CALQUENCE real-world evidence and long-term
follow-up data, as well as research collaborations, will reinforce
efficacy and safety across B-cell malignancies
Early clinical data will illustrate
potential of multiple pipeline molecules, including TNB-486
(AZD0486), across hematologic malignancies
Research from Alexion, AstraZeneca Rare
Disease, offers new insights to accelerate innovation and
improve time to diagnosis for several rare diseases
AstraZeneca will present 47 abstracts showcasing new data from
across its hematology portfolio and clinical pipeline,
demonstrating its commitment to redefining care for hard-to-treat
blood diseases at the 64th American Society of Hematology (ASH)
Annual Meeting and Exposition, December 10 to 13, 2022.
A total of eight approved and potential new medicines will be
featured across more than 10 types of blood cancers and rare
diseases, including data in chronic lymphocytic leukemia (CLL),
follicular lymphoma (FL), diffuse large B-cell lymphoma (DLBCL),
mantle cell lymphoma (MCL), paroxysmal nocturnal hemoglobinuria
(PNH), atypical hemolytic uremic syndrome (aHUS) and amyloid light
chain (AL) amyloidosis.
Anas Younes, Senior Vice President, Oncology R&D,
AstraZeneca, said: “At this year’s ASH Annual Meeting, our data
demonstrate the broad potential of our hematology pipeline and the
continued strength of our approved medicines. Data are being
highlighted from many of our early-stage molecules, including
clinical trials of TNB-486 (AZD0486), a B-cell targeting T-cell
engager, and presentations of long-term follow-up data will show
the consistent safety and efficacy profile of CALQUENCE.”
Gianluca Pirozzi, Senior Vice President, Head of Development and
Safety, Alexion, AstraZeneca Rare Disease said: “The depth and
breadth of Alexion data at this year’s ASH Annual Meeting reinforce
the importance of earlier diagnosis and disease management for rare
diseases that are often not well-understood. We will share research
across several therapy areas – including an oral presentation
demonstrating the potential of vemircopan, an investigational,
second-generation factor D inhibitor as monotherapy treatment of
paroxysmal nocturnal hemoglobinuria – underscoring our leadership
and unwavering commitment to driving critical innovations in rare
disease.”
CALQUENCE® (acalabrutinib) real-world evidence and
long-term follow-up data support consistent efficacy and safety
profile
- A post-hoc safety analysis from the head-to-head ELEVATE-RR
Phase III trial of CALQUENCE versus ibrutinib will further support
tolerability differences of CALQUENCE in relapsed or refractory
CLL.1
- Final long-term follow-up results of the Phase I/II trials
evaluating CALQUENCE monotherapy in front-line and relapsed or
refractory CLL will further support the continued efficacy and
safety CALQUENCE demonstrated in both settings.2,3
- An oral presentation of Phase II research sponsored by the
Dana-Farber Cancer Institute will show the efficacy and
tolerability of CALQUENCE combined with venetoclax and obinutuzumab
in a front-line, high-risk CLL population.4
- A retrospective pooled analysis will show the benefit of adding
obinutuzumab to CALQUENCE in the front-line CLL setting in patients
with select genomic characteristics.5
- An oral presentation of preliminary Phase II results sponsored
by Weill Cornell Medicine will show that CALQUENCE combined with
lenalidomide and rituximab is generally well-tolerated, highly
effective and produces high rates of minimal residual
disease-negative complete remission in front-line MCL.6
Novel treatment strategies with emerging pipeline molecules
exhibit therapeutic potential
- An oral presentation of interim Phase I results evaluating
TNB-486 (AZD0486), a CD19/CD3 next generation bispecific T-cell
engager, will show the potential of targeting CD19/CD3, leading to
an increase in anti-cancer activity in heavily pretreated patients
with B-cell non-Hodgkin lymphoma (NHL).7
- Results from Phase I and II trials of CDK9 inhibitor AZD4573
alone and with CALQUENCE will exhibit data on tolerability across a
broad range of hematologic malignancies, including relapsed or
refractory DLBCL.8,9
- Preliminary results from an ongoing Phase I trial will
demonstrate that Bcl-2/Bcl-xl inhibitor AZD0466 has been
well-tolerated in patients with advanced hematologic
malignancies.10
Innovating to help address the treatment needs of all
patients with PNH
- An oral presentation detailing interim results from a Phase II
open-label trial of vemircopan (ALXN2050) will highlight efficacy
and safety data from the treatment-naïve patient group,
establishing proof-of-concept as a monotherapy for PNH.11
- An interim analysis from an ongoing Phase IV trial assessing
the impact of switching to standard, weight-based intravenous
(i.v.) ULTOMIRIS® (ravulizumab-cwvz) from high-dose i.v. SOLIRIS®
(eculizumab) in adults with PNH will be presented.12
Improving diagnosis and management of life-threatening rare
diseases
- An analysis of data from the Global aHUS Registry, which
contains information on patients across more than 100 sites in more
than 20 countries, will highlight the importance of considering
aHUS as a diagnosis even in the presence of a triggering condition
or associated event.13
- An analysis of real-world patient data from the US Premier
Healthcare Database will expand on the potential of the PLASMIC
scoring system to aid in identifying people with aHUS and making
earlier treatment decisions.14
- An analysis of pediatric patients with hematopoietic stem cell
transplant-associated thrombotic microangiopathy (HSCT-TMA) will
provide insights on the correlation between complement activation
and endothelial damage in HSCT-TMA and the potential for useful
biomarkers indicative of this damage to inform diagnosis.15
- Results through one year on safety, tolerability and biomarker
data will be presented from a Phase II trial evaluating CAEL-101, a
potentially first-in-class monoclonal antibody, in adults with AL
amyloidosis.16
- A real-world analysis in a current population with AL
amyloidosis using Komodo Health US claims data will highlight the
need for greater awareness and understanding to accelerate time to
diagnosis.17
Key presentations during the 64th ASH Annual Meeting and
Exposition
Lead author
Abstract title
Presentation details
CALQUENCE (acalabrutinib)
Byrd, J
Final Results of the Phase 1/2 Study of
Acalabrutinib Monotherapy in Treatment-Naive Chronic Lymphocytic
Leukemia with >6 Years of Follow-Up
Abstract # 4431
Poster Session: 642. Chronic Lymphocytic
Leukemia: Clinical and Epidemiological: Poster III
December 12, 2022
18:00-20:00 CST
Location: Hall D (Ernest N. Morial
Convention Center)
Davids, MS
Contribution of Obinutuzumab to
Acalabrutinib Therapy in Patients with Treatment-Naive Chronic
Lymphocytic Leukemia: Analysis of Survival Outcomes by Genomic
Features
Abstract # 1815
Poster Session: 642. Chronic Lymphocytic
Leukemia: Clinical and Epidemiological: Poster I
December 10, 2022
17:30-19:30 CST
