Molina Healthcare, Inc. (NYSE: MOH):
- Net loss of $230 million for the
quarter, or $4.10 per diluted share.
- Restructuring plan now underway is
expected to reduce annualized run-rate expenses by $300 million to
$400 million upon completion in 2018.
- $200 million total reduction to
annualized run-rate expenses resulting from staff reductions
expected to be achieved by the end of 2017 in time for full
realization in 2018.
- Annualized salary eliminations of $55
million achieved so far in the third quarter of 2017.
- Direct delivery operations will be
restructured during the second half of 2017.
- 2018 Marketplace participation to be
terminated in Utah and Wisconsin; additional states in review.
- 2017 earnings per share guidance
withdrawn.
Molina Healthcare, Inc. (NYSE: MOH) today reported its financial
results for the second quarter of 2017.
“We are disappointed with our bottom-line results for this
quarter and have taken aggressive and urgent steps to substantially
improve our financial performance going forward,” said Joseph
White, chief financial officer and interim president and chief
executive officer of Molina Healthcare, Inc. “Following a thorough
review of our business operations, we have begun to implement a
Company-wide restructuring plan that we expect will reduce
annualized run-rate expenses by between $300 million and $400
million by late 2018 when fully implemented, with approximately
$200 million of these run-rate reductions expected to be achieved
by the end of 2017 and in time for full realization in 2018. In the
past, we have been focused on top line growth, often at the expense
of bottom line results. While we expect to enjoy continued RFP and
organic growth in our Medicaid managed care business, we are now
intensively focused on improved operating performance and
efficiency as the path to greater profitability and shareholder
returns.”
Second Quarter 2017 Compared with Second Quarter 2016
Net loss per diluted share was $4.10 in the second quarter of
2017 compared with net income per diluted share of $0.58 reported
for the second quarter of 2016. Loss before income tax benefit for
the second quarter of 2017 was $314 million.
Certain significant items increased loss before income tax
benefit in the second quarter of 2017 by approximately $330
million. Specifically:
- We recorded $72 million in non-cash
impairment losses for goodwill and intangibles, primarily relating
to our Pathways subsidiary. In the course of developing our
restructuring and profitability improvement plan, we determined
that future benefits to be derived from Pathways (including
integration with our health plans) will be less than previously
anticipated. While such impairment losses have a short-term impact
on profitability, there is no impact to our cash flows. Pathways
experienced operating losses of $8 million for the quarter ended
June 30, 2017 and $12 million for the six months ended June 30,
2017.
- Medical care costs related to 2016
service dates were significantly in excess of what the Company
usually experiences for out-of-period claims development,
particularly at the Florida, Illinois, New Mexico, and Puerto Rico
health plans. In total, we experienced out-of-period claims
development that was approximately $85 million higher than expected
at December 31, 2016.
- We recorded $44 million for Marketplace
changes in estimates, including risk transfer and cost sharing
subsidies, related to 2016 service dates. Liabilities for risk
transfer payments and cost sharing subsidies that were estimated at
December 31, 2016 were finalized during the second quarter of
2017.
- Loss before income tax benefit
increased by $78 million as a result of an increase to the premium
deficiency reserve established for the Marketplace program. The
reserve, which was $22 million at March 31, 2017, increased to $100
million as of June 30, 2017. Based upon revenue and cost trends
observed in the second quarter of 2017, we now believe that
Marketplace performance in the second half of 2017 will fall
substantially short of previous expectations. Marketplace
performance has been most disappointing in Florida, Utah,
Washington, and Wisconsin.
- We recorded $43 million in
restructuring and separation costs in the second quarter of 2017
related primarily to contractually required termination benefits
paid to our former chief executive officer and chief financial
officer. Also included in these costs are consulting fees incurred
for the development and implementation of our corporate
restructuring initiatives.
In addition to the items noted above, ongoing poor performance
at our Florida, Illinois, New Mexico and Puerto Rico health plans
in 2017 all contributed to our disappointing financial performance
in the second quarter of 2017.
The table below summarizes the impact of these significant items
on the Company’s financial performance.
Summary of
Significant Items Affecting 2017 Financial Results
Three Months Ended Six
Months Ended June 30, 2017 June 30, 2017 (In
millions, except per diluted share amounts) Amount
Per DilutedShare
(1)
Amount
Per DilutedShare
(1)
Impairment losses $ 72 $ 1.01 $ 72 $ 1.02 Losses at behavioral
health subsidiary exclusive of impairment 8 0.09 12 0.14 Medical
care costs related to prior year service dates that were in excess
of historical expectations 85 0.95 74 0.84 Marketplace adjustments
related to risk transfer, cost sharing subsidies, and other items
for 2016 service dates 44 0.49 47 0.53 Marketplace premium
deficiency reserve for 2017 service dates 78 0.87 70 0.79
Restructuring and separation costs 43 0.68 43 0.68 Termination fee
received for Terminated Medicare acquisition — — (75
) (0.84 ) $ 330 $ 4.09 $ 243 $ 3.16
____________________
(1)
Except for certain items that are not
deductible for tax purposes, per diluted share amounts are
generally calculated at our statutory income tax rate of 37%, which
is in excess of the effective tax rate recorded in our consolidated
statements of operations.
Income Tax (Benefit) Expense
The effective tax rate benefit for 2017 was less than the
statutory tax rate benefit due to the relatively large amount of
our reported expenses that are not deductible for tax purposes.
Restructuring and Profit Improvement Plan
As a result of our poor operating performance and catalyzed by
our change in management, we accelerated the implementation of a
comprehensive restructuring and profitability improvement plan (the
Restructuring Plan). Under the Restructuring Plan, we are taking
the following actions:
- We are streamlining our organizational
structure, including the elimination of redundant layers of
management, the consolidation of regional support services, and
other reductions to our workforce, to improve efficiency as well as
the speed and quality of our decision-making.
- We are re-designing core operating
processes such as provider payment, utilization management, quality
monitoring and improvement, and information technology to achieve
more effective and cost efficient outcomes.
- We are remediating high cost provider
contracts and building around high quality, cost-effective
networks.
- We are restructuring our existing
direct delivery operations.
- We are reviewing our vendor base to
ensure that we are partnering with the lowest-cost, most-effective
vendors.
- Throughout this process, we are taking
precautions to ensure that our actions do not impede our ability to
continue to deliver quality health care, retain existing managed
care contracts, and to secure new managed care contracts.
In total, we estimate that the Restructuring Plan will reduce
annualized run-rate expenses by approximately $300 million to $400
million upon its completion in late 2018. $200 million of these
run-rate reductions, which are a result of staff reductions, will
be in place by December 2017, and therefore will fully contribute
to our 2018 results. Since the close of the second quarter, we have
already achieved $55 million of our annualized run-rate reduction
target as a result of staff reductions taken on July 27th. All
savings targets discussed in regards to the Restructuring Plan
represent annualized run-rate savings that we expect to achieve
during the year following the indicated implementation date.
