Summit Therapeutics Inc. (NASDAQ: SMMT) (“Summit,” “we,” or the
“Company”) and its product candidate, ridinilazole, today had an
oral podium presentation at IDWeek 2022. IDWeek is the joint annual
meeting of the Infectious Diseases Society of America (IDSA), the
Society for Healthcare Epidemiology of America (SHEA), the HIV
Medicine Association (HIVMA), the Pediatric Infectious Diseases
Society (PIDS), and the Society of Infectious Diseases Pharmacists
(SIDP).
The oral presentation, entitled “Ri-CoDIFy - A
Phase 3, Randomized, Double-Blind Study to Evaluate the Efficacy
and Safety of Ridinilazole Compared with Vancomycin for the
Treatment of Clostridioides difficile Infection,” delivered by Dr.
Pablo C. Okhuysen, M.D., Professor, Department of Infectious
Diseases at MD Anderson Cancer Center, detailed the scientific data
from the Ri-CoDIFy trial for our investigational, first-in-class
antibiotic, ridinilazole, for the treatment of Clostridioides
difficile infection (“C. diff. infection,” or “CDI”). There were
759 patients enrolled, with the mITT population comprising 745
patients; 323 were over the age of 65, 400 were hospitalized at the
beginning of treatment, and 112 were previously diagnosed with
COVID-19.
- Ridinilazole achieved a numerically higher sustained clinical
response rate (73.0% vs 70.7%) than vancomycin, but did not achieve
the pre-specified superiority endpoint
- Ridinilazole resulted in a 53% relative risk reduction in
recurrence rates of C. diff. infection vs. vancomycin
- Recurrence of C. diff. infection is a major concern for
patients with the disease; recurrence rates for infection in the
United States are estimated to be approximately 20%-25% in patients
after the initial treatment and with increased probabilities of
recurrence after each subsequent episode i, ii
- Ridinilazole resulted in an 8.1% recurrence rate of CDI vs.
17.3% for patients treated with vancomycin
- Ridinilazole consistently resulted in decreased rates of
recurrence compared to vancomycin in each of the prespecified
subgroup analyses performed
- Patients with 10+ daily unformed bowel movements prior to
treatment receiving ridinilazole experienced a disease recurrence
rate of 5.8% as compared to 28.0% for vancomycin
- Patients, aged 65 or over experienced a 9.3% recurrence rate
when treated with ridinilazole vs. 22.2% with vancomycin
- Patients with a prior COVID-19 diagnosis experienced recurrence
5.5% of the time when treated with ridinilazole vs. 24.6% when
administered vancomycin
- Immunocompromised patients recurred 13.6% with ridinilazole vs.
26.3% with vancomycin
- Ri-CoDIFy is the largest and most comprehensive CDI assessment
of the gut microbiome comprising over 600 CDI patients globally
across different regions to date
- Patients treated with ridinilazole experienced a minimal impact
on gut microbiome diversity compared to those patients treated with
vancomycin
- Ridinilazole preserved the levels of protective secondary bile
acids at the end of the treatment period, an important component of
the microbiome, while vancomycin resulted in a substantial decrease
in secondary bile acids
- Higher levels of secondary bile acids at the end of the
treatment window are associated with earlier recovery of gut
microbiome health and associated with a lower rate of recurrence of
CDI
- Ridinilazole did not increase the gut resistome as evidenced by
the relative lack of abundance of antibacterial resistance genes;
exposure to vancomycin resulted in an expansion of the gut
resistome
- Increases in the gut resistome are associated with an increased
risk of resistance to antibiotics that a patient may be using or
may use in the future
- Ridinilazole was well tolerated with a low rate of treatment
discontinuation for adverse events in the Phase 3 study
“While both ridinilazole and vancomycin target
Clostridioides difficile, the lower recurrence rates in those CDI
patients treated with ridinilazole compared to that of vancomycin
highlight the differing effects of the two drugs on the gut
microbiome,” stated Dr. Pablo C. Okhuysen, the presenter of this
data at IDWeek 2022. “Ridinilazole spared the gut microbiome and
did not select for an increase in antimicrobial resistance at the
end of treatment. Conversely, vancomycin decreased the microbiota
diversity and selected for an increase of antimicrobial resistance
to commonly-used antibiotics. The clinical and molecular results
presented continue to validate the need to develop new antibiotics,
that like ridinilazole, can selectively treat CDI (or for that
matter, any infectious agent) while at the same time preserve
microbiome diversity and not promote the emergence of antibiotic
resistance. These features are consistent with the hallmark
principles of antimicrobial stewardship and should be the focus of
future anti-infective drug development.”
“We believe that this study may be indicative as
to the need to change the way in which anti-infective agents are
developed and assessed going forward, including the need for
monitoring the impact of treatments on the gut microbiome,” added
Robert W. Duggan, Chairman and Chief Executive Officer of Summit.