Location: Hall D (Ernest N. Morial
Convention Center)
Davies, AJ
Durable Responses from Acalabrutinib in
Combination with Rituximab, Cyclophosphamide, Doxorubicin,
Vincristine and Prednisolone (R-CHOP) as First Line Therapy for
Patients with Diffuse Large B-Cell Lymphoma (DLBCL): The ACCEPT
Phase Ib/II Single Arm Study
Abstract # 4265
Poster Session: 626. Aggressive Lymphomas:
Prospective Therapeutic Trials: Poster III
December 12, 2022
18:00-20:00 CST
Location: Hall D (Ernest N. Morial
Convention Center)
Furman, R
Phase 1/2 Study of Acalabrutinib
Monotherapy in Patients with Relapsed/Refractory Chronic
Lymphocytic Leukemia: Final Results with >4 Years of
Follow-Up
Abstract # 4434
Poster Session: 642. Chronic Lymphocytic
Leukemia: Clinical and Epidemiological: Poster III
December 12, 2022
18:00-20:00 CST
Location: Hall D (Ernest N. Morial
Convention Center)
Ruan, J
Phase 2 Trial of
Acalabrutinib-Lenalidomide-Rituximab (ALR) with Real-Time
Monitoring of MRD in Patients with Treatment-Naïve Mantle Cell
Lymphoma
Abstract # 73
Oral Session: 623. Mantle Cell,
Follicular, and Other Indolent B Cell Lymphomas: Clinical and
Epidemiological I
December 10, 2022
9:30 CST
Location: La Nouvelle Orleans Ballroom C
(Ernest N. Morial Convention Center)
Ryan, CE
Updated Results from a Multicenter, Phase
2 Study of Acalabrutinib, Venetoclax, Obinutuzumab (AVO) in a
Population of Previously Untreated Patients with CLL Enriched for
High-Risk Disease
Abstract # 344
Oral Session: 642. Chronic Lymphocytic
Leukemia: Clinical and Epidemiological: Targeted Triplet
Combinations and Richter’s Transformation
December 10, 2022
16:15 CST
Location: R06-R09 (Ernest N. Morial
Convention Center)
Seymour, JF
Assessing the Burden of Adverse Events in
a Head-to-Head Trial of Acalabrutinib Versus Ibrutinib in
Previously Treated Chronic Lymphocytic Leukemia (CLL)
Abstract # 3133
Poster Session: 642. Chronic Lymphocytic
Leukemia: Clinical and Epidemiological: Poster II
December 11, 2022
18:00-20:00 CST
Location: Hall D (Ernest N. Morial
Convention Center)
AZD0486 (CD19/CD3 T-cell
engager)
Hou, JZ
Interim Results of the Phase 1 Study of
Tnb-486, a Novel CD19xCD3 T-Cell Engager, in Patients with
Relapsed/Refractory (R/R) B-NHL
Abstract # 612
Oral Session: 623. Mantle Cell,
Follicular, and Other Indolent B Cell Lymphomas: Clinical and
Epidemiological IV
December 11, 2022
17:45 CST
Location: 278-282 (Ernest N. Morial
Convention Center)
AZD0466 (Bcl-2/Bcl-xL
inhibitor)
Arslan, S
Safety and Tolerability of AZD0466 as
Monotherapy for Patients with Advanced Hematological Malignancies.
Preliminary Results from an Ongoing Phase I/II Trial
Abstract # 4094
Poster Session: 616. Acute Myeloid
Leukemias: Investigational Therapies, Excluding Transplantation and
Cellular Immunotherapies: Poster III
December 12, 2022
18:00-20:00 CST
Location: Hall D (Ernest N. Morial
Convention Center)
AZD4573 (CDK9 inhibitor)
Brümmendorf, T
Safety, Tolerability, Pharmacokinetics
(PK) and Preliminary Antitumor Activity of the Cyclin-Dependent
Kinase-9 (CDK9) Inhibitor AZD4573 in Relapsed/Refractory
Hematological Malignancies: A Phase 1 First-in-Human Study
Abstract # 1353
Poster Session: 605. Molecular
Pharmacology and Drug Resistance: Lymphoid Neoplasms: Poster I
December 10, 2022
17:30-19:30 CST
Location: Hall D (Ernest N. Morial
Convention Center)
Strati, P
Phase 1b/2a Study of AZD4573 (CDK9i) and
Acalabrutinib in Patients with Relapsed/Refractory Diffuse Large
B-Cell Lymphoma (r/r DLBCL): Results from Dose-Escalation
Abstract # 2962
Poster Session: 627. Aggressive Lymphomas:
Clinical and Epidemiological: Poster II
December 11, 2022
18:00-20:00 CST
Location: Hall D (Ernest N. Morial
Convention Center)
VEMIRCOPAN (ALXN2050)
Browett, P
Vemircopan (ALXN2050) Monotherapy in
Paroxysmal Nocturnal Hemoglobinuria: Interim Data from a Phase 2
Open-Label Proof-of-Concept Study
Abstract # 294
Oral Session: 508. Bone Marrow Failure:
Acquired: Clinical Studies
December 10, 2022
17:15 CST
Location: 260-262 (Ernest N. Morial
Convention Center)
ULTOMIRIS (ravulizumab-cwvz)
Griffin, M
Terminal Complement Inhibition and Control
of Hemolysis in Paroxysmal Nocturnal Hemoglobinuria Following
Switching from High-Dose Eculizumab to Ravulizumab: An Interim
Analysis
Abstract # 1251
Poster Session: 508. Bone Marrow Failure:
Acquired: Poster I
December 10, 2022
17:30-19:30 CST
Location: Hall D (Ernest N. Morial
Convention Center)
ALXN1820
Dai, Y
A Phase 2a, Randomized, Open-Label Study
to Evaluate Multiple Dosing Regimens of Subcutaneous ALXN1820 in
Adult Patients with Sickle Cell Disease
Abstract # 3713
Poster Session: 114. Hemoglobinopathies,
Excluding Thalassemia: Clinical and Epidemiological: Poster III
December 12, 2022
18:00-20:00 CST
Location: Hall D (Ernest N. Morial
Convention Center)
CAEL-101
Valent, J
1-Year Results from a Phase 2 Study to
Determine Safety and Tolerability of Treating Patients with
Light-Chain (AL) Amyloidosis with CAEL-101, an Anti-Amyloid
Monoclonal Antibody, Combined with Anti-Plasma Cell Dyscrasia
Abstract # 4550
Poster Session: 653. Myeloma and Plasma
Cell Dyscrasias: Prospective Therapeutic Trials: Poster III
December 12, 2022
18:00-20:00 CST
Location: Hall D (Ernest N. Morial
Convention Center)
AL Amyloidosis
Catini, J
Evaluation of the Path to Diagnosis and
Time to Treatment in Patients with Light-Chain Amyloidosis Using
the Komodo Claims Database
Abstract # 1887
Poster Session: 652. Multiple Myeloma and
Plasma Cell Dyscrasias: Clinical and Epidemiological: Poster I
December 10, 2022
17:30-19:30 CST
Location: Hall D (Ernest N. Morial
Convention Center)
HSCT-TMA
Jacobi, P
Complement Activation is Associated
with Endothelial Damage in
Hematopoietic Stem Cell Transplant
Associated-Thrombotic Microangiopathy
Abstract # 2431
Poster Session: 301. Vasculature,
Endothelium, Thrombosis and Platelets: Basic and Translational:
Poster II
December 11, 2022
18:00-20:00 CST
Location: Hall D (Ernest N. Morial
Convention Center)
aHUS
Gasteyger, C
Use of PLASMIC Scores to Aid Diagnosis of
aHUS: A Real-World Analysis of Hospitalized Patients from the
Premier Healthcare Database
Abstract # 1178
Poster Session: 331. Thrombotic
Microangiopathies/Thrombocytopenias and COVID-19-related
Thrombotic/Vascular Disorders: Clinical and Epidemiological: Poster
I
December 10, 2022
17:30-19:30 CST
Location: Hall D (Ernest N. Morial
Convention Center)
Siedlecki, A
Characterization of Patients with aHUS and
Triggering/Associated Events, with and without Complement
Pathogenic Variants or anti-CFH Antibodies: A Global aHUS Registry
Analysis
Abstract # 1173
Poster Session: 331. Thrombotic
Microangiopathies/Thrombocytopenias and COVID-19-related
Thrombotic/Vascular Disorders: Clinical and Epidemiological: Poster
I
December 10, 2022
17:30-19:30 CST
Location: Hall D (Ernest N. Morial
Convention Center)
INDICATION AND USAGE
CALQUENCE is a Bruton tyrosine kinase (BTK) inhibitor indicated
for the treatment of adult patients with mantle cell lymphoma (MCL)
who have received at least one prior therapy.
