the BREYANZI REMS are:
- Healthcare facilities that dispense and administer BREYANZI
must be enrolled and comply with the REMS requirements.
- Certified healthcare facilities must have on-site, immediate
access to tocilizumab.
- Ensure that a minimum of 2 doses of tocilizumab are available
for each patient for infusion within 2 hours after BREYANZI
infusion, if needed for treatment of CRS.
Further information is available at www.BreyanziREMS.com, or
contact Bristol-Myers Squibb at 1-866-340-7332.
Hypersensitivity Reactions
Allergic reactions may occur with the infusion of BREYANZI.
Serious hypersensitivity reactions, including anaphylaxis, may be
due to dimethyl sulfoxide (DMSO).
Serious Infections
Severe infections, including life-threatening or fatal
infections, have occurred in patients after BREYANZI infusion. In
clinical trials of BREYANZI, infections of any grade occurred in
34% of patients, with Grade 3 or higher infections occurring in 12%
of all patients. Grade 3 or higher infections with an unspecified
pathogen occurred in 7%, bacterial infections in 3.7%, viral
infections in 2%, and fungal infections in 0.7% of patients. One
patient who received 4 prior lines of therapy developed a fatal
case of John Cunningham (JC) virus progressive multifocal
leukoencephalopathy 4 months after treatment with BREYANZI. One
patient who received 3 prior lines of therapy developed a fatal
case of cryptococcal meningoencephalitis 35 days after treatment
with BREYANZI.
Febrile neutropenia developed after BREYANZI infusion in 8% of
patients. Febrile neutropenia may be concurrent with CRS. In the
event of febrile neutropenia, evaluate for infection and manage
with broad-spectrum antibiotics, fluids, and other supportive care
as medically indicated.
Monitor patients for signs and symptoms of infection before and
after BREYANZI administration and treat appropriately. Administer
prophylactic antimicrobials according to standard institutional
guidelines. Avoid administration of BREYANZI in patients with
clinically significant, active systemic infections.
Viral reactivation: Hepatitis B virus (HBV) reactivation, in
some cases resulting in fulminant hepatitis, hepatic failure, and
death, can occur in patients treated with drugs directed against B
cells. In clinical trials of BREYANZI, 35 of 38 patients with a
prior history of HBV were treated with concurrent antiviral
suppressive therapy. Perform screening for HBV, HCV, and HIV in
accordance with clinical guidelines before collection of cells for
manufacturing. In patients with prior history of HBV, consider
concurrent antiviral suppressive therapy to prevent HBV
reactivation per standard guidelines.
Prolonged Cytopenias
Patients may exhibit cytopenias not resolved for several weeks
following lymphodepleting chemotherapy and BREYANZI infusion. In
clinical trials of BREYANZI, Grade 3 or higher cytopenias persisted
at Day 29 following BREYANZI infusion in 35% of patients, and
included thrombocytopenia in 25%, neutropenia in 22%, and anemia in
6% of patients. Monitor complete blood counts prior to and after
BREYANZI administration.
Hypogammaglobulinemia
B-cell aplasia and hypogammaglobulinemia can occur in patients
receiving BREYANZI. In clinical trials of BREYANZI,
hypogammaglobulinemia was reported as an adverse reaction in 10% of
patients. Hypogammaglobulinemia, either as an adverse reaction or
laboratory IgG level below 500 mg/dL after infusion, was reported
in 30% of patients. Monitor immunoglobulin levels after treatment
with BREYANZI and manage using infection precautions, antibiotic
prophylaxis, and immunoglobulin replacement as clinically
indicated.
Live vaccines: The safety of immunization with live viral
vaccines during or following BREYANZI treatment has not been
studied. Vaccination with live virus vaccines is not recommended
for at least 6 weeks prior to the start of lymphodepleting
chemotherapy, during BREYANZI treatment, and until immune recovery
following treatment with BREYANZI.
Secondary Malignancies
Patients treated with BREYANZI may develop secondary
malignancies. T cell malignancies have occurred following treatment
of hematologic malignancies with BCMA- and CD19-directed
genetically modified autologous T cell immunotherapies, including
BREYANZI. Mature T cell malignancies, including CAR-positive
tumors, may present as soon as weeks following infusion, and may
include fatal outcomes. Monitor lifelong for secondary
malignancies. In the event that a secondary malignancy occurs,
contact Bristol-Myers Squibb at 1-888-805-4555 for reporting and to
obtain instructions on collection of patient samples for
testing.
Effects on Ability to Drive and Use Machines
Due to the potential for neurologic events, including altered
mental status or seizures, patients receiving BREYANZI are at risk
for developing altered or decreased consciousness or impaired
coordination in the 8 weeks following BREYANZI administration.
Advise patients to refrain from driving and engaging in hazardous
occupations or activities, such as operating heavy or potentially
dangerous machinery, for at least 8 weeks.
Immune Effector Cell-Associated Hemophagocytic
Lymphohistiocytosis-Like Syndrome (IEC-HS)
Immune Effector Cell-Associated Hemophagocytic
Lymphohistiocytosis-Like Syndrome (IEC-HS), including fatal or
life-threatening reactions, occurred following treatment with
BREYANZI. Three of 89 (3%) safety evaluable patients with R/R
CLL/SLL developed IEC-HS. Time to onset of IEC-HS ranged from 7 to
18 days. Two of the 3 patients developed IEC-HS in the setting of
ongoing CRS and 1 in the setting of ongoing neurotoxicity. IEC-HS
was fatal in 2 of 3 patients. One patient had fatal IEC-HS and one
had ongoing IEC-HS at time of death. IEC-HS is a life-threatening
condition with a high mortality rate if not recognized and treated
early. Treatment of IEC-HS should be administered per current
practice guidelines.