“A diverse microbiome is critical to human health and protecting it
must be a focus going forward. As we saw in the Ri-CoDIFy study,
the health of the microbiome was associated with a lower rate of
recurrence of CDI. I am very proud of the work of Team Summit in
this significant breakthrough to the infectious disease space and
beyond. As we have referenced several times and further illustrated
by Drs. Giovanni, Schneider, Calder, and Fauci in the Journal of
Infectious Diseases,iii the microbiome not only impacts infectious
diseases, but can impact immune-mediated diseases and potentially
beyond: maintaining a healthy, diverse microbiome is critical to
maximizing patient safety and optimizing overall human health.”
A poster, entitled “A US-Based National
Surveillance Study for the Susceptibility and Epidemiology of
Clostridioides difficile Associated Diarrheal Isolates with Special
Reference to Ridinilazole: 2020-2021” is also available throughout
IDWeek 2022.
Ridinilazole is not currently approved for use
by any regulatory authority.
The presentation and poster are now available
within the “Scientific Literature & Publications” section of
our website: https://www.summittxinc.com/publications/.
Summit Therapeutics’ Mission Statement
To build a viable, long-lasting health care
organization that assumes full responsibility for designing,
developing, trial execution and enrollment, regulatory submission
and approval, and successful commercialization of patient,
physician, caregiver, and societal-friendly medicinal therapy
intended to: improve quality of life, increase potential duration
of life, and resolve serious medical healthcare needs. To identify
and control promising product candidates based on exceptional
scientific development and administrational expertise, develop our
products in a rapid, cost-efficient manner, and to engage
commercialization and/or development partners when appropriate.
We accomplish this by building a team of world
class professional scientists and business administrators that
apply their experience and knowledge to this mission. Team Summit
exists to pose, strategize, and execute a path forward in medicinal
therapeutic health care that places Summit in a well-deserved, top
market share, leadership position. Team Summit assumes full
responsibility for stimulating continuous expansion of knowledge,
ability, capability, and well-being for all involved stakeholders
and highly-valued shareholders.
About Summit TherapeuticsSummit
was founded in 2003 and our shares are listed on the Nasdaq Global
Market (symbol ‘SMMT’). We are headquartered in Menlo Park,
California, and we have additional offices in Oxford, UK and
Cambridge, UK.For more information, please visit
https://www.summittxinc.com and follow us on Twitter
@summitplc.
Contact Summit Investor
Relations:Dave GancarzHead of Stakeholder Relations &
Corporate Strategydavid.gancarz@summitplc.com
General Inquiries:
investors@summitplc.com
Summit Forward-looking
StatementsAny statements in this press release about the
Company’s future expectations, plans and prospects, including but
not limited to, statements about the clinical and preclinical
development of the Company’s product candidates, the therapeutic
potential of the Company’s product candidates, the potential
commercialization of the Company’s product candidates, the timing
of initiation, completion and availability of data from clinical
trials, the potential submission of applications for marketing
approvals, the impact of the COVID-19 pandemic on the Company’s
operations and clinical trials, potential acquisitions and other
statements containing the words "anticipate," "believe,"
"continue," "could," "estimate," "expect," "intend," "may," "plan,"
"potential," "predict," "project," "should," "target," "would," and
similar expressions, constitute forward-looking statements within
the meaning of The Private Securities Litigation Reform Act of
1995. Actual results may differ materially from those indicated by
such forward-looking statements as a result of various important
factors, including the results of our evaluation of the underlying
data in connection with the topline results of our Phase III
Ri-CoDIFy study evaluating ridinilazole, the outcome of discussions
with regulatory authorities, including the Food and Drug
Administration, the uncertainties inherent in the initiation of
future clinical trials, availability and timing of data from
ongoing and future clinical trials, the results of such trials, and
their success, and global public health crises, including the
coronavirus COVID-19 outbreak, that may affect timing and status of
our clinical trials and operations, whether preliminary results
from a clinical trial will be predictive of the final results of
that trial or whether results of early clinical trials or
preclinical studies will be indicative of the results of later
clinical trials, whether business development opportunities to
expand the Company’s pipeline of drug candidates, including without
limitation, through potential acquisitions of, and/or
collaborations with, other entities occur, expectations for
regulatory approvals, laws and regulations affecting government
contracts and funding awards, availability of funding sufficient
for the Company’s foreseeable and unforeseeable operating expenses
and capital expenditure requirements and other factors discussed in
the "Risk Factors" section of filings that the Company makes with
the Securities and Exchange Commission. Any change to our ongoing
trials could cause delays, affect our future expenses, and add
uncertainty to our commercialization efforts, as well as to affect
the likelihood of the successful completion of clinical development
of ridinilazole. Accordingly, readers should not place undue
reliance on forward-looking statements or information. In addition,
any forward-looking statements included in this press release
represent the Company’s views only as of the date of this release
and should not be relied upon as representing the Company’s views
as of any subsequent date. The Company specifically disclaims any
obligation to update any forward-looking statements included in
this press release.