This indication is approved under accelerated approval based on
overall response rate. Continued approval for this indication may
be contingent upon verification and description of clinical benefit
in confirmatory trials.
CALQUENCE is also indicated for the treatment of adult patients
with chronic lymphocytic leukemia (CLL) or small lymphocytic
lymphoma (SLL).
IMPORTANT SAFETY INFORMATION ABOUT CALQUENCE® (acalabrutinib)
tablets
Serious and Opportunistic Infections
Fatal and serious infections, including opportunistic
infections, have occurred in patients with hematologic malignancies
treated with CALQUENCE.
Serious or Grade 3 or higher infections (bacterial, viral, or
fungal) occurred in 19% of 1029 patients exposed to CALQUENCE in
clinical trials, most often due to respiratory tract infections
(11% of all patients, including pneumonia in 6%). These infections
predominantly occurred in the absence of Grade 3 or 4 neutropenia,
with neutropenic infection reported in 1.9% of all patients.
Opportunistic infections in recipients of CALQUENCE have included,
but are not limited to, hepatitis B virus reactivation, fungal
pneumonia, Pneumocystis jiroveci pneumonia, Epstein-Barr virus
reactivation, cytomegalovirus, and progressive multifocal
leukoencephalopathy (PML). Consider prophylaxis in patients who are
at increased risk for opportunistic infections. Monitor patients
for signs and symptoms of infection and treat promptly.
Hemorrhage
Fatal and serious hemorrhagic events have occurred in patients
with hematologic malignancies treated with CALQUENCE. Major
hemorrhage (serious or Grade 3 or higher bleeding or any central
nervous system bleeding) occurred in 3.0% of patients, with fatal
hemorrhage occurring in 0.1% of 1029 patients exposed to CALQUENCE
in clinical trials. Bleeding events of any grade, excluding
bruising and petechiae, occurred in 22% of patients.
Use of antithrombotic agents concomitantly with CALQUENCE may
further increase the risk of hemorrhage. In clinical trials, major
hemorrhage occurred in 2.7% of patients taking CALQUENCE without
antithrombotic agents and 3.6% of patients taking CALQUENCE with
antithrombotic agents. Consider the risks and benefits of
antithrombotic agents when co-administered with CALQUENCE. Monitor
patients for signs of bleeding.
Consider the benefit-risk of withholding CALQUENCE for 3-7 days
pre- and post-surgery depending upon the type of surgery and the
risk of bleeding.
Cytopenias
Grade 3 or 4 cytopenias, including neutropenia (23%), anemia
(8%), thrombocytopenia (7%), and lymphopenia (7%), developed in
patients with hematologic malignancies treated with CALQUENCE.
Grade 4 neutropenia developed in 12% of patients. Monitor complete
blood counts regularly during treatment. Interrupt treatment,
reduce the dose, or discontinue treatment as warranted.
Second Primary Malignancies
Second primary malignancies, including skin cancers and other
solid tumors, occurred in 12% of 1029 patients exposed to CALQUENCE
in clinical trials. The most frequent second primary malignancy was
skin cancer, reported in 6% of patients. Monitor patients for skin
cancers and advise protection from sun exposure.
Atrial Fibrillation and Flutter
Grade 3 atrial fibrillation or flutter occurred in 1.1% of 1029
patients treated with CALQUENCE, with all grades of atrial
fibrillation or flutter reported in 4.1% of all patients. The risk
may be increased in patients with cardiac risk factors,
hypertension, previous arrhythmias, and acute infection. Monitor
for symptoms of arrhythmia (eg, palpitations, dizziness, syncope,
dyspnea) and manage as appropriate.
ADVERSE REACTIONS
The most common adverse reactions (≥20%) of any grade in
patients with relapsed or refractory MCL were anemia,*
thrombocytopenia,* headache (39%), neutropenia,* diarrhea (31%),
fatigue (28%), myalgia (21%), and bruising (21%). The most common
Grade ≥3 non-hematological adverse reaction (reported in at least
2% of patients) was diarrhea (3.2%).
*Treatment-emergent decreases (all grades) of hemoglobin (46%),
platelets (44%), and neutrophils (36%) were based on laboratory
measurements and adverse reactions.
Dose reductions or discontinuations due to any adverse reaction
were reported in 1.6% and 6.5% of patients, respectively. Increases
in creatinine to 1.5 to 3 times the upper limit of normal (ULN)
occurred in 4.8% of patients.
The most common adverse reactions (≥30%) of any grade in
patients with CLL were anemia,* neutropenia,* thrombocytopenia,*
headache, upper respiratory tract infection, and diarrhea.
*Treatment-emergent decreases (all grades) of hemoglobin,
platelets, and neutrophils were based on laboratory measurements
and adverse reactions.
In patients with previously untreated CLL exposed to CALQUENCE,
fatal adverse reactions that occurred in the absence of disease
progression and with onset within 30 days of the last study
treatment were reported in 2% for each treatment arm, most often
from infection. Serious adverse reactions were reported in 39% of
patients in the CALQUENCE plus obinutuzumab arm and 32% in the
CALQUENCE monotherapy arm, most often due to events of pneumonia
(7% and 2.8%, respectively).
