Intercept Pharmaceuticals, Inc., a biopharmaceutical company and
wholly-owned subsidiary of Alfasigma S.p.A. focused on the
development and commercialization of novel therapeutics to treat
rare and serious liver diseases, today announced new data from a
sub-analysis of the landmark Phase 3 POISE trial evaluating the
impact of obeticholic acid (OCA) on achievement of gamma-glutamyl
transferase (GGT) <3.2×upper limit of normal (ULN) and alkaline
phosphatase (ALP) <1.5×ULN for the treatment of primary biliary
cholangitis (PBC). This analysis suggests OCA’s potential to reduce
GGT, in addition to the well-known effects on ALP levels, below the
biochemical thresholds that are prognostic for worsening clinical
outcomes. These data will be presented on Monday, November 13,
2023, at the American Association for the Study of Liver Diseases’
(AASLD) The Liver Meeting® in Boston.
“These new data demonstrate the potential of OCA to reduce GGT,
in addition to the already established effect on ALP levels, which
have been shown to be predictive of risk of liver transplantation
or death in patients with PBC,” said M. Michelle Berrey, M.D.,
M.P.H., President of Research & Development and Chief Medical
Officer of Intercept. “With the increasing evidence of improved
event-free survival for patients treated with OCALIVA across
different studies, it was important to improve our understanding of
OCALIVA’s impact on different biochemical markers and how that
correlates with improved outcomes. We are pleased to join
clinicians, researchers and industry peers at The Liver Meeting®
2023 to share these data that reaffirm the need for comprehensive
assessment of treatment response beyond ALP when managing patients
with PBC.”
In the study, patients with PBC who were receiving a stable dose
of ursodeoxycholic acid (UDCA) or who were unable to tolerate UDCA
were randomized to receive placebo, OCA 5-10 mg (OCA titration), or
OCA 10 mg daily. For the OCA 5-10 mg group, OCA 5 mg was titrated
to 10 mg at 6 months based on tolerability and biochemical
response. A 12-month double-blind (DB) period was followed by a
5-year optional open-label extension (OLE), in which all patients
were initially treated with OCA 5 mg daily for the first 3 months;
every 3 months thereafter, patients had the option to increase the
dose up to 10 mg. Serum GGT and ALP levels were assessed at
baseline and every 3 months through the 5-year follow-up.
Hepatocyte injury causes GGT to be released into the blood.
Elevated GGT in the setting of elevated ALP and other liver enzyme
abnormalities is a marker for hepatobiliary disorder. The goal of
this sub-analysis was to evaluate the proportion of patients
receiving OCA who achieved and sustained GGT <3.2×ULN and ALP
<1.5×ULN. Results include:
- In the double-blind (DB) intent-to-treat population (N=203),
the proportion of responders was significantly greater at each time
point in both OCA cohorts compared with placebo, with the highest
responder rates observed in the OCA 10 mg group.
- In the OCA titration group, 17% (11/66) were responders at DB
Months 9 and 12. In the OCA 10 mg group, the highest responder rate
was observed at DB Month 9 (31% [21/68]), followed by DB Month 12
(26% [18/68]).
- In the open-label extension (OLE) intent-to-treat population
(N=119), the proportion of responders generally increased over
time, ranging from 18% (22/119) at OLE Month 3 to 38% (35/91) at
OLE Month 51. At OLE Month 60, 37% (17/46) were responders.
“A recent study from the Global PBC study group showed that GGT
≥3.2xULN and ALP≥1.5xULN increase the risk of liver transplantation
or death in patients with PBC,” said Robert G. Gish, M.D. FAASLD,
Professor at Loma Linda University Department of Medicine. “This
new analysis shows that OCA can reduce and maintain GGT and ALP
levels below these thresholds over a 6-year period, adding to an
already substantial body of evidence supporting OCA’s potential to
decrease the risk of progression to liver transplant or death in
patients with PBC.”
Poster Presentation“Effect of
Obeticholic Acid on Prognostic Thresholds of Gamma-Glutamyl
Transferase and Alkaline Phosphatase Levels: Sub-analysis of the
Phase 3 POISE Trial in Primary Biliary Cholangitis” Poster
#4545-CMonday, November 13, 1-2 PM ETAlan Bonder, Darren
Wheeler, Radhika Nair, Erik Ness, Elizabeth S. Malecha and Robert
G. Gish
A full list of sessions at The Liver Meeting® 2023 is available
at https://www.aasld.org/the-liver-meeting.