One-time costs associated with the Restructuring Plan are expected
to exceed the benefits realized in 2017 due to the upfront payment
of implementation costs and the delayed benefit of full savings
until the beginning of 2018.
We estimate that total pre-tax costs associated with the
Restructuring Plan will be approximately $130 million to $150
million for the second half of 2017, with an additional $40 million
to be incurred in 2018.
As part of the Restructuring Plan, we are reducing our corporate
and health plans workforce by approximately 10%, or 1,500
full-time-equivalent employees. This workforce rightsizing, which
represents 7% of the total number of our employees, is expected to
be completed by the end of 2017. Affected employees will be offered
severance and outplacement assistance.
“This reduction in our workforce is a difficult, but necessary,
step as we concentrate our efforts on achieving operational
excellence and improved efficiency. By transforming the entire
enterprise into a leaner, more streamlined organization, we can
enhance our decision-making, improve our operating performance, and
grow our margins,” said Mr. White.
Actions Taken to Remediate 2018 Marketplace
Performance
In addition to the Restructuring Plan, we are taking these
further steps to improve profitability in 2018:
- We are exiting the Utah and Wisconsin
ACA Marketplaces effective December 31, 2017. For the three months
ended June 30, 2017, these two health plans reported a total of
$127 million in Marketplace premium revenue (16% of consolidated
Marketplace premium revenue), and a combined Marketplace medical
care ratio of 128%.
- In our remaining Marketplace plans, we
are increasing 2018 premiums by 55%. The increase takes into
account the absence of cost sharing reduction subsidies. Had we
assumed that cost sharing reduction subsidies would be funded for
2018, the premium increase would have been 30%.
- We are also reducing the scope of our
2018 participation in the Washington Marketplace.
- We continue to closely monitor the
current political and programmatic developments pertaining to our
2018 participation in other Marketplace states, and subject to
those developments, will withdraw from 2018 participation as may be
necessary.
Withdrawing 2017 Outlook
We are withdrawing our previously issued 2017 full-year earnings
per diluted share and adjusted earnings per diluted share guidance.
Among the reasons for withdrawing guidance are:
- Our results for the quarter ended June
30, 2017.
- Uncertain medical cost trends in the
Florida, Illinois, New Mexico, and Puerto Rico health plans.
- Uncertainty around the funding of
Marketplace cost sharing subsidies.
- Potential variability in the timing of
benefits achieved and costs incurred as a result of the
Restructuring Plan.
Update on Search for Permanent Chief Executive
Officer
Our search for a permanent chief executive officer is well
underway and we are encouraged by the response.
Conference Call
Management will host a conference call and webcast to discuss
Molina Healthcare’s second quarter results at 5:00 p.m. Eastern
time on Wednesday, August 2, 2017. The number to call for the
interactive teleconference is (212) 231-2909. A telephonic replay
of the conference call will be available from 7:00 p.m. Eastern
time on Wednesday, August 2, 2017, through 6:00 p.m. Eastern Time
on Thursday, August 3, 2017, by dialing (800) 633-8284 and entering
confirmation number 21855049. A live audio broadcast of Molina
Healthcare’s conference call will be available on our website,
molinahealthcare.com. A 30-day online replay will be available
approximately an hour following the conclusion of the live
broadcast.
About Molina Healthcare
Molina Healthcare, Inc., a FORTUNE 500 company, provides managed
health care services under the Medicaid and Medicare programs and
through the state insurance marketplaces. Through our health plans
operating in 12 states across the nation and in the Commonwealth of
Puerto Rico, Molina currently serves approximately 4.7 million
members. Dr. C. David Molina founded our company in 1980 to serve
low-income families in Southern California. Today, we continue his
mission of providing high quality and cost-effective health care to
those who need it most. For more information about Molina
Healthcare, please visit our website at molinahealthcare.com.
Safe Harbor Statement under the Private Securities Litigation
Reform Act of 1995: This earnings release contains
“forward-looking statements” regarding our plans, expectations, and
anticipated future events. Actual results could differ materially
due to numerous known and unknown risks and uncertainties. Those
known risks and uncertainties include, but are not limited to, the
following:
- the success of the Restructuring Plan,
including the timing of the benefits realized;
- the numerous political and market-based
uncertainties associated with the Affordable Care Act (the “ACA”)
or “Obamacare,” including any potential repeal and replacement of
the law, amendment of the law, or move to state block grants for
Medicaid;
- the market dynamics surrounding the ACA
Marketplaces, including but not limited to uncertainties associated
with risk transfer requirements, the potential for disproportionate
enrollment of higher acuity members, the withdrawal of cost sharing
subsidies and/or premium tax credits, the adequacy of agreed rates,
and potential disruption associated with market withdrawal;
- subsequent adjustments to reported
premium revenue based upon subsequent developments or new
information, including changes to estimated amounts payable or
receivable related to Marketplace risk adjustment/risk transfer,
risk corridors, and reinsurance;
- effective management of our medical
costs;
- our ability to predict with a
reasonable degree of accuracy utilization rates, including
utilization rates associated with seasonal flu patterns or other
newly emergent diseases;
- significant budget pressures on state
governments and their potential inability to maintain current
rates, to implement expected rate increases, or to maintain
existing benefit packages or membership eligibility thresholds or
criteria, including the payment of all amounts due to our Illinois
health plan following the resolution of the Illinois budget
impasse;
- the success of our efforts to retain
existing government contracts, including those in Florida,
Illinois, New Mexico, Puerto Rico, and Texas, and to obtain new
government contracts in connection with state requests for
proposals (RFPs) in both existing and new states;
- any adverse impact resulting from the
significant changes to our executive leadership team and the
rightsizing of our workforce;
- the impact of our decision to exit the
Utah and Wisconsin ACA Marketplace markets effective
December 31, 2017;
- our ability to manage our operations,
including maintaining and creating adequate internal systems and
controls relating to authorizations, approvals, provider payments,
and the overall success of our care management initiatives;
- our ability to consummate and realize
benefits from acquisitions or divestitures;
- our receipt of adequate premium rates
to support increasing pharmacy costs, including costs associated
with specialty drugs and costs resulting from formulary changes
that allow the option of higher-priced non-generic drugs;
- our ability to operate profitably in an
environment where the trend in premium rate increases lags behind
the trend in increasing medical costs;
- the interpretation and implementation
of federal or state medical cost expenditure floors, administrative
cost and profit ceilings, premium stabilization programs, profit
sharing arrangements, and risk adjustment provisions;
- our estimates of amounts owed for such
cost expenditure floors, administrative cost and profit ceilings,