Appendix: Glossary of Critical Terms Contained
Herein
Antibiotic resistance genes –
Genes known to be involved in bacterial resistance; such genes may
include, for example, beta-lactamases which can inactivate various
beta-lactam antibiotics.
Bile acids – a collection of
steroid-based gut metabolites, the balance of the amount of and
types of bile acids in the gut microbiome are believed to play an
important role in the development of or prevention of an initial
and potential recurrent instance of C. difficile Infection.ii
Clostridia – a class of
bacteria that exist within a healthy gut microbiome that likely
plays a largely crucial role in microbiome homeostasis by
interacting with the other resident microbe populations and
providing specific and essential functions to the overall
microbiome. While most groups of Clostridia have a commensal, or
co-existing, relationship with the rest of the gut microbiome, some
Clostridia can be pathogenic, when larger concentrations of the
bacteria exist, such as Clostridioides difficile
bacteria.iv
Clostridioides difficile
(C. difficile or C. diff.) – a germ (bacterium)
that can cause severe diarrhea and colitis (an inflammation of the
colon). C. difficile can live naturally in the intestines
(gut) of humans and not cause any problem. Sometimes changes in the
gut microbiome lead the bacteria to grow and produce toxins from
which illness can develop.v
C. diff. Infection
(CDI) – a bacterial infection of the colon that produces
toxins causing inflammation of the colon and severe watery
diarrhea, very painful and persistent abdominal cramping, nausea,
fever, and dehydration. CDI can also result in more serious disease
complications, including bowel perforation (a tear in the
gastrointestinal tract), sepsis, and death. Most cases of C.
diff. infection occur while a person is taking antibiotics or not
long after a person has finished taking antibiotics. CDI is
an insidious and debilitating disease that necessitates patient
isolation because of its contagious nature, making it able to be
passed from one person to another either in a hospital or long-term
care facility setting or in the community.v
Gut microbiome – within the
human gastrointestinal tract, the gut microbiome is a collection of
microbiota, consisting of trillions of microorganisms that inhabit
the gut. The gut microbiota is considered an important
partner to human cell systems, interacting extensively with other
organs in the body to influence a wide range of functions from
digestion to immunity. The balance of the different types of
cells and microorganisms within the microbiome is considered to be
important in the microbiome's ability to properly play its role
within the human body. Disruption in the balance of
microorganisms within the gut microbiome (known as dysbiosis) is
believed to impact the gut microbiome's role in keeping a person
healthy and free of certain conditions or diseases.ii, vi
Gut microbiota – the trillions
of microorganisms, including symbiotic and pathogenic
microorganisms, that inhabit the gut. Examples of these
microorganisms include bacteria, fungi, viruses, protists, and
archaea.
Gut resistome – within the
human gastrointestinal tract, the diversity and dynamics of the
antibiotic resistance genes that are harbored by the gut
microbiota. Examples of the gut resistome include genes
associated with resistance to carbapenem antibiotics.vii
Microbiome - a community
of microorganisms (such as bacteria, fungi, and viruses)
that live in or on humans; the collection of microbial genomes that
contribute to the broader genetic portrait, or metagenome, of a
human.viii
Vancomycin – an antibiotic that
is used to treat CDI
_____________________________
i Song JH, Kim YS. Recurrent Clostridium
difficile Infection: Risk Factors, Treatment, and Prevention.
Gut Liver Vol 13(1):16-24, 2019.
ii Qian, X, et. al. Ridinilazole, a narrow spectrum antibiotic
for treatment of Clostridioides difficile infection, enhances
preservation of microbiota-dependent bile acids. Am J Physiol
Gasterintest Liver Physiol 319: G227-G237, 2020.
iii Giovanni, Schneider, Calder, and Fauci. Refocusing Human
Microbiota Research in Infectious and Immune-Mediated Diseases:
Advancing to the Next Stage. The Journal of Infectious Diseases,
Vol. 224, Issue 1: 5-8, Jul 2021.
iv Lopetuso, L.R., et al. Commensal Clostridia: leading players
in the maintenance of gut homeostasis. Gut Pathog 5, 23, 2013.
v United States Centers for Disease Control and
Prevention. https://www.cdc.gov/cdiff/what-is.html.
Accessed October 2022.
vi Cani PD. Human gut microbiome: hopes, threats and
promises. British Medical Journal (BMJ) Gut
67:1716-1725, 2018.
vii van Schaik, W. The human gut resistome. Philos Trans R Soc
Lond B Biol Sci. 370(1670):20140087, 2015.
viii Britannica Medical Dictionary.
https://www.britannica.com/s
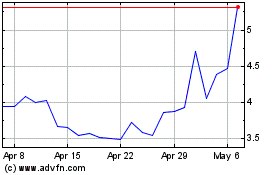
Summit Therapeutics (NASDAQ:SMMT)
Historical Stock Chart
From Apr 2024 to May 2024
Summit Therapeutics (NASDAQ:SMMT)
Historical Stock Chart
From May 2023 to May 2024