Adverse reactions led to CALQUENCE dose reduction in 7% and 4%
of patients in the CALQUENCE plus obinutuzumab arm (N=178) and
CALQUENCE monotherapy arm (N=179), respectively. Adverse events led
to discontinuation in 11% and 10% of patients, respectively.
Increases in creatinine to 1.5 to 3 times ULN occurred in 3.9% and
2.8% of patients in the CALQUENCE combination arm and monotherapy
arm, respectively.
In patients with relapsed/refractory CLL exposed to CALQUENCE,
serious adverse reactions occurred in 29% of patients. Serious
adverse reactions in >5% of patients who received CALQUENCE
included lower respiratory tract infection (6%). Fatal adverse
reactions within 30 days of the last dose of CALQUENCE occurred in
2.6% of patients, including from second primary malignancies and
infection.
Adverse reactions led to CALQUENCE dose reduction in 3.9% of
patients (N=154), dose interruptions in 34% of patients, most often
due to respiratory tract infections followed by neutropenia, and
discontinuation in 10% of patients, most frequently due to second
primary malignancies followed by infection. Increases in creatinine
to 1.5 to 3 times ULN occurred in 1.3% of patients who received
CALQUENCE.
DRUG INTERACTIONS
Strong CYP3A Inhibitors: Avoid co-administration of
CALQUENCE with a strong CYP3A inhibitor. If these inhibitors will
be used short-term, interrupt CALQUENCE. After discontinuation of
strong CYP3A inhibitor for at least 24 hours, resume previous
dosage of CALQUENCE.
Moderate CYP3A Inhibitors: Reduce the dosage of CALQUENCE
to 100 mg once daily when co-administered with a moderate CYP3A
inhibitor.
Strong CYP3A Inducers: Avoid co-administration of
CALQUENCE with a strong CYP3A inducer. If co-administration is
unavoidable, increase the dosage of CALQUENCE to 200 mg
approximately every 12 hours.
SPECIFIC POPULATIONS
Based on findings in animals, CALQUENCE may cause fetal harm and
dystocia when administered to a pregnant woman. There are no
available data in pregnant women to inform the drug-associated
risk. Advise pregnant women of the potential risk to a fetus.
Pregnancy testing is recommended for females of reproductive
potential prior to initiating CALQUENCE therapy. Advise female
patients of reproductive potential to use effective contraception
during treatment with CALQUENCE and for 1 week following the last
dose of CALQUENCE.
It is not known if CALQUENCE is present in human milk. Advise
lactating women not to breastfeed while taking CALQUENCE and for 2
weeks after the last dose.
Avoid use of CALQUENCE in patients with severe hepatic
impairment (Child-Pugh class C). No dosage adjustment of CALQUENCE
is recommended in patients with mild (Child-Pugh class A) or
moderate (Child-Pugh class B) hepatic impairment.
Please see full Prescribing Information,
including Patient Information.
INDICATION(S) & IMPORTANT SAFETY INFORMATION for
ULTOMIRIS
INDICATION(S)
Paroxysmal Nocturnal Hemoglobinuria (PNH)
ULTOMIRIS is indicated for the treatment of adult and pediatric
patients one month of age and older with paroxysmal nocturnal
hemoglobinuria (PNH).
Atypical Hemolytic Uremic Syndrome (aHUS)
ULTOMIRIS is indicated for the treatment of adult and pediatric
patients one month of age and older with atypical hemolytic uremic
syndrome (aHUS) to inhibit complement-mediated thrombotic
microangiopathy (TMA).
Limitation of Use:
ULTOMIRIS is not indicated for the treatment of patients with
Shiga toxin E. coli related hemolytic uremic syndrome
(STEC-HUS).
Subcutaneous Use in Adult Patients with PNH or aHUS
Subcutaneous administration of ULTOMIRIS is not approved for use
in pediatric patients.
IMPORTANT SAFETY INFORMATION
WARNING: SERIOUS MENINGOCOCCAL
INFECTIONS
Life-threatening meningococcal
infections/sepsis have occurred in patients treated with ULTOMIRIS.
Meningococcal infection may become rapidly life-threatening or
fatal if not recognized and treated early.
- Comply with the most current Advisory Committee on
Immunization Practices (ACIP) recommendations for meningococcal
vaccination in patients with complement deficiencies.
- Immunize patients with meningococcal vaccines at least 2
weeks prior to administering the first dose of ULTOMIRIS, unless
the risks of delaying ULTOMIRIS therapy outweigh the risk of
developing a meningococcal infection. See Warnings and Precautions
for additional guidance on the management of the risk of
meningococcal infection.
- Vaccination reduces, but does not eliminate, the risk of
meningococcal infections. Monitor patients for early signs of
meningococcal infections and evaluate immediately if infection is
suspected.
Because of the risk of serious
meningococcal infections, ULTOMIRIS is available only through a
restricted program under a Risk Evaluation and Mitigation Strategy
(REMS) called ULTOMIRIS REMS.
CONTRAINDICATIONS
- Patients with unresolved Neisseria meningitidis infection.
- Patients who are not currently vaccinated against Neisseria
meningitidis, unless the risks of delaying ULTOMIRIS treatment
outweigh the risks of developing a meningococcal infection.
WARNINGS AND PRECAUTIONS
Serious Meningococcal Infections
Life-threatening meningococcal infections have occurred in
patients treated with ULTOMIRIS. The use of ULTOMIRIS increases a
patient’s susceptibility to serious meningococcal infections
(septicemia and/or meningitis). Meningococcal disease due to any
serogroup may occur.
Vaccinate or revaccinate for meningococcal disease according to
the most current ACIP recommendations for patients with complement
deficiencies. Immunize patients without history of meningococcal
vaccination at least 2 weeks prior to the first dose of ULTOMIRIS.
Patients who initiate ULTOMIRIS treatment less than 2 weeks after
receiving meningococcal vaccine(s) must receive appropriate
prophylactic antibiotics until 2 weeks after vaccination.
In clinical studies, 59 adult patients with PNH and 2 adult
patients with gMG were treated with ULTOMIRIS less than 2 weeks
after meningococcal vaccination. All of these patients received
antibiotics for prophylaxis of meningococcal infection until at
least 2 weeks after meningococcal vaccination. The benefits and
risks of antibiotic prophylaxis for prevention of meningococcal
infections in patients receiving ULTOMIRIS have not been
established. In clinical studies with ULTOMIRIS, <1% of patients
developed serious meningococcal infections/sepsis while receiving
treatment with ULTOMIRIS. All were adult patients with PNH who had
been vaccinated. These patients recovered while continuing
treatment with ULTOMIRIS. Consider discontinuation of ULTOMIRIS in
patients who are undergoing treatment for serious meningococcal
infection.
ULTOMIRIS REMS
Due to the risk of meningococcal infections, ULTOMIRIS is
available only through a restricted program under a REMS called
ULTOMIRIS REMS.
Under the ULTOMIRIS REMS, prescribers must enroll in the
program. Prescribers must counsel patients about the risk of
meningococcal infection/sepsis, provide the patients with the REMS
educational materials, and ensure patients are vaccinated with
meningococcal vaccines.