premium stabilization programs, profit-sharing arrangements, and
risk adjustment provisions;
- the Medicaid expansion cost corridors
in California, New Mexico, and Washington, and any other
retroactive adjustment to revenue where methodologies and
procedures are subject to interpretation or dependent upon
information about the health status of participants other than
Molina members;
- the interpretation and implementation
of at-risk premium rules and state contract performance
requirements regarding the achievement of certain quality measures,
and our ability to recognize revenue amounts associated
therewith;
- cyber-attacks or other privacy or data
security incidents resulting in an inadvertent unauthorized
disclosure of protected health information;
- the success of our health plan in
Puerto Rico, including the resolution of the Puerto Rico debt
crisis, payment of all amounts due under our Medicaid contract, the
effect of the PROMESA law, and our efforts to better manage the
health care costs of our Puerto Rico health plan;
- the success and renewal of our duals
demonstration programs in California, Illinois, Michigan, Ohio,
South Carolina, and Texas;
- the accurate estimation of incurred but
not reported or paid medical costs across our health plans;
- efforts by states to recoup previously
paid and recognized premium amounts;
- the continuation and renewal of the
government contracts of our health plans, Molina Medicaid
Solutions, and Pathways, and the terms under which such contracts
are renewed;
- complications, member confusion, or
enrollment backlogs related to the annual renewal of Medicaid
coverage;
- government audits and reviews, or
potential investigations, and any fine, sanction, enrollment
freeze, monitoring program, or premium recovery that may result
therefrom, including any potential demand by the state of New
Mexico to recover purportedly underpaid premium taxes;
- changes with respect to our provider
contracts and the loss of providers;
- approval by state regulators of
dividends and distributions by our health plan subsidiaries;
- changes in funding under our contracts
as a result of regulatory changes, programmatic adjustments, or
other reforms;
- high dollar claims related to
catastrophic illness;
- the favorable resolution of litigation,
arbitration, or administrative proceedings;
- the relatively small number of states
in which we operate health plans;
- the availability of adequate financing
on acceptable terms to fund and capitalize our expansion and
growth, repay our outstanding indebtedness at maturity and meet our
liquidity needs, including the interest expense and other costs
associated with such financing;
- our failure to comply with the
financial or other covenants in our credit agreement or the
indentures governing our outstanding notes;
- the sufficiency of our funds on hand to
pay the amounts due upon conversion or maturity of our outstanding
notes;
- the failure of a state in which we
operate to renew its federal Medicaid waiver;
- changes generally affecting the managed
care or Medicaid management information systems industries;
- increases in government surcharges,
taxes, and assessments, including but not limited to the
deductibility of certain compensation costs;
- newly emergent viruses or widespread
epidemics, public catastrophes or terrorist attacks, and associated
public alarm;
- increasing competition and
consolidation in the Medicaid industry;
and numerous other risk factors, including those discussed in
our periodic reports and filings with the Securities and Exchange
Commission. These reports can be accessed under the investor
relations tab of our website or on the SEC’s website at
sec.gov. Given these risks and
uncertainties, we can give no assurances that our forward-looking
statements will prove to be accurate, or that any other results or
events projected or contemplated by our forward-looking statements
will in fact occur, and we caution investors not to place undue
reliance on these statements. All forward-looking statements in
this release represent our judgment as of August 2, 2017, and we
disclaim any obligation to update any forward-looking statements to
conform the statement to actual results or changes in our
expectations.
MOLINA HEALTHCARE, INC.
UNAUDITED CONSOLIDATED STATEMENTS OF
OPERATIONS
Three Months Ended June 30, Six Months Ended June
30, 2017 2016 2017
2016 (Dollar amounts in millions, except per-share
amounts) Revenue: Premium revenue $ 4,740 $ 4,029 $ 9,388 $
8,024 Service revenue 129 135 260 275 Premium tax revenue 114 109
225 218 Health insurer fee revenue — 76 — 166 Investment income and
other revenue 16 10 30 19 Total revenue
4,999 4,359 9,903 8,702 Operating
expenses: Medical care costs 4,491 3,594 8,602 7,182 Cost of
service revenue 124 116 246 243 General and administrative expenses
405 351 844 691 Premium tax expenses 114 109 225 218 Health insurer
fee expenses — 50 — 108 Depreciation and amortization 37 34 76 66
Impairment losses 72 — 72 — Restructuring and separation costs 43
— 43 — Total operating expenses 5,286
4,254 10,108 8,508 Operating (loss)
income (287 ) 105 (205 ) 194 Other expenses (income),
net: Interest expense 27 25 53 50 Other income, net — —
(75 ) — Total other expenses (income), net 27
25 (22 ) 50 (Loss) income before income tax (benefit)
expense (314 ) 80 (183 ) 144 Income tax (benefit) expense (84 ) 47
(30 ) 87 Net (loss) income $ (230 ) $ 33 $
(153 ) $ 57 Net (loss) income per diluted share $
(4.10 ) $ 0.58 $ (2.74 ) $ 1.01 Diluted
weighted average shares outstanding 56.2 55.5 56.1
56.3
Operating Statistics: Medical care
ratio (1) 94.8 % 89.2 % 91.6 % 89.5 % G&A ratio (2) 8.1 % 8.1 %
8.5 % 7.9 % Premium tax ratio (1) 2.4 % 2.6 % 2.3 % 2.6 % Effective
tax rate 26.8 % 59.8 % 16.0 % 60.7 % Net profit margin (2) (4.6 )%
0.7 % (1.5 )% 0.7 % __________________ (1) Medical care ratio
represents medical care costs as a percentage of premium revenue;
premium tax ratio represents premium tax expenses as a percentage
of premium revenue plus premium tax revenue. (2) G&A ratio
represents general and administrative expenses as a percentage of
total revenue. Net profit margin represents net (loss) income as a
percentage of total revenue.
MOLINA HEALTHCARE, INC.
UNAUDITED CONSOLIDATED BALANCE
SHEETS
June 30, December 31, 2017 2016
(In millions,except per-share
data)
ASSETS Current assets: Cash and cash equivalents $ 2,979 $
2,819 Investments 2,192 1,758 Restricted investments 325 —
Receivables 1,006 974 Income taxes refundable
68
39 Prepaid expenses and other current assets 159 131 Derivative
asset 440 267 Total current assets 7,169 5,988
Property, equipment, and capitalized software, net 449 454 Deferred
contract costs 93 86 Intangible assets, net 112 140 Goodwill 559
620 Restricted investments 118 110 Deferred income taxes 36 10
Other assets 47 41 $ 8,583 $ 7,449
LIABILITIES AND STOCKHOLDERS’ EQUITY Current liabilities:
Medical claims and benefits payable $ 2,077 $ 1,929 Amounts due
government agencies 1,844 1,202 Accounts payable and accrued
liabilities 375 385 Deferred revenue 284 315 Current portion of
long-term debt 773 472 Derivative liability 440 267
Total current liabilities 5,793 4,570 Senior notes 1,017 975 Lease
financing obligations 198 198 Deferred income taxes — 15 Other
long-term liabilities 54 42 Total liabilities 7,062
5,800 Stockholders’ equity: Common stock, $0.001 par
value; 150 shares authorized; outstanding: 57 shares at June 30,
2017 and December 31, 2016 — — Preferred stock, $0.001 par value;
20 shares authorized, no shares issued and outstanding — —
Additional paid-in capital 865 841 Accumulated other comprehensive
loss (1 ) (2 ) Retained earnings 657 810 Total
stockholders’ equity 1,521 1,649 $ 8,583 $
7,449
MOLINA HEALTHCARE, INC.