About the POISE Trial
The POISE trial studied the safety and efficacy of once-daily
treatment with Ocaliva in PBC patients with an inadequate
therapeutic response to, or who were unable to tolerate,
ursodeoxycholic acid (UDCA). There were 217 patients randomized to
one of three groups in the trial: placebo, OCA 10 mg, or OCA 5 mg
for six months titrated to 10 mg based on clinical response. Seven
subjects did not participate in the open-label extension and were
not included in the current study. Patients completing the
double-blind phase had the option to continue in an open-label
extension (OLE) phase for a maximum of five additional years,
during which all patients received treatment with OCA 5-10 mg once
daily. Of the 198 patients who completed the double-blind phase,
more than 95 percent continued in the long-term safety extension
phase of the trial for up to 5 years. Additional information
regarding the POISE trial can be found on the NIH clinical study
listing website:
http://clinicaltrials.gov/ct2/show/NCT01473524.
About Primary Biliary CholangitisPrimary
biliary cholangitis (PBC) is a rare, progressive, and chronic
autoimmune disease that affects the bile ducts in the liver and is
most prevalent (approximately 1 in 10,000) in women over the age of
40. PBC causes bile acid to build up in the liver, resulting in
inflammation and scarring (fibrosis), which, if left untreated, can
lead to cirrhosis, a liver transplant, or death.
About Ocaliva® (obeticholic
acid)OCALIVA, a farnesoid X receptor (FXR) agonist, is
indicated for the treatment of adult patients with primary biliary
cholangitis (PBC)
- with compensated cirrhosis who do
not have evidence of portal hypertension,
either in combination with ursodeoxycholic acid (UDCA) with an
inadequate response to UDCA or as monotherapy in patients unable to
tolerate UDCA.
This indication is approved under accelerated approval based on
a reduction in alkaline phosphatase (ALP). An improvement in
survival or disease-related symptoms has not been established.
Continued approval for this indication may be contingent upon
verification and description of clinical benefit in confirmatory
trials.
IMPORTANT SAFETY INFORMATION
WARNING: HEPATIC DECOMPENSATION AND FAILURE IN PRIMARY
BILIARY CHOLANGITIS PATIENTS WITH CIRRHOSIS
- Hepatic decompensation and failure, sometimes fatal or
resulting in liver transplant, have been reported with OCALIVA
treatment in primary biliary cholangitis (PBC) patients with either
compensated or decompensated cirrhosis.
- OCALIVA is contraindicated in PBC patients with
decompensated cirrhosis, a prior decompensation event, or with
compensated cirrhosis who have evidence of portal
hypertension.
- Permanently discontinue
OCALIVA in patients who develop laboratory or clinical evidence of
hepatic decompensation; have compensated cirrhosis and develop
evidence of portal hypertension, or experience clinically
significant hepatic adverse reactions while on
treatment.
Contraindications
OCALIVA is contraindicated in patients with:
- decompensated cirrhosis (e.g., Child-Pugh Class B or C) or
a prior decompensation event
- compensated cirrhosis who have evidence of portal hypertension
(e.g., ascites, gastroesophageal varices, persistent
thrombocytopenia)
- complete biliary obstruction
Warnings and Precautions
Hepatic Decompensation and Failure in PBC Patients with
CirrhosisHepatic decompensation and failure, sometimes
fatal or resulting in liver transplant, have been reported with
OCALIVA treatment in PBC patients with cirrhosis, either
compensated or decompensated. Among post-marketing cases reporting
it, median time to hepatic decompensation (e.g., new onset ascites)
was 4 months for patients with compensated cirrhosis; median time
to a new decompensation event (e.g., hepatic encephalopathy) was
2.5 months for patients with decompensated cirrhosis.
Some of these cases occurred in patients with decompensated
cirrhosis when they were treated with higher than the recommended
dosage for that patient population; however, cases of hepatic
decompensation and failure have continued to be reported in
patients with decompensated cirrhosis even when they received the
recommended dosage.
Hepatotoxicity was observed in the OCALIVA clinical trials. A
dose-response relationship was observed for the occurrence of
hepatic adverse reactions including jaundice, worsening ascites,
and primary biliary cholangitis flare with dosages of OCALIVA of 10
mg once daily to 50 mg once daily (up to 5-times the highest
recommended dosage), as early as one month after starting treatment
with OCALIVA in two 3-month, placebo-controlled clinical trials in
patients with primarily early stage PBC.
Routinely monitor patients for progression of PBC, including
hepatic adverse reactions, with laboratory and clinical assessments
to determine whether drug discontinuation is needed. Closely
monitor patients with compensated cirrhosis, concomitant hepatic
disease (e.g., autoimmune hepatitis, alcoholic liver disease),
and/or with severe intercurrent illness for new evidence of portal
hypertension (e.g., ascites, gastroesophageal varices, persistent
thrombocytopenia), or increases above the upper limit of normal in
total bilirubin, direct bilirubin, or prothrombin time to determine
whether drug discontinuation is needed. Permanently discontinue
OCALIVA in patients who develop laboratory or clinical evidence of
hepatic decompensation (e.g., ascites, jaundice, variceal bleeding,
hepatic encephalopathy), have compensated cirrhosis and develop
evidence of portal hypertension (e.g., ascites, gastroesophageal
varices, persistent thrombocytopenia), experience clinically
significant hepatic adverse reactions, or develop complete biliary
obstruction. If severe intercurrent illness occurs, interrupt
treatment with OCALIVA and monitor the patient’s liver function.