Additional information on the REMS requirements is available at
www.ultomirisrems.com or 1-888-765-4747.
Other Infections
Patients may have increased susceptibility to infections,
especially with encapsulated bacteria, such as infections caused by
Neisseria meningitidis but also Streptococcus pneumoniae,
Haemophilus influenzae, and to a lesser extent, Neisseria
gonorrhoeae. Children treated with ULTOMIRIS may be at increased
risk of developing serious infections due to Streptococcus
pneumoniae and Haemophilus influenzae type b (Hib). Administer
vaccinations for the prevention of Streptococcus pneumoniae and
Haemophilus influenzae type b (Hib) infections according to ACIP
guidelines. If ULTOMIRIS is administered to patients with active
systemic infections, monitor closely for worsening infection.
Monitoring Disease Manifestations after ULTOMIRIS
Discontinuation
Treatment Discontinuation for
PNH
After discontinuing treatment with ULTOMIRIS, closely monitor
for signs and symptoms of hemolysis, identified by elevated LDH
along with sudden decrease in PNH clone size or hemoglobin, or
re-appearance of symptoms such as fatigue, hemoglobinuria,
abdominal pain, shortness of breath (dyspnea), major adverse
vascular event (including thrombosis), dysphagia, or erectile
dysfunction. Monitor any patient who discontinues ULTOMIRIS for at
least 16 weeks to detect hemolysis and other reactions. If signs
and symptoms of hemolysis occur after discontinuation, including
elevated LDH, consider restarting treatment with ULTOMIRIS.
Treatment Discontinuation for
aHUS
ULTOMIRIS treatment of aHUS should be a minimum duration of 6
months. Due to heterogeneous nature of aHUS events and
patient-specific risk factors, treatment duration beyond the
initial 6 months should be individualized. There are no specific
data on ULTOMIRIS discontinuation. After discontinuing treatment
with ULTOMIRIS, patients should be monitored for clinical symptoms
and laboratory signs of TMA complications for at least 12
months.
TMA complications post-discontinuation can be identified if any
of the following is observed: Clinical symptoms of TMA include
changes in mental status, seizures, angina, dyspnea, thrombosis or
increasing blood pressure. In addition, at least two of the
following laboratory signs observed concurrently and results should
be confirmed by a second measurement 28 days apart with no
interruption: a decrease in platelet count of 25% or more as
compared to either baseline or to peak platelet count during
ULTOMIRIS treatment; an increase in serum creatinine of 25% or more
as compared to baseline or to nadir during ULTOMIRIS treatment; or,
an increase in serum LDH of 25% or more as compared to baseline or
to nadir during ULTOMIRIS treatment. If TMA complications occur
after discontinuation, consider reinitiation of ULTOMIRIS treatment
or appropriate organ-specific supportive measures.
Thromboembolic Event Management
The effect of withdrawal of anticoagulant therapy during
treatment with ULTOMIRIS has not been established. Treatment should
not alter anticoagulant management.
Infusion-Related Reactions
Intravenous or subcutaneous administration of ULTOMIRIS may
result in systemic infusion-related reactions, including
anaphylaxis and hypersensitivity reactions. In clinical trials,
infusion-related reactions occurred in approximately 1% of patients
treated with ULTOMIRIS. These events included lower back pain, drop
in blood pressure, elevation in blood pressure, limb discomfort,
drug hypersensitivity (allergic reaction), dysgeusia (bad taste),
and drowsiness. These reactions did not require discontinuation of
ULTOMIRIS. If signs of cardiovascular instability or respiratory
compromise occur, interrupt ULTOMIRIS infusion and institute
appropriate supportive measures.
Injection Site Reactions- Subcutaneous administration
27% (23/84) of patients treated with subcutaneous administration
of ULTOMIRIS experienced injection site reactions which included
application site rash, device allergy, infusion site pain, infusion
site reaction, injection site bruising, injection site erythema,
injection site hematoma, injection site induration, injection site
inflammation, injection site pain, injection site pruritus,
injection site rash, injection site reaction, injection site
swelling, injection site urticaria, medical device site bruise,
medical device site erythema, medical device site hematoma, medical
device site induration, medical device site pruritus, medical
device site rash, and medical device site reaction.
Allergies to Acrylic Adhesives
The on-body injector of ULTOMIRIS uses acrylic adhesive. For
patients with a known allergy to acrylic adhesive, use of this
product may result in an allergic reaction. Premedication can be
considered, and supportive measures should be instituted if signs
of allergy appear.
ADVERSE REACTIONS
Adverse Reactions for PNH
Adverse reactions reported in 5% or more of patients treated
with ULTOMIRIS vs. Eculizumab was Upper respiratory tract infection
(39% vs. 39%), Headache (32% vs. 26%), Diarrhea (9% vs. 5%), Nausea
(9% vs. 9%), Pyrexia (7% vs. 8%), Pain in extremity (6% vs. 5%),
Abdominal pain (6% vs. 7%), Dizziness (5% vs. 6%), Arthralgia (5%
vs. 5%). Serious adverse reactions were reported in 15 (6.8%)
patients receiving ULTOMIRIS. The serious adverse reactions in
patients treated with ULTOMIRIS included hyperthermia and pyrexia.
No serious adverse reaction was reported in more than 1 patient
treated with ULTOMIRIS. One fatal case of sepsis was identified in
a patient treated with ULTOMIRIS. In clinical studies, clinically
relevant adverse reactions in 1% of adult patients include
infusion-related reactions.
Adverse reactions reported in 10% or more of pediatric patients
treated with ULTOMIRIS who were treatment-naïve vs.
Eculizumab-experienced was Anemia (20% vs. 25%), Abdominal pain (0%
vs. 38%), Constipation (0% vs. 25%), Pyrexia (20% vs. 13%), Upper
respiratory tract infection (20% vs. 75%), Pain in extremity (0%
vs. 25%), Headache (20% vs. 25%).
Adverse Reactions for aHUS
Most common adverse reactions in patients with aHUS (incidence
≥20%) were upper respiratory tract infection, diarrhea, nausea,
vomiting, headache, hypertension and pyrexia. Serious adverse
reactions were reported in 42 (57%) patients with aHUS receiving
ULTOMIRIS. The most frequent serious adverse reactions reported in
more than 2 patients (2.7%) treated with ULTOMIRIS were
hypertension, pneumonia and abdominal pain. In clinical studies,
clinically relevant adverse reactions in <10% of patients
include viral tonsillitis in adults and viral infection in
pediatric patients and in 3% of adult patients include
infusion-related reactions.
Adverse Reactions for Subcutaneous
Administration of ULTOMIRIS
Most common adverse reactions (≥10%) with ULTOMIRIS subcutaneous
administration via On Body Injector in adult patients with PNH were
local injection site reactions, diarrhea, and headache.