UNAUDITED CONDENSED CONSOLIDATED
STATEMENTS OF CASH FLOWS
Three Months Ended June 30, Six Months Ended June
30, 2017 2016 2017
2016 (In millions) Operating activities: Net
(loss) income $ (230 ) $ 33 $ (153 ) $ 57 Adjustments to reconcile
net (loss) income to net cash (used in) provided by operating
activities: Depreciation and amortization 47 45 96 89 Impairment
losses 72 — 72 — Deferred income taxes (36 ) 9 (41 ) 39 Share-based
compensation, including accelerated share-based compensation 29 9
35 16 Amortization of convertible senior notes and lease financing
obligations 8 7 16 15 Other, net 4 5 7 11 Changes in operating
assets and liabilities: Receivables — (149 ) (32 ) (415 ) Prepaid
expenses and other assets (26 ) 59 (38 ) (143 ) Medical claims and
benefits payable 151 (173 ) 148 82 Amounts due government agencies
269 328 642 509 Accounts payable and accrued liabilities (68 ) (58
) (18 ) 147 Deferred revenue (178 ) 10 (32 ) (119 ) Income taxes
(89 ) 14 (30 ) (10 ) Net cash (used in) provided by
operating activities (47 ) 139 672 278
Investing activities: Purchases of investments (903 ) (363 ) (1,636
) (974 ) Proceeds from sales and maturities of investments 441 464
874 812 Purchases of property, equipment, and capitalized software
(34 ) (56 ) (60 ) (102 ) (Increase) decrease in restricted
investments held-to-maturity (3 ) 9 (10 ) 5 Net cash paid in
business combinations — (6 ) — (8 ) Other, net (7 ) (7 ) (13 ) (6 )
Net cash (used in) provided by investing activities (506 ) 41
(845 ) (273 ) Financing activities: Proceeds from senior
notes offerings, net of issuance costs 325 — 325 — Proceeds from
employee stock plans 10 10 11 10 Other, net (1 ) (1 ) (3 ) 1
Net cash provided by financing activities 334 9 333
11 Net (decrease) increase in cash and cash
equivalents (219 ) 189 160 16 Cash and cash equivalents at
beginning of period 3,198 2,156 2,819 2,329
Cash and cash equivalents at end of period $ 2,979 $
2,345 $ 2,979 $ 2,345
MOLINA HEALTHCARE, INC.
UNAUDITED HEALTH PLANS SEGMENT
MEMBERSHIP
June 30, 2017
December 31,2016
June 30, 2016
Ending Membership by Program: Temporary Assistance for Needy
Families (TANF) and Children’s Health Insurance Program (CHIP)
2,517,000 2,536,000 2,500,000 Marketplace 949,000 526,000 597,000
Medicaid Expansion 678,000 673,000 654,000 Aged, Blind or Disabled
(ABD) 408,000 396,000 387,000 Medicare-Medicaid Plan (MMP) -
Integrated 54,000 51,000 51,000 Medicare Special Needs Plans 44,000
45,000 44,000 4,650,000 4,227,000
4,233,000
Ending Membership by Health Plan: California
766,000 683,000 680,000 Florida 672,000 553,000 565,000 Illinois
163,000 195,000 201,000 Michigan 414,000 391,000 393,000 New Mexico
266,000 254,000 251,000 New York (1) 34,000 35,000 — Ohio 351,000
332,000 341,000 Puerto Rico 322,000 330,000 336,000 South Carolina
112,000 109,000 105,000 Texas 465,000 337,000 367,000 Utah 167,000
146,000 151,000 Washington 788,000 736,000 709,000 Wisconsin
130,000 126,000 134,000 4,650,000 4,227,000
4,233,000 ____________________ (1) The New York health plan
was acquired on August 1, 2016.
MOLINA HEALTHCARE, INC.
UNAUDITED SELECTED HEALTH PLANS SEGMENT
FINANCIAL DATA
(In millions, except percentages and
per-member per-month amounts)
Three Months Ended June 30, 2017 Member
Months (1)
Premium Revenue Medical Care
Costs MCR (2)
MedicalMargin
Total PMPM Total
PMPM TANF and CHIP 7.6 $ 1,391 $ 182.47 $ 1,315 $ 172.48
94.5 % $ 76 Medicaid Expansion 2.1 786 383.07 689 335.26 87.5 97
ABD 1.2 1,285 1,053.89 1,245 1,020.85 96.9 40
Total Medicaid 10.9 3,462 317.79 3,249
298.10 93.8 213 MMP 0.1 361 2,217.44 333 2,050.20 92.5 28
Medicare 0.2 148 1,126.14 126 963.34 85.5 22
Total Medicare 0.3 509 1,730.91 459
1,565.65 90.5 50 Excluding Marketplace 11.2 3,971 354.87
3,708 331.36 93.4 263 Marketplace 2.8 769 267.37 783
272.37 101.9 (14 ) 14.0 $ 4,740 $ 336.98 $
4,491 $ 319.29 94.8 % $ 249
Three
Months Ended June 30, 2016 Member
Months (1)
Premium Revenue Medical Care Costs MCR
(2)
MedicalMargin
Total PMPM Total PMPM TANF and CHIP 7.5
$ 1,302 $ 173.57 $ 1,202 $ 160.26 92.3 % $ 100 Medicaid Expansion
1.9 742 378.19 634 323.56 85.6 108 ABD 1.2 1,168
991.38 1,038 881.80 88.9 130 Total Medicaid 10.6
3,212 301.86 2,874 270.27 89.5 338 MMP
0.2 315 2,093.29 270 1,792.78 85.6 45 Medicare 0.2 129
997.44 127 974.30 97.7 2 Total Medicare 0.4
444 1,584.77 397 1,412.96 89.2 47
Excluding Marketplace 11.0 3,656 334.86 3,271 299.67 89.5 385
Marketplace 1.8 373 206.88 323 178.79 86.4 50
12.8 $ 4,029 $ 316.72 $ 3,594 $ 282.54
89.2 % $ 435 ____________________ (1) A member month is
defined as the aggregate of each month’s ending membership for the
period presented. (2) The MCR represents medical costs as a
percentage of premium revenue.