Adverse Reactions
The most common adverse reaction(s) (incidence ≥30%) in:
- LBCL are fever, cytokine release syndrome, fatigue,
musculoskeletal pain, and nausea. The most common Grade 3-4
laboratory abnormalities include lymphocyte count decrease,
neutrophil count decrease, platelet count decrease, and hemoglobin
decrease.
- CLL/SLL are cytokine release syndrome, encephalopathy, fatigue,
musculoskeletal pain, nausea, edema, and diarrhea. The most common
Grade 3-4 laboratory abnormalities include neutrophil count
decrease, white blood cell decrease, hemoglobin decrease, platelet
count decrease, and lymphocyte count decrease.
- FL is cytokine release syndrome. The most common Grade 3-4
laboratory abnormalities include lymphocyte count decrease,
neutrophil count decrease, and white blood cell decrease.
- MCL are cytokine release syndrome, fatigue, musculoskeletal
pain, and encephalopathy. The most common Grade 3-4 laboratory
abnormalities include neutrophil count decrease, white blood cell
decrease, and platelet count decrease.
Please see full Prescribing Information,
including Boxed WARNINGS and Medication
Guide.
Bristol Myers Squibb: Creating a Better
Future for People with Cancer
Bristol Myers Squibb is inspired by a single vision—transforming
patients’ lives through science. The goal of the company’s cancer
research is to deliver medicines that offer each patient a better,
healthier life and to make cure a possibility. Building on a legacy
across a broad range of cancers that have changed survival
expectations for many, Bristol Myers Squibb researchers are
exploring new frontiers in personalized medicine, and through
innovative digital platforms, are turning data into insights that
sharpen their focus. Deep understanding of causal human biology,
cutting-edge capabilities and differentiated research platforms
uniquely position the company to approach cancer from every
angle.
Cancer can have a relentless grasp on many parts of a patient’s
life, and Bristol Myers Squibb is committed to taking actions to
address all aspects of care, from diagnosis to survivorship. As a
leader in cancer care, Bristol Myers Squibb is working to empower
all people with cancer to have a better future.
Learn more about the science behind cell therapy and ongoing
research at Bristol Myers Squibb here.
About Bristol Myers
Squibb
Bristol Myers Squibb is a global biopharmaceutical company whose
mission is to discover, develop and deliver innovative medicines
that help patients prevail over serious diseases. For more
information about Bristol Myers Squibb, visit us at BMS.com or
follow us on LinkedIn, Twitter, YouTube, Facebook and
Instagram.
Cautionary Statement Regarding
Forward-Looking Statements
This press release contains “forward-looking statements” within
the meaning of the Private Securities Litigation Reform Act of 1995
regarding, among other things, the research, development and
commercialization of pharmaceutical products. All statements that
are not statements of historical facts are, or may be deemed to be,
forward-looking statements. Such forward-looking statements are
based on current expectations and projections about our future
financial results, goals, plans and objectives and involve inherent
risks, assumptions and uncertainties, including internal or
external factors that could delay, divert or change any of them in
the next several years, that are difficult to predict, may be
beyond our control and could cause our future financial results,
goals, plans and objectives to differ materially from those
expressed in, or implied by, the statements. These risks,
assumptions, uncertainties and other factors include, among others,
whether Breyanzi (lisocabtagene maraleucel) for the additional
indication described in this release will be commercially
successful, any marketing approvals, if granted, may have
significant limitations on their use, and that continued approval
of Breyanzi for such additional indication described in this
release may be contingent upon verification and description of
clinical benefit in confirmatory trials. No forward-looking
statement can be guaranteed. Forward-looking statements in this
press release should be evaluated together with the many risks and
uncertainties that affect Bristol Myers Squibb’s business and
market, particularly those identified in the cautionary statement
and risk factors discussion in Bristol Myers Squibb’s Annual Report
on Form 10-K for the year ended December 31, 2023, as updated by
our subsequent Quarterly Reports on Form 10-Q, Current Reports on
Form 8-K and other filings with the Securities and Exchange
Commission. The forward-looking statements included in this
document are made only as of the date of this document and except
as otherwise required by applicable law, Bristol Myers Squibb
undertakes no obligation to publicly update or revise any
forward-looking statement, whether as a result of new information,
future events, changed circumstances or otherwise.
corporatefinancial-news
View source
version on businesswire.com: https://www.businesswire.com/news/home/20240523741069/en/
Bristol Myers Squibb Media Inquiries:
media@bms.com Investors: investor.relations@bms.com
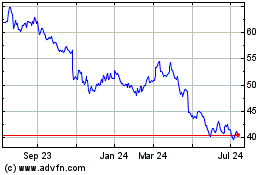
Bristol Myers Squibb (NYSE:BMY)
Historical Stock Chart
From Nov 2024 to Dec 2024
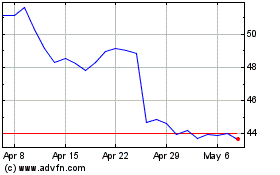
Bristol Myers Squibb (NYSE:BMY)
Historical Stock Chart
From Dec 2023 to Dec 2024