DRUG INTERACTIONS
Plasma Exchange, Plasmapheresis, and
Intravenous Immunoglobulins
Concomitant use of ULTOMIRIS with plasma exchange (PE),
plasmapheresis (PP), or intravenous immunoglobulin (IVIg) treatment
can reduce serum ravulizumab concentrations and requires a
supplemental dose of ULTOMIRIS.
Neonatal Fc Receptor Blockers
Concomitant use of ULTOMIRIS with neonatal Fc receptor (FcRn)
blockers (e.g., efgartigimod) may lower systemic exposures and
reduce effectiveness of ULTOMIRIS. Closely monitor for reduced
effectiveness of ULTOMIRIS.
Please see accompanying full Prescribing
Information for ULTOMIRIS, including Boxed WARNING regarding
serious and life-threatening meningococcal
infections/sepsis.
INDICATIONS & IMPORTANT SAFETY INFORMATION FOR SOLIRIS®
(eculizumab)
INDICATIONS
Paroxysmal Nocturnal Hemoglobinuria (PNH)
Soliris is indicated for the treatment of patients with
paroxysmal nocturnal hemoglobinuria (PNH) to reduce hemolysis.
Atypical Hemolytic Uremic Syndrome (aHUS)
Soliris is indicated for the treatment of patients with atypical
hemolytic uremic syndrome (aHUS) to inhibit complement-mediated
thrombotic microangiopathy.
Limitation of Use
Soliris is not indicated for the treatment of patients with
Shiga toxin E. coli related hemolytic uremic syndrome
(STEC-HUS).
IMPORTANT SAFETY INFORMATION
WARNING: SERIOUS MENINGOCOCCAL
INFECTIONS Life-threatening and fatal meningococcal
infections have occurred in patients treated with Soliris and may
become rapidly life-threatening or fatal if not recognized and
treated early.
- Comply with the most current Advisory Committee on
Immunization Practices (ACIP) recommendations for meningococcal
vaccination in patients with complement deficiencies.
- Immunize patients with meningococcal vaccines at least 2
weeks prior to administering the first dose of Soliris, unless the
risks of delaying Soliris therapy outweigh the risk of developing a
meningococcal infection. (See Serious Meningococcal Infections for
additional guidance on the management of the risk of meningococcal
infection).
- Vaccination reduces, but does not eliminate, the risk of
meningococcal infections. Monitor patients for early signs of
meningococcal infections and evaluate immediately if infection is
suspected.
Soliris is available only through a restricted program under
a Risk Evaluation and Mitigation Strategy (REMS). Under the Soliris
REMS, prescribers must enroll in the program. Enrollment in the
Soliris REMS program and additional information are available by
telephone: 1-888-SOLIRIS (1-888-765-4747) or at
www.solirisrems.com.
Contraindications
- Patients with unresolved serious Neisseria meningitidis
infection
- Patients who are not currently vaccinated against Neisseria
meningitidis, unless the risks of delaying Soliris treatment
outweigh the risks of developing a meningococcal infection
Warnings and Precautions
Serious Meningococcal Infections
Risk and Prevention
The use of Soliris increases a patient's susceptibility to
serious meningococcal infections (septicemia and/or
meningitis).
Vaccinate or revaccinate for meningococcal disease according to
the most current ACIP recommendations for patients with complement
deficiencies. Immunize patients without a history of meningococcal
vaccination at least 2 weeks prior to receiving the first dose of
Soliris. If Soliris must be initiated immediately in an
unvaccinated patient, administer meningococcal vaccine(s) as soon
as possible and provide 2 weeks of antibacterial drug prophylaxis.
Discontinue Soliris in patients who are undergoing treatment for
serious meningococcal infections.
REMS
Prescribers must counsel patients about the risk of
meningococcal infection, provide the patients with the REMS
educational materials, and ensure patients are vaccinated with
meningococcal vaccine(s).
Other Infections
Serious infections with Neisseria species (other than N.
meningitidis), including disseminated gonococcal infections, have
been reported.
Patients may have increased susceptibility to infections,
especially with encapsulated bacteria. Additionally, Aspergillus
infections have occurred in immunocompromised and neutropenic
patients. Children treated with Soliris may be at increased risk of
developing serious infections due to Streptococcus pneumoniae and
Haemophilus influenzae type b (Hib). Administer vaccinations for
the prevention of Streptococcus pneumoniae and Haemophilus
influenzae type b (Hib) infections according to ACIP guidelines.
Use caution when administering Soliris to patients with any
systemic infection.
Monitoring Disease Manifestations After Soliris
Discontinuation
Treatment Discontinuation for
PNH
Monitor patients after discontinuing Soliris for at least 8
weeks to detect hemolysis.
Treatment Discontinuation for
aHUS
After discontinuing Soliris, monitor patients with aHUS for
signs and symptoms of thrombotic microangiopathy (TMA)
complications for at least 12 weeks. In aHUS clinical trials, 18
patients (5 in the prospective studies) discontinued Soliris
treatment. TMA complications occurred following a missed dose in 5
patients, and Soliris was reinitiated in 4 of these 5 patients.
Clinical signs and symptoms of TMA include changes in mental
status, seizures, angina, dyspnea, or thrombosis. In addition, the
following changes in laboratory parameters may identify a TMA
complication: occurrence of 2, or repeated measurement of any one
of the following: a decrease in platelet count by 25% or more
compared to baseline or the peak platelet count during Soliris
treatment; an increase in serum creatinine by 25% or more compared
to baseline or nadir during Soliris treatment; or, an increase in
serum LDH by 25% or more over baseline or nadir during Soliris
treatment.
If TMA complications occur after Soliris discontinuation,
consider reinstitution of Soliris treatment, plasma therapy
[plasmapheresis, plasma exchange, or fresh frozen plasma infusion
(PE/PI)], or appropriate organ-specific supportive measures.
Thrombosis Prevention and Management
The effect of withdrawal of anticoagulant therapy during Soliris
treatment has not been established. Therefore, treatment with
Soliris should not alter anticoagulant management.
Infusion-Related Reactions
Administration of Soliris may result in infusion-related
reactions, including anaphylaxis or other hypersensitivity
reactions. Interrupt Soliris infusion and institute appropriate
supportive measures if signs of cardiovascular instability or
respiratory compromise occur.
Adverse Reactions
The most frequently reported adverse reactions in the PNH
randomized trial (≥10% overall and greater than placebo) are:
headache, nasopharyngitis, back pain, and nausea.
The most frequently reported adverse reactions in aHUS single
arm prospective trials (≥20%) are: headache, diarrhea,
hypertension, upper respiratory infection, abdominal pain,
vomiting, nasopharyngitis, anemia, cough, peripheral edema, nausea,
urinary tract infections, pyrexia.
Please see accompanying full prescribing
information for Soliris, including Boxed WARNING regarding
serious meningococcal infections.