MOLINA HEALTHCARE, INC.
UNAUDITED SELECTED HEALTH PLANS SEGMENT
FINANCIAL DATA
(In millions, except percentages and
per-member per-month amounts)
Six Months Ended June 30, 2017 Member
Months (1)
Premium Revenue Medical Care
Costs MCR (2)
MedicalMargin
Total PMPM Total
PMPM TANF and CHIP 15.3 $ 2,793 $ 182.58 $ 2,619 $ 171.25
93.8 % $ 174 Medicaid Expansion 4.1 1,603 390.88 1,378 335.88 85.9
225 ABD 2.4 2,481 1,030.68 2,375 986.54 95.7
106 Total Medicaid 21.8 6,877 315.39 6,372
292.22 92.7 505 MMP 0.3 705 2,152.75 640 1,954.15 90.8 65 Medicare
0.3 286 1,097.36 243 933.20 85.0 43 Total
Medicare 0.6 991 1,685.72 883 1,502.36 89.1
108 Excluding Marketplace 22.4 7,868 351.35 7,255 323.98 92.2 613
Marketplace 5.7 1,520 264.77 1,347 234.62 88.6
173 28.1 $ 9,388 $ 333.68 $ 8,602 $ 305.74
91.6 % $ 786
Six Months Ended June 30, 2016
Member
Months (1)
Premium Revenue Medical Care Costs MCR
(2)
MedicalMargin
Total PMPM Total PMPM TANF and CHIP
14.9 $ 2,626 $ 176.00 $ 2,400 $ 160.85 91.4 % $ 226 Medicaid
Expansion 3.8 1,421 371.82 1,208 316.13 85.0 213 ABD 2.4
2,280 976.58 2,079 890.71 91.2 201 Total Medicaid
21.1 6,327 300.19 5,687 269.86 89.9 640 MMP
0.3 655 2,157.55 587 1,932.73 89.6 68 Medicare 0.3 260
1,013.04 251 977.35 96.5 9 Total Medicare 0.6
915 1,633.08 838 1,494.92 91.5 77 Excluding
Marketplace 21.7 7,242 334.74 6,525 301.61 90.1 717 Marketplace 3.4
782 228.19 657 191.62 84.0 125 25.1 $
8,024 $ 320.17 $ 7,182 $ 286.57 89.5 % $ 842
____________________ (1) A member month is defined as the aggregate
of each month’s ending membership for the period presented. (2) The
MCR represents medical costs as a percentage of premium revenue.
MOLINA HEALTHCARE, INC.
UNAUDITED SELECTED HEALTH PLANS SEGMENT
FINANCIAL DATA—NON-MARKETPLACE
(In millions, except percentages and
per-member per-month amounts)
Three Months Ended June 30, 2017 Member
Months (1)
Premium Revenue Medical Care
Costs MCR (2)
MedicalMargin
Total PMPM Total
PMPM California 1.9 $ 598 $ 318.89 $ 539 $ 287.36 90.1 % $
59 Florida 1.1 380 347.20 370 337.92 97.3 10 Illinois 0.5 149
289.51 174 336.76 116.3 (25 ) Michigan 1.1 390 333.26 358 305.40
91.6 32 New Mexico 0.8 321 443.13 311 428.58 96.7 10 New York (3)
0.1 46 457.96 45 442.16 96.5 1 Ohio 1.0 529 536.90 489 496.41 92.5
40 Puerto Rico 0.9 179 184.28 189 194.42 105.5 (10 ) South Carolina
0.4 111 326.57 102 304.14 93.1 9 Texas 0.7 524 752.01 473 679.43
90.3 51 Utah 0.3 89 313.93 76 267.15 85.1 13 Washington 2.2 618
276.90 546 244.58 88.3 72 Wisconsin 0.2 34 170.98 26 130.54 76.3 8
Other (4) — 3 — 10 — — (7 ) 11.2 $
3,971 $ 354.87 $ 3,708 $ 331.36 93.4 % $ 263
Three Months Ended June 30, 2016 Member
Months (1)
Premium Revenue Medical Care Costs MCR
(2)
MedicalMargin
Total PMPM Total PMPM California 1.9 $
519 $ 281.99 $ 472 $ 256.37 90.9 % $ 47 Florida 1.0 314 312.23 289
287.84 92.2 25 Illinois 0.6 154 256.17 137 227.71 88.9 17 Michigan
1.2 366 312.88 332 283.89 90.7 34 New Mexico 0.7 328 468.35 296
422.37 90.2 32 New York (3) — — — — — — — Ohio 0.9 474 479.41 427
431.46 90.0 47 Puerto Rico 1.0 170 169.04 175 173.49 102.6 (5 )
South Carolina 0.3 87 277.22 71 226.27 81.6 16 Texas 0.8 580 784.32
470 633.94 80.8 110 Utah 0.3 86 293.39 74 254.59 86.8 12 Washington
2.1 538 263.41 484 237.43 90.1 54 Wisconsin 0.2 36 166.95 27 120.69
72.3 9 Other (4) — 4 — 17 — — (13 ) 11.0
$ 3,656 $ 334.86 $ 3,271 $ 299.67 89.5 % $ 385
____________________ (1) A member month is defined as the
aggregate of each month’s ending membership for the period
presented. (2) The MCR represents medical costs as a percentage of
premium revenue. (3) The New York health plan was acquired on
August 1, 2016. (4) “Other” medical care costs include primarily
medically related administrative costs at the parent company, and
direct delivery costs.
MOLINA HEALTHCARE, INC.