After resolution of the intercurrent illness, consider the
potential risks and benefits of restarting OCALIVA treatment.
Severe PruritusSevere pruritus was
reported in 23% of patients in the OCALIVA 10 mg arm, 19% of
patients in the OCALIVA titration arm, and 7% of patients in the
placebo arm in a 12-month double-blind randomized controlled
clinical trial of 216 patients. Severe pruritus was defined as
intense or widespread itching, interfering with activities of daily
living, or causing severe sleep disturbance, or intolerable
discomfort, and typically requiring medical interventions. Consider
clinical evaluation of patients with new onset or worsening severe
pruritus. Management strategies include the addition of bile acid
binding resins or antihistamines, OCALIVA dosage reduction, and/or
temporary interruption of OCALIVA dosing.
Reduction in HDL-CPatients with PBC generally
exhibit hyperlipidemia characterized by a significant elevation in
total cholesterol primarily due to increased levels of high-density
lipoprotein-cholesterol (HDL-C). Dose-dependent reductions from
baseline in mean HDL-C levels were observed at 2 weeks in
OCALIVA-treated patients, 20% and 9% in the 10 mg and titration
arms, respectively, compared to 2% in the placebo arm. Monitor
patients for changes in serum lipid levels during treatment. For
patients who do not respond to OCALIVA after 1 year at the highest
recommended dosage that can be tolerated (maximum of 10 mg once
daily), and who experience a reduction in HDL-C, weigh the
potential risks against the benefits of continuing treatment.
Adverse ReactionsThe most common adverse
reactions (≥5%) are: pruritus, fatigue, abdominal pain and
discomfort, rash, oropharyngeal pain, dizziness, constipation,
arthralgia, thyroid function abnormality, and eczema.
Drug Interactions
- Bile Acid Binding ResinsBile acid binding resins such as
cholestyramine, colestipol, or colesevelam adsorb and reduce bile
acid absorption and may reduce the absorption, systemic exposure,
and efficacy of OCALIVA. If taking a bile acid binding resin, take
OCALIVA at least 4 hours before or 4 hours after taking the bile
acid binding resin, or at as great an interval as possible.
- WarfarinThe International Normalized Ratio (INR) decreased
following coadministration of warfarin and OCALIVA. Monitor INR and
adjust the dose of warfarin, as needed, to maintain the target INR
range when co-administering OCALIVA and warfarin.
- CYP1A2 Substrates with Narrow Therapeutic IndexObeticholic acid
may increase the exposure to concomitant drugs that are CYP1A2
substrates. Therapeutic monitoring of CYP1A2 substrates with a
narrow therapeutic index (e.g., theophylline and tizanidine) is
recommended when co-administered with OCALIVA.
- Inhibitors of Bile Salt Efflux
PumpAvoid concomitant use of inhibitors of the bile salt efflux
pump (BSEP) such as cyclosporine. Concomitant medications that
inhibit canalicular membrane bile acid transporters such as the
BSEP may exacerbate accumulation of conjugated bile salts including
taurine conjugate of obeticholic acid in the liver and result in
clinical symptoms. If concomitant use is deemed necessary, monitor
serum transaminases and bilirubin.
Please click here for Full
Prescribing Information, including Boxed
WARNING.To report SUSPECTED ADVERSE REACTIONS,
contact Intercept Pharmaceuticals, Inc. at 1-844-782-ICPT
or FDA at 1-800-FDA-1088
or www.fda.gov/medwatch.
About InterceptIntercept is a biopharmaceutical
company and wholly-owned subsidiary of Alfasigma S.p.A. focused on
the development and commercialization of novel therapeutics to
treat rare and serious liver diseases, including primary biliary
cholangitis (PBC) and severe alcohol-associated hepatitis (sAH).
For more information, please
visit www.interceptpharma.com or connect with the Company
on LinkedIn, Threads, and X (formerly Twitter)
ContactFor more information about Intercept,
please contact:
For media:media@interceptpharma.com
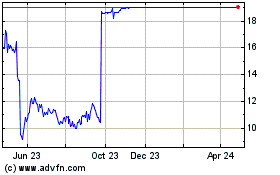
Intercept Pharmaceuticals (NASDAQ:ICPT)
Historical Stock Chart
From Mar 2024 to Apr 2024
Intercept Pharmaceuticals (NASDAQ:ICPT)
Historical Stock Chart
From Apr 2023 to Apr 2024