Centene Corporation (NYSE: CNC) today announced its net earnings
from continuing operations for the quarter ended September 30, 2009
were $22.7 million, or $0.51 per diluted share, compared to $18.1
million, or $0.41 per diluted share in the third quarter of 2008.
The results of operations for our New Jersey health plan,
University Health Plans, are classified as discontinued operations.
The discussions below, with the exception of cash flow information,
are in the context of continuing operations and all financial
ratios are calculated using revenues excluding premium taxes and
investment income.
Third Quarter Highlights
- Quarter-end managed care at-risk
membership of 1,386,400, an increase of 215,300 lives year over
year.
- Premium and Service revenues of
$987.3 million, representing 18.1% year over year growth.
- Health Benefits Ratio (HBR) of
83.7%.
- General and Administrative
(G&A) expense ratio of 13.2%.
- Cash flow from operations of
$114.9 million.
- Days in claims payable of
47.1.
- Diluted earnings per share from
continuing operations of $0.51, compared to $0.41 in the third
quarter of 2008. Earnings per diluted share in 2008 included a
$0.06 loss on investments from the Primary Reserve fund.
Other Events
- On August 31, 2009, Centene
announced that the State of Massachusetts had accepted its proposal
to manage healthcare services for the Commonwealth Bridge Program
through its subsidiary, CeltiCare Health Plan of Massachusetts,
effective October 1, 2009, through June 30, 2010.
- Effective September 1, 2009,
Centene converted 62,100 members in Florida from Access Health
Solutions to at-risk under our Sunshine State Health Plan.
- On October 24, 2009, Centene
announced a settlement agreement with Amerigroup Corporation
associated with the sale of our New Jersey health plan. Pursuant to
the settlement agreement, the parties will move forward with the
transaction, which is subject to regulatory approval and expected
to be completed in the first quarter of 2010.
- In August 2009, Jason Harrold,
president and CEO of OptiCare Managed Vision, Inc. was appointed to
Senior Vice President of Centene’s Specialty Business Unit. Mr.
Harrold assumed the leadership role over the specialty companies
previously held by William Scheffel.
- On October 26, 2009 our Board of
Directors approved an extension of our stock repurchase
program.
Michael F. Neidorff, Centene’s Chairman and Chief Executive
Officer, stated, “We are pleased with the ability of our team to
deliver solid results across Centene's products and markets in a
challenging economic environment.”
The following table depicts membership in Centene’s managed care
organizations, by state, at September 30, 2009 and 2008:
September 30, 2009 2008 Arizona
17,400 — Florida 84,400 — Georgia 303,400 283,900 Indiana 200,700
172,400 Massachusetts 500 — Ohio 151,200 132,500 South Carolina
46,100 26,600 Texas 450,200 433,200 Wisconsin 132,500 122,500 Total
at-risk membership 1,386,400 1,171,100 Non-risk membership 63,200*
3,700 Total 1,449,600 1,174,800 ______________________________
* Increase mainly due to
consolidation of our Access Health Solutions LLC investment,
effective January 1, 2009.
The following table depicts membership in Centene’s managed care
organizations, by member category, at September 30, 2009 and
2008:
September 30, 2009 2008 Medicaid
1,040,500 850,500 CHIP & Foster Care 263,400 261,800 ABD &
Medicare 82,500 58,800 Total at-risk membership 1,386,400 1,171,100
Non-risk membership 63,200 3,700 Total 1,449,600 1,174,800
Statement of Operations
- For the third quarter of 2009,
Premium and Service Revenues increased 18.1% to $987.3 million from
$835.7 million in the third quarter of 2008. The increase was
primarily driven by premium rate increases and membership growth in
all states, including the commencement of our Arizona acute care
contract in October 2008, the consolidation of Access and
conversion of members to our at-risk plan in Florida.
- The consolidated HBR, which
reflects medical costs as a percent of premium revenues, was 83.7%.
A reconciliation of the change in HBR from the prior year same
period and from the immediately preceding quarter is presented
below:
Q3:2009 vs. Q3:2008 Q3:2009 vs. Q2:2009
Third Quarter 2008 82.2 % Second Quarter 2009 83.1 % Decrease in
Texas CHIP/Perinate rates 1.0 New markets reserved at higher rates
0.1 Impact of additional costs related to the flu 0.5 Impact of
additional costs related to the flu 0.3 Pass-through payments 0.1
Pass-through payments 0.1 Net change in other markets (0.1 ) Net
change in other markets 0.1 Third Quarter 2009 83.7 % Third
Quarter 2009 83.7 %
The increase in the third quarter of 2009
over the comparable period in 2008 was due to the March 1, 2009
rate decrease for our CHIP/Perinate product in Texas which brought
the HBR more in line with our normal range and the impact of
additional costs related to the flu. We also experienced
improvements in our ABD product, particularly in Ohio, which was
mostly offset by the impact of changes in rates and benefit
structures in other markets. Sequentially, the increase in the HBR
reflects the impact of additional costs related to the flu along
with the effect of reserving at higher rates for new markets and
receiving pass-through payments which increase the HBR ratio.