UNAUDITED SELECTED HEALTH PLANS SEGMENT
FINANCIAL DATA—NON-MARKETPLACE
(In millions, except percentages and
per-member per-month amounts)
Six Months Ended June 30, 2017 Member
Months (1)
Premium Revenue Medical Care
Costs MCR (2)
MedicalMargin
Total PMPM Total
PMPM California 3.7 $ 1,170 $ 313.76 $ 1,023 $ 274.42 87.5 %
$ 147 Florida 2.2 744 343.29 722 333.23 97.1 22 Illinois 1.1 310
282.66 354 322.63 114.1 (44 ) Michigan 2.3 772 330.34 690 295.02
89.3 82 New Mexico 1.5 629 432.98 610 419.65 96.9 19 New York (3)
0.2 92 449.48 87 425.72 94.7 5 Ohio 2.0 1,049 532.35 951 482.73
90.7 98 Puerto Rico 1.9 362 185.40 354 181.24 97.8 8 South Carolina
0.7 216 321.85 200 298.79 92.8 16 Texas 1.4 1,051 751.94 962 687.96
91.5 89 Utah 0.6 178 313.56 148 260.43 83.1 30 Washington 4.4 1,223
275.05 1,081 243.18 88.4 142 Wisconsin 0.4 67 168.16 53 133.25 79.2
14 Other (4) — 5 — 20 — — (15 ) 22.4 $
7,868 $ 351.35 $ 7,255 $ 323.98 92.2 % $ 613
Six Months Ended June 30, 2016 Member
Months (1)
Premium Revenue Medical Care Costs MCR
(2)
MedicalMargin
Total PMPM Total PMPM California 3.7 $
1,028 $ 281.37 $ 918 $ 251.15 89.3 % $ 110 Florida 2.0 639 322.01
575 290.08 90.1 64 Illinois 1.2 303 261.43 269 232.06 88.8 34
Michigan 2.4 751 317.13 678 286.40 90.3 73 New Mexico 1.4 651
465.65 580 414.80 89.1 71 New York (3) — — — — — — — Ohio 1.9 952
485.86 869 443.08 91.2 83 Puerto Rico 2.0 351 172.98 349 171.95
99.4 2 South Carolina 0.6 171 276.61 138 223.58 80.8 33 Texas 1.5
1,116 752.54 982 661.63 87.9 134 Utah 0.6 172 295.69 150 259.29
87.7 22 Washington 4.0 1,030 259.79 931 234.95 90.4 99 Wisconsin
0.4 72 164.90 52 118.37 71.8 20 Other (4) — 6 — 34
— — (28 ) 21.7 $ 7,242 $ 334.74 $ 6,525
$ 301.61 90.1 % $ 717 ____________________ (1) A member
month is defined as the aggregate of each month’s ending membership
for the period presented. (2) The MCR represents medical costs as a
percentage of premium revenue. (3) The New York health plan was
acquired on August 1, 2016. (4) “Other” medical care costs include
primarily medically related administrative costs at the parent
company, and direct delivery costs.
MOLINA HEALTHCARE, INC.
UNAUDITED SELECTED HEALTH PLANS SEGMENT
FINANCIAL DATA—MARKETPLACE
(In millions, except percentages and
per-member per-month amounts)
Three Months Ended June 30, 2017 Member
Months (1)
Premium Revenue Medical Care
Costs MCR (2)
MedicalMargin
Total PMPM Total
PMPM California 0.5 $ 81 $ 186.90 $ 67 $ 154.23 82.5 % $ 14
Florida 0.9 269 284.60 317 336.78 118.3 (48 ) Michigan 0.1 16
204.15 10 135.89 66.6 6 New Mexico — 31 367.98 23 266.91 72.5 8
Ohio — 24 377.94 27 404.20 106.9 (3 ) Texas 0.7 177 247.49 129
180.92 73.1 48 Utah 0.2 41 186.87 53 239.50 128.2 (12 ) Washington
0.2 44 317.42 49 359.87 113.4 (5 ) Wisconsin 0.2 86 434.01 109
550.81 126.9 (23 ) Other (3) — — — (1 ) — — 1
2.8 $ 769 $ 267.37 $ 783 $ 272.37 101.9 % $
(14 )
Three Months Ended June 30, 2016
Member
Months (1)
Premium Revenue Medical Care Costs MCR
(2)
MedicalMargin
Total PMPM Total PMPM California 0.1 $
35 $ 159.56 $ 21 $ 99.15 62.1 % $ 14 Florida 0.8 150 217.96 137
198.93 91.3 13 Michigan — 3 235.15 2 176.34 75.0 1 New Mexico 0.1
14 240.40 9 164.00 68.2 5 Ohio 0.1 9 294.90 6 210.36 71.3 3 Texas
0.3 55 146.76 29 78.56 53.5 26 Utah 0.2 24 146.37 32 195.18 133.3
(8 ) Washington — 21 291.91 16 205.59 70.4 5 Wisconsin 0.2 63
335.32 69 369.55 110.2 (6 ) Other (3) — (1 ) — 2 — —
(3 ) 1.8 $ 373 $ 206.88 $ 323 $ 178.79 86.4 %
$ 50 ____________________ (1) A member month is defined as
the aggregate of each month’s ending membership for the period
presented. (2) The MCR represents medical costs as a percentage of
premium revenue. (3) “Other” medical care costs include primarily
medically related administrative costs at the parent company, and
direct delivery costs.
MOLINA HEALTHCARE, INC.
UNAUDITED SELECTED HEALTH PLANS SEGMENT
FINANCIAL DATA—MARKETPLACE
(In millions, except percentages and
per-member per-month amounts)
Six Months Ended June 30, 2017 Member
Months (1)
Premium Revenue Medical Care
Costs MCR (2)
MedicalMargin
Total PMPM Total
PMPM California 0.9 $ 153 $ 185.68 $ 93 $ 112.20 60.4 % $ 60
Florida 1.9 561 288.81 523 269.48 93.3 38 Michigan 0.2 27 177.12 17
116.21 65.6 10 New Mexico 0.1 53 317.10 42 249.90 78.8 11 Ohio 0.1
45 356.20 44 339.26 95.2 1 Texas 1.4 334 235.07 242 171.07 72.8 92
Utah 0.4 86 194.68 104 233.85 120.1 (18 ) Washington 0.3 81 310.26
95 362.78 116.9 (14 ) Wisconsin 0.4 180 443.86 190 469.01 105.7 (10
) Other (3) — — — (3 ) — — 3 5.7 $
1,520 $ 264.77 $ 1,347 $ 234.62 88.6 % $ 173
Six Months Ended June 30, 2016 Member
Months (1)
Premium Revenue Medical Care Costs MCR
(2)
MedicalMargin
Total PMPM Total PMPM California 0.3 $
67 $ 173.55 $ 44 $ 115.80 66.7 % $ 23 Florida 1.4 314 230.11 264
193.24 84.0 50 Michigan — 5 208.83 3 141.43 67.7 2 New Mexico 0.1
27 251.96 21 192.53 76.4 6 Ohio 0.1 19 330.26 13 241.55 73.1 6
Texas 0.7 139 199.62 92 132.77 66.5 47 Utah 0.3 52 169.84 58 187.64
110.5 (6 ) Washington 0.1 35 267.82 27 200.50 74.9 8 Wisconsin 0.4
124 348.84 136 382.15 109.5 (12 ) Other (3) — — — (1
) — — 1 3.4 $ 782 $ 228.19 $ 657 $
191.62 84.0 % $ 125 ____________________ (1) A member month
is defined as the aggregate of each month’s ending membership for
the period presented. (2) The MCR represents medical costs as a
percentage of premium revenue. (3) “Other” medical care costs
include primarily medically related administrative costs at the
parent company, and direct delivery costs.
MOLINA HEALTHCARE, INC.