Notes
CALQUENCE
CALQUENCE (acalabrutinib) is a next-generation, selective
inhibitor of Bruton’s tyrosine kinase (BTK). CALQUENCE binds
covalently to BTK, thereby inhibiting its activity.18,19 In B
cells, BTK signaling results in activation of pathways necessary
for B-cell proliferation, trafficking, chemotaxis and
adhesion.18
CALQUENCE is available for prescribing in capsule and tablet
formulations in the US. CALQUENCE tablets and capsules are approved
in the US for the treatment of CLL and SLL, and for the treatment
of adult patients with MCL who have received at least one prior
therapy.18,20 Capsules have restrictions in relation to use with
gastric acid-reducing agents. The tablets are not licensed in the
European Union.
CALQUENCE capsules are approved for CLL in the EU and many other
countries worldwide and approved in Japan for relapsed or
refractory CLL and SLL. A Phase I trial is currently underway in
Japan for the treatment of front-line CLL.
In the US and several other countries, CALQUENCE capsules are
also approved for the treatment of adult patients with MCL who have
received at least one prior therapy. The US MCL indication is
approved under accelerated approval based on overall response rate.
Continued approval for this indication may be contingent upon
verification and description of clinical benefit in confirmatory
trials. CALQUENCE is not currently approved for the treatment of
MCL in Europe or Japan.
As part of an extensive clinical development program,
AstraZeneca and Acerta Pharma are currently evaluating CALQUENCE in
more than 20 company-sponsored clinical trials. CALQUENCE is being
evaluated for the treatment of multiple B-cell blood cancers,
including CLL, MCL, diffuse large B-cell lymphoma, Waldenstr�m’s
macroglobulinemia, follicular lymphoma and marginal zone
lymphoma.
ULTOMIRIS
ULTOMIRIS (ravulizumab-cwvz), the first and only long-acting C5
complement inhibitor, provides immediate, complete and sustained
complement inhibition. The medication works by inhibiting the C5
protein in the terminal complement cascade, a part of the body’s
immune system. When activated in an uncontrolled manner, the
complement cascade over-responds, leading the body to attack its
own healthy cells. ULTOMIRIS is administered intravenously every
eight weeks in adult patients, following a loading dose.
ULTOMIRIS is approved in the US, EU and Japan for the treatment
of certain adults with gMG.
ULTOMIRIS is also approved in the US, EU and Japan for the
treatment of certain adults with PNH and for certain children with
PNH in the US and EU.
Additionally, ULTOMIRIS is approved in the US, EU and Japan for
certain adults and children with aHUS to inhibit
complement-mediated thrombotic microangiopathy.
As part of a broad development program, ULTOMIRIS is being
assessed for the treatment of additional hematology and neurology
indications.
SOLIRIS
SOLIRIS (eculizumab) is a first-in-class C5 complement
inhibitor. The medication works by inhibiting the C5 protein in the
terminal complement cascade, a part of the body’s immune system.
When activated in an uncontrolled manner, the terminal complement
cascade over-responds, leading the body to attack its own healthy
cells. SOLIRIS is administered intravenously every two weeks,
following an introductory dosing period.
SOLIRIS is approved in the US, EU and Japan for the treatment of
PNH, aHUS, certain adults with gMG and certain adults with
NMOSD.
SOLIRIS is not indicated for the treatment of patients with
STEC-HUS.
AstraZeneca in hematology
AstraZeneca is pushing the boundaries of science to redefine
care in hematology. We have expanded our commitment to patients
with hematologic conditions, not only in oncology but also in rare
diseases with the acquisition of Alexion, allowing us to reach more
patients with high unmet needs. By applying our deep understanding
of blood cancers, leveraging our strength in solid tumor oncology
and delivering on Alexion’s pioneering legacy in complement science
to provide innovative medicines for rare diseases, we are pursuing
the end-to-end development of novel therapies designed to target
underlying drivers of disease.
By targeting hematologic conditions with high unmet medical
needs, we aim to deliver innovative medicines and approaches to
improve patient outcomes. Our goal is to help transform the lives
of patients living with malignant, rare and other related
hematologic diseases, shaped by insights from patients, caregivers
and physicians to have the most meaningful impact.
AstraZeneca in oncology
AstraZeneca is leading a revolution in oncology with the
ambition to provide cures for cancer in every form, following the
science to understand cancer and all its complexities to discover,
develop and deliver life-changing medicines to patients.
The Company’s focus is on some of the most challenging cancers.
It is through persistent innovation that AstraZeneca has built one
of the most diverse portfolios and pipelines in the industry, with
the potential to catalyze changes in the practice of medicine and
transform the patient experience.
AstraZeneca has the vision to redefine cancer care and, one day,
eliminate cancer as a cause of death.
About Alexion, AstraZeneca Rare Disease
Alexion, AstraZeneca Rare Disease, is the group within
AstraZeneca focused on rare diseases, created following the 2021
acquisition of Alexion Pharmaceuticals, Inc. As a leader in rare
diseases for 30 years, Alexion is focused on serving patients and
families affected by rare diseases and devastating conditions
through the discovery, development and commercialization of
life-changing medicines. Alexion focuses its research efforts on
novel molecules and targets in the complement cascade and its
development efforts on hematology, nephrology, neurology, metabolic
disorders, cardiology and ophthalmology. Headquartered in Boston,
Massachusetts, Alexion has offices around the globe and serves
patients in more than 50 countries.
About AstraZeneca
AstraZeneca is a global, science-led biopharmaceutical company
that focuses on the discovery, development and commercialization of
prescription medicines in Oncology, Rare Diseases and
BioPharmaceuticals, including Cardiovascular, Renal &
Metabolism, and Respiratory & Immunology. Based in Cambridge,
UK, AstraZeneca operates in over 100 countries, and its innovative
medicines are used by millions of patients worldwide. For more
information, please visit www.astrazeneca-us.com and follow us on
Twitter @AstraZenecaUS.
References
- Seymour JF, Byrd JC, Munir T, et al. Assessing the Burden of
Adverse Events in a Head-to-Head Trial of Acalabrutinib Versus
Ibrutinib in Previously Treated Chronic Lymphocytic Leukemia (CLL)
[abstract and poster]. Presented at: American Society of Hematology
(ASH) Congress; December 10-13, 2022; New Orleans, LA. Abs
3133.
- Byrd JC, Woyach JA, Furman RR, et al. Final Results of the
Phase 1/2 Study of Acalabrutinib Monotherapy in Treatment-Naive
Chronic Lymphocytic Leukemia with >6 Years of Follow-up
[abstract and poster]. Presented at: American Society of Hematology
(ASH) Congress; December 10-13, 2022; New Orleans, LA. Abs
4431.
- Furman RR, Wierda WG, Schuh A, et al. Phase 1/2 Study of
Acalabrutinib Monotherapy in Patients with Relapsed/Refractory
Chronic Lymphocytic Leukemia: Final Results with >4 Years of
Follow-up [abstract and poster]. Presented at: American Society of
Hematology (ASH) Congress; December 10-13, 2022; New Orleans, LA.
Abs 4434.