- Consolidated G&A expense as
a percent of premium and service revenues was 13.2% in the third
quarter of 2009, a decrease from 14.2% in the third quarter of
2008. The reduction in the G&A ratio between years reflects
improved leveraging of our costs over a higher revenue base and the
impact of additional revenue from new business (Arizona Acute Care,
Florida and South Carolina).
- Earnings per diluted share from
continuing operations were $0.51, compared to $0.41 in the third
quarter of 2008. Earnings per diluted share in 2008 included a
$0.06 loss on investments from the Primary Reserve fund.
Balance Sheet and Cash Flow
At September 30, 2009, the Company had cash and investments of
$939.0 million, including $911.4 million held by its regulated
entities and $27.6 million held by its unregulated entities.
Medical claims liabilities totaled $411.0 million, representing
47.1 days in claims payable, a decrease of 0.4 days from June 30,
2009. Total debt was $277.3 million and debt to capitalization was
31.9%. Year to date cash flow from operations was $177.0
million.
A reconciliation of the Company’s change in days in claims
payable from the immediately preceding quarter-end is presented
below:
Days in claims payable, June 30, 2009 47.5 Payment of annual
provider bonuses (0.7) Impact of Florida expansion 0.3 Days in
claims payable, September 30, 2009 47.1
Outlook
The table below depicts the Company’s annual guidance from
continuing operations for 2009:
Full Year 2009 Low High Premium
and Service revenues (in millions) $ 3,850 $ 3,900 Earnings per
diluted share $ 1.91 $ 1.97
Stock Repurchase Authorization
On October 26, 2009, the Company’s Board of Directors extended
the Company’s stock repurchase program. The program authorizes the
repurchase of up to 4,000,000 shares of the Company’s common stock
from time to time on the open market or through privately
negotiated transactions. No duration has been placed on the
repurchase program and we reserve the right to discontinue the
repurchase program at any time.
Conference Call
As previously announced, the Company will host a conference call
Tuesday, October 27, 2009, at 8:30 A.M. (Eastern Time) to review
the financial results for the second quarter ended September 30,
2009, and to discuss its business outlook. Michael F. Neidorff and
William N. Scheffel will host the conference call. Investors and
other interested parties are invited to listen to the conference
call by dialing 800-273-1254 in the U.S. and Canada, 973-638-3440
from abroad, or via a live Internet broadcast on the Company's
website at www.centene.com, under the Investor Relations section. A
replay will be available for on-demand listening shortly after the
completion of the call until 11:59 PM (Eastern Time) on Tuesday,
November 10, 2009, at the aforementioned URL, or by dialing
800-642-1687 in the U.S. and Canada, or 706-645-9291 from abroad,
and entering access code 30957978.
About Centene Corporation
Centene Corporation is a leading multi-line healthcare
enterprise that provides programs and related services to
individuals receiving benefits under Medicaid, including the
Children’s Health Insurance Program (CHIP), as well as Aged, Blind,
or Disabled (ABD), Foster Care, Long-Term Care and Medicare
(Special Needs Plans). The Company operates local health plans and
offers a wide range of health insurance solutions to individuals
and the rising number of uninsured Americans. It also contracts
with other healthcare and commercial organizations to provide
specialty services including behavioral health, life and health
management, managed vision, telehealth services, pharmacy benefits
management and medication adherence. Information regarding Centene
is available via the Internet at www.centene.com.
The information provided in this press release contains
forward-looking statements that relate to future events and future
financial performance of Centene. Subsequent events and
developments may cause the Company’s estimates to change. The
Company disclaims any obligation to update this forward-looking
financial information in the future. Readers are cautioned that
matters subject to forward-looking statements involve known and
unknown risks and uncertainties, including economic, regulatory,
competitive and other factors that may cause Centene’s or its
industry’s actual results, levels of activity, performance or
achievements to be materially different from any future results,
levels of activity, performance or achievements expressed or
implied by these forward-looking statements. Actual results may
differ from projections or estimates due to a variety of important
factors, including Centene’s ability to accurately predict and
effectively manage health benefits and other operating expenses,
competition, changes in healthcare practices, changes in federal or
state laws or regulations, inflation, provider contract changes,
new technologies, reduction in provider payments by governmental
payors, major epidemics, disasters and numerous other factors
affecting the delivery and cost of healthcare. The expiration,
cancellation or suspension of Centene’s Medicaid Managed Care
contracts by state governments would also negatively affect
Centene.