UNAUDITED SELECTED HEALTH PLANS SEGMENT
FINANCIAL DATA—TOTAL
(In millions, except percentages and
per-member per-month amounts)
Three Months Ended June 30, 2017 Member
Months (1)
Premium Revenue Medical Care
Costs MCR (2)
MedicalMargin
Total PMPM Total
PMPM California 2.4 $ 679 $ 294.09 $ 606 $ 262.34 89.2 % $
73 Florida 2.0 649 318.21 687 337.39 106.0 (38 ) Illinois 0.5 149
289.51 174 336.76 116.3 (25 ) Michigan 1.2 406 325.38 368 295.06
90.7 38 New Mexico 0.8 352 435.34 334 411.83 94.6 18 New York (3)
0.1 46 457.96 45 442.16 96.5 1 Ohio 1.0 553 527.14 516 490.75 93.1
37 Puerto Rico 0.9 179 184.28 189 194.42 105.5 (10 ) South Carolina
0.4 111 326.57 102 304.14 93.1 9 Texas 1.4 701 495.93 602 426.41
86.0 99 Utah 0.5 130 258.10 129 255.00 98.8 1 Washington 2.4 662
279.21 595 251.16 90.0 67 Wisconsin 0.4 120 303.59 135 342.43 112.8
(15 ) Other (4) — 3 — 9 — — (6 ) 14.0 $
4,740 $ 336.98 $ 4,491 $ 319.29 94.8 % $ 249
Three Months Ended June 30, 2016
MemberMonths (1)
Premium Revenue Medical Care Costs MCR
(2)
MedicalMargin
Total PMPM Total PMPM California 2.0 $
554 $ 268.95 $ 493 $ 239.63 89.1 % $ 61 Florida 1.8 464 273.90 426
251.69 91.9 38 Illinois 0.6 154 256.17 137 227.71 88.9 17 Michigan
1.2 369 312.18 334 282.86 90.6 35 New Mexico 0.8 342 451.72 305
403.52 89.3 37 New York (3) — — — — — — — Ohio 1.0 483 473.91 433
424.87 89.7 50 Puerto Rico 1.0 170 169.04 175 173.49 102.6 (5 )
South Carolina 0.3 87 277.22 71 226.27 81.6 16 Texas 1.1 635 571.14
499 448.23 78.5 136 Utah 0.5 110 240.26 106 233.12 97.0 4
Washington 2.1 559 264.40 500 236.32 89.4 59 Wisconsin 0.4 99
244.88 96 235.88 96.3 3 Other (4) — 3 — 19 — —
(16 ) 12.8 $ 4,029 $ 316.72 $ 3,594 $ 282.54
89.2 % $ 435 ____________________ (1) A member month is
defined as the aggregate of each month’s ending membership for the
period presented. (2) The MCR represents medical costs as a
percentage of premium revenue. (3) The New York health plan was
acquired on August 1, 2016. (4) “Other” medical care costs include
primarily medically related administrative costs at the parent
company, and direct delivery costs.
MOLINA HEALTHCARE, INC.
UNAUDITED SELECTED HEALTH PLANS SEGMENT
FINANCIAL DATA—TOTAL
(In millions, except percentages and
per-member per-month amounts)
Six Months Ended June 30, 2017 Member
Months (1)
Premium Revenue Medical Care
Costs MCR (2)
MedicalMargin
Total PMPM Total
PMPM California 4.6 $ 1,323 $ 290.56 $ 1,116 $ 245.02 84.3 %
$ 207 Florida 4.1 1,305 317.53 1,245 303.09 95.5 60 Illinois 1.1
310 282.66 354 322.63 114.1 (44 ) Michigan 2.5 799 321.10 707
284.24 88.5 92 New Mexico 1.6 682 421.11 652 402.27 95.5 30 New
York (3) 0.2 92 449.48 87 425.72 94.7 5 Ohio 2.1 1,094 521.57 995
473.95 90.9 99 Puerto Rico 1.9 362 185.40 354 181.24 97.8 8 South
Carolina 0.7 216 321.85 200 298.79 92.8 16 Texas 2.8 1,385 491.46
1,204 427.48 87.0 181 Utah 1.0 264 261.42 252 248.77 95.2 12
Washington 4.7 1,304 276.99 1,176 249.79 90.2 128 Wisconsin 0.8 247
307.50 243 302.95 98.5 4 Other (4) — 5 — 17 —
— (12 ) 28.1 $ 9,388 $ 333.68 $ 8,602 $ 305.74
91.6 % $ 786
Six Months Ended June 30,
2016 Member
Months (1)
Premium Revenue Medical Care Costs MCR
(2)
MedicalMargin
Total PMPM Total PMPM California 4.0 $
1,095 $ 271.14 $ 962 $ 238.30 87.9 % $ 133 Florida 3.4 953 284.53
839 250.58 88.1 114 Illinois 1.2 303 261.43 269 232.06 88.8 34
Michigan 2.4 756 316.18 681 285.13 90.2 75 New Mexico 1.5 678
450.62 601 399.17 88.6 77 New York (3) — — — — — — — Ohio 2.0 971
481.44 882 437.35 90.8 89 Puerto Rico 2.0 351 172.98 349 171.95
99.4 2 South Carolina 0.6 171 276.61 138 223.58 80.8 33 Texas 2.2
1,255 575.87 1,074 492.65 85.5 181 Utah 0.9 224 252.08 208 234.46
93.0 16 Washington 4.1 1,065 260.05 958 233.84 89.9 107 Wisconsin
0.8 196 247.57 188 236.92 95.7 8 Other (4) — 6 — 33
— — (27 ) 25.1 $ 8,024 $ 320.17 $ 7,182
$ 286.57 89.5 % $ 842 ____________________ (1) A member
month is defined as the aggregate of each month’s ending membership
for the period presented. (2) The MCR represents medical costs as a
percentage of premium revenue. (3) The New York health plan was
acquired on August 1, 2016. (4) “Other” medical care costs include
primarily medically related administrative costs at the parent
company, and direct delivery costs.
MOLINA HEALTHCARE, INC.