- Ryan CE, Lampson BL, Tyekucheva, S, et al. Updated Results from
a Multicenter, Phase 2 Study of Acalabrutinib, Venetoclax,
Obinutuzumab (AVO) in a Population of Previously Untreated Patients
with CLL Enriched for High-Risk Disease [abstract and oral].
Presented at: American Society of Hematology (ASH) Congress;
December 10-13, 2022; New Orleans, LA. Abs 344.
- Davids MS, Sharman JP, Eyre TA, et al. Contribution of
Obinutuzumab to Acalabrutinib Therapy in Patients with
Treatment-Naive Chronic Lymphocytic Leukemia: Analysis of Survival
Outcomes by Genomic Features [abstract and poster]. Presented at:
American Society of Hematology (ASH) Congress; December 10-13,
2022; New Orleans, LA. Abs 1815.
- Ruan J, Leonard JP, Chen GZ, et al. Phase 2 Trial of
Acalabrutinib-Lenalidomide-Rituximab (ALR) with Real-Time
Monitoring of MRD in Patients with Treatment-Naïve Mantle Cell
Lymphoma [abstract and oral]. Presented at: American Society of
Hematology (ASH) Congress; December 10-13, 2022; New Orleans, LA.
Abs 73.
- Hou JZ, Jacobs R, Cho SG, et al. Interim Results of the Phase 1
Study of Tnb-486, a Novel CD19xCD3 T-Cell Engager, in Patients with
Relapsed/Refractory (R/R) B-NHL [abstract and oral]. Presented at:
American Society of Hematology (ASH) Congress; December 10-13,
2022; New Orleans, LA. Abs 612.
- Brümmendorf T, Medd P, Koch R, et al. Safety, Tolerability,
Pharmacokinetics (PK) and Preliminary Antitumor Activity of the
Cyclin-Dependent Kinase-9 (CDK9) Inhibitor AZD4573 in
Relapsed/Refractory Hematological Malignancies: A Phase 1
First-in-Human Study [abstract and poster]. Presented at: American
Society of Hematology (ASH) Congress; December 10-13, 2022; New
Orleans, LA. Abs 1353.
- Strati P, Kim TM, Danilov A, et al. Phase 1b/2a Study of
AZD4573 (CDK9i) and Acalabrutinib in Patients with
Relapsed/Refractory Diffuse Large B-Cell Lymphoma (r/r DLBCL):
Results from Dose-Escalation [abstract and poster]. Presented at:
American Society of Hematology (ASH) Congress; December 10-13,
2022; New Orleans, LA. Abs 2962.
- Arslan S, Fleming S, Jain N, et al. Safety and Tolerability of
AZD0466 as Monotherapy for Patients with Advanced Hematological
Malignancies. Preliminary Results from an Ongoing Phase I/II Trial
[abstract and poster]. Presented at: American Society of Hematology
(ASH) Congress; December 10-13, 2022; New Orleans, LA. Abs
4094.
- Browett P, Kulasekararaj A, Notaro R, et al. Vemircopan
(ALXN2050) Monotherapy in Paroxysmal Nocturnal Hemoglobinuria:
Interim Data from a Phase 2 Open-Label Proof-of-Concept Study
[abstract and oral]. Presented at: American Society of Hematology
(ASH) Congress; December 10-13, 2022; New Orleans, LA. Abs
294.
- Griffin M, Gandhi S, Hicks E, et al. Terminal Complement
Inhibition and Control of Hemolysis in Paroxysmal Nocturnal
Hemoglobinuria Following Switching from High-Dose Eculizumab to
Ravulizumab: An Interim Analysis [abstract and poster]. Presented
at: American Society of Hematology (ASH) Congress; December 10-13,
2022; New Orleans, LA. Abs 1251.
- Siedlecki A, Al-Dakkak I, Anokhina K, et al. Characterization
of Patients with aHUS and Triggering/Associated Events, with and
without Complement Pathogenic Variants or Anti-CFH Antibodies: A
Global aHUS Registry Analysis [abstract and poster]. Presented at:
American Society of Hematology (ASH) Congress; December 10-13,
2022; New Orleans, LA. Abs 1173.
- Gasteyger C, Uriol-Rivera M, Ávila A, et al. Use of PLASMIC
Scores to Aid Diagnosis of aHUS: A Real-World Analysis of
Hospitalized Patients from the Premier Healthcare Database
[abstract and poster]. Presented at: American Society of Hematology
(ASH) Congress; December 10-13, 2022; New Orleans, LA. Abs
1178.
- Jacobi P, Cofiell R, Chang CH, et. al. Complement Activation is
Associated with Endothelial Damage in Hematopoietic Stem Cell
Transplant Associated-Thrombotic Microangiopathy [abstract and
poster]. Presented at: American Society of Hematology (ASH)
Congress; December 10-13, 2022; New Orleans, LA. Abs 2431.
- Valent J, Liedtke M, Zonder J, et al. 1-Year Results from a
Phase 2 Study to Determine Safety and Tolerability of Treating
Patients with Light-Chain (AL) Amyloidosis with CAEL-101, an
Anti-Amyloid Monoclonal Antibody, Combined with Anti-Plasma Cell
Dyscrasia [abstract and poster]. Presented at: American Society of
Hematology (ASH) Congress; December 10-13, 2022; New Orleans, LA.
Abs 4550.
- Catini J, Doan Q, Evans J, et al. Evaluation of the Path to
Diagnosis and Time to Treatment in Patients with Light-Chain
Amyloidosis Using the Komodo Claims Database [abstract and poster].
Presented at: American Society of Hematology (ASH) Congress;
December 10-13, 2022; New Orleans, LA. Abs 1887.
- CALQUENCE® (acalabrutinib) capsules [prescribing information].
Wilmington, DE; AstraZeneca Pharmaceuticals LP; 2019.
- Wu J, Zhang M, Liu D. Acalabrutinib (ACP-196): a selective
second-generation BTK inhibitor. J Hematol Oncol. 2016;9(21).
- CALQUENCE® (acalabrutinib) tablets [prescribing information].
Wilmington, DE; AstraZeneca Pharmaceuticals LP; 2022.
View source
version on businesswire.com: https://www.businesswire.com/news/home/20221130005401/en/
Media Inquiries Brendan McEvoy, +1 302 885 2677 Miranda
Kulp, +1 302 885 2677
US Media Mailbox: usmediateam@astrazeneca.com
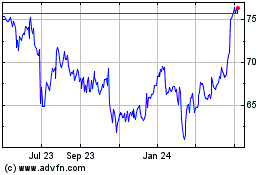
AstraZeneca (NASDAQ:AZN)
Historical Stock Chart
From Mar 2024 to Apr 2024
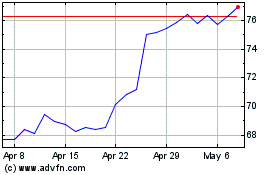
AstraZeneca (NASDAQ:AZN)
Historical Stock Chart
From Apr 2023 to Apr 2024