UNAUDITED SELECTED HEALTH PLANS SEGMENT
FINANCIAL DATA
(In millions, except percentages and
per-member per-month amounts)
The following tables provide the details
of our medical care costs for the periods indicated:
Three Months Ended June 30, 2017
2016 Amount PMPM
% of
Total
Amount PMPM % of
Total
Fee for service $ 3,348 $ 238.04 74.5 % $ 2,620 $ 206.01 72.9 %
Pharmacy 650 46.23 14.5 529 41.59 14.7 Capitation 356 25.29 7.9 304
23.87 8.5 Direct delivery 22 1.54 0.5 18 1.39 0.5 Other 115
8.19 2.6 123 9.68 3.4 $
4,491 $ 319.29 100.0 % $ 3,594 $ 282.54 100.0 %
Six Months Ended June 30, 2017 2016
Amount PMPM % of
Total
Amount PMPM % of
Total
Fee for service $ 6,434 $ 228.68 74.8 % $ 5,357 $ 213.77 74.6 %
Pharmacy 1,266 45.00 14.7 1,054 42.05 14.7 Capitation 680 24.17 7.9
599 23.87 8.3 Direct delivery 44 1.56 0.5 34 1.36 0.5 Other
178 6.33 2.1 138 5.52 1.9
$ 8,602 $ 305.74 100.0 % $ 7,182 $ 286.57 100.0 %
The following table provides the details of our medical
claims and benefits payable as of the dates indicated:
June 30, December 31, 2017 2016
Fee-for-service claims incurred but not paid (IBNP) $ 1,478 $ 1,352
Pharmacy payable 121 112 Capitation payable 45 37 Other (1)
433 428 $ 2,077 $ 1,929
____________________ (1) “Other” medical claims and benefits
payable include amounts payable to certain providers for which we
act as an intermediary on behalf of various state agencies without
assuming financial risk. Such receipts and payments do not impact
our consolidated statements of operations. As of June 30, 2017 and
December 31, 2016, we had recorded non-risk provider payables of
approximately $111 million and $225 million, respectively.
MOLINA HEALTHCARE, INC.
UNAUDITED CHANGE IN MEDICAL CLAIMS AND
BENEFITS PAYABLE
(Dollars in millions, except per-member
amounts)
Our claims liability includes a provision
for adverse claims deviation based on historical experience and
other factors including, but not limited to, variations in claims
payment patterns, changes in utilization and cost trends, known
outbreaks of disease, and large claims. Our reserving methodology
is consistently applied across all periods presented. The amounts
displayed for “Components of medical care costs related to: Prior
period” represent the amount by which our original estimate of
claims and benefits payable at the beginning of the period were
more than the actual amount of the liability based on information
(principally the payment of claims) developed since that liability
was first reported. The following table presents the components of
the change in medical claims and benefits payable for the periods
indicated:
Six Months Ended June 30,
Year EndedDecember
31,2016
2017 2016 Medical claims and benefits
payable, beginning balance $ 1,929 $ 1,685 $ 1,685 Components of
medical care costs related to: Current period 8,633 7,371 14,966
Prior period (31 ) (189 ) (192 ) Total medical care costs 8,602
7,182 14,774 Change in non-risk
provider payables (114 ) 24 58 Payments for medical
care costs related to: Current period 6,883 5,885 13,304 Prior
period 1,457 1,240 1,284 Total paid 8,340
7,125 14,588 Medical claims and benefits
payable, ending balance $ 2,077 $ 1,766 $ 1,929
Benefit from prior period as a percentage of: Balance
at beginning of period 1.6 % 11.3 % 11.4 % Premium revenue,
trailing twelve months 0.2 % 1.3 % 1.2 % Medical care costs,
trailing twelve months 0.2 % 1.4 % 1.3 % Days in claims
payable, fee for service (1) 46 48 47 ____________________
(1) Claims payable includes primarily IBNP. Additionally, it
includes certain fee-for-service payables reported in “Other”
medical claims and benefits payable amounting to $157 million, $74
million and $94 million, as of June 30, 2017, June 30, 2016, and
December 31, 2016, respectively.
MOLINA HEALTHCARE, INC.
UNAUDITED NON-GAAP FINANCIAL
MEASURES
We use non-GAAP financial measures as
supplemental metrics in evaluating our financial performance,
making financing and business decisions, and forecasting and
planning for future periods. For these reasons, management believes
such measures are useful supplemental measures to investors in
comparing our performance to the performance of other public
companies in the health care industry. These non-GAAP financial
measures should be considered as supplements to, and not as
substitutes for or superior to, GAAP measures. See further
information regarding non-GAAP measures below the tables (in
millions, except per diluted share amounts).
Three Months Ended June 30, Six Months Ended June
30, 2017 2016 2017
2016 Net (loss) income $ (230 ) $ 33 $ (153 )
$ 57 Adjustments: Depreciation, and amortization of intangible
assets and capitalized software 44 39 90 76 Interest expense 27 25
53 50 Income tax (benefit) expense (84 ) 47 (30 ) 87 EBITDA
$ (243 ) $ 144 $ (40 ) $ 270
Three Months Ended June 30, Six Months Ended June
30, 2017 2016 2017
2016 Amount
PerDilutedshare
Amount
PerDiluted
share
Amount
PerDiluted
share
Amount
PerDilutedshare
Net (loss) income $ (230 ) $ (4.10 ) $ 33 $ 0.58 $ (153 ) $ (2.74 )
$ 57 $ 1.01 Adjustment: Amortization of intangible assets 8 0.14 8
0.14 17 0.30 15 0.27 Income tax effect (1) (3 ) (0.05 ) (3 ) (0.05
) (6 ) (0.11 ) (5 ) (0.10 ) Amortization of intangible assets, net
of tax effect 5 0.09 5 0.09 11
0.19 10 0.17 Adjusted net (loss) income $ (225
) $ (4.01 ) $ 38 $ 0.67 $ (142 ) $ (2.55 ) $ 67
$ 1.18
____________________
(1) Income tax effect of adjustment
calculated at the blended federal and state statutory tax rate of
37%.
The following are descriptions of the
adjustments made to GAAP measures used to calculate the non-GAAP
measures used in this news release:
Earnings before interest, taxes,
depreciation and amortization (EBITDA): Net (loss)
income (GAAP) less depreciation, and amortization of intangible
assets and capitalized software, interest expense and income tax
(benefit) expense. We believe that EBITDA is helpful in assessing
our ability to meet the cash demands of our operating units.
Adjusted net (loss) income: Net
(loss) income (GAAP) less amortization of intangible assets, net of
income tax effect calculated at the statutory tax rate of 37%. We
believe that adjusted net (loss) income is helpful in assessing our
financial performance exclusive of the non-cash impact of the
amortization of purchased intangibles.
Adjusted net (loss) income per diluted
share: Adjusted net (loss) income divided by weighted average
common shares outstanding on a fully diluted basis.
View source
version on businesswire.com: http://www.businesswire.com/news/home/20170802006305/en/
Molina Healthcare, Inc.Juan José Orellana, 562-435-3666, ext.
111143Investor Relations
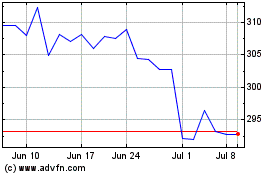
Molina Healthcare (NYSE:MOH)
Historical Stock Chart
From May 2024 to Jun 2024
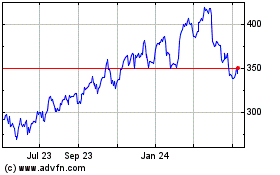
Molina Healthcare (NYSE:MOH)
Historical Stock Chart
From Jun 2023 to Jun 2024