[Tables Follow]
CENTENE CORPORATION AND
SUBSIDIARIES
CONSOLIDATED BALANCE
SHEETS
(In thousands, except share
data)
(Unaudited)
September 30,
2009
December 31,
2008
ASSETS Current assets: Cash and cash equivalents of
continuing operations $ 389,135 $ 370,999 Cash and cash equivalents
of discontinued operations 4,847 8,100 Total
cash and cash equivalents 393,982 379,099 Premium and related
receivables, net of allowance for uncollectible accounts of $19 and
$595, respectively 104,798 92,531 Short-term investments, at fair
value (amortized cost $45,332 and $108,469, respectively) 45,692
109,393 Other current assets 61,294 75,333 Current assets of
discontinued operations other than cash 8,292 9,987
Total current assets 614,058 666,343 Long-term investments,
at fair value (amortized cost $475,078 and $329,330, respectively)
486,889 332,411 Restricted deposits, at fair value (amortized cost
$17,177 and $9,124, respectively) 17,286 9,254 Property, software
and equipment, net of accumulated depreciation of $96,314 and
$74,194, respectively 209,920 175,858 Goodwill 219,100 163,380
Intangible assets, net 23,454 17,575 Other long-term assets 37,100
59,083 Long-term assets of discontinued operations 27,207
27,248 Total assets $ 1,635,014 $ 1,451,152
LIABILITIES AND STOCKHOLDERS’ EQUITY Current
liabilities: Medical claims liability $ 410,997 $ 373,037 Accounts
payable and accrued expenses 204,411 219,566 Unearned revenue
68,024 17,107 Current portion of long-term debt 645 255 Current
liabilities of discontinued operations 23,846 31,013
Total current liabilities 707,923 640,978 Long-term debt
276,687 264,637 Other long-term liabilities 55,992 43,539 Long-term
liabilities of discontinued operations 1,155 726
Total liabilities 1,041,757 949,880 Commitments and
contingencies Stockholders’ equity: Common stock, $.001 par
value; authorized 100,000,000 shares; issued and outstanding
45,402,369 and 45,071,179 shares, respectively 45 45 Additional
paid-in capital 277,709 263,835 Accumulated other comprehensive
income: Unrealized gain on investments, net of tax 7,812 3,152
Retained earnings 335,192 275,236 Treasury stock, at cost
(2,373,893 and 2,083,415 shares, respectively) (46,497 )
(40,996 ) Total Centene stockholders’ equity 574,261 501,272
Noncontrolling interest 18,996 — Total
stockholders’ equity 593,257 501,272 Total
liabilities and stockholders’ equity $ 1,635,014 $ 1,451,152
CENTENE CORPORATION AND
SUBSIDIARIES
CONSOLIDATED STATEMENTS OF
OPERATIONS
(In thousands, except share
data)
(Unaudited)
Three Months Ended
September 30,
Nine Months Ended
September 30,
2009 2008 2009 2008
Revenues: Premium $ 960,009 $ 817,740 $ 2,754,713 $
2,338,550 Service 27,300 17,962 72,740
56,958 Premium and service revenues 987,309 835,702 2,827,453
2,395,508 Premium tax 50,925 22,897 182,685
66,249 Total revenues 1,038,234 858,599
3,010,138 2,461,757
Expenses: Medical costs 803,062
671,920 2,298,108 1,932,172 Cost of services 15,843 12,854 46,364
43,467 General and administrative expenses 130,024 118,628 381,524
323,391 Premium tax 51,295 23,284 183,785
66,636 Total operating expenses 1,000,224
826,686 2,909,781 2,365,666 Earnings from operations
38,010 31,913 100,357 96,091
Other income (expense):
Investment and other income 3,750 2,708 11,781 15,724 Interest
expense (4,064 ) (4,377 ) (12,210 )
(12,436 ) Earnings from continuing operations, before income tax
expense 37,696 30,244 99,928 99,379 Income tax expense
12,426 12,145 35,060 38,464 Earnings from
continuing operations, net of income tax expense 25,270 18,099
64,868 60,915
Discontinued operations, net of income tax
(benefit) expense of $(792), $242, $(1,148) and $390,
respectively (1,460 ) 149 (2,394 )
1,159 Net earnings 23,810 18,248 62,474 62,074
Noncontrolling
interest 2,542 ― 2,518 ―
Net
earnings attributable to Centene Corporation $ 21,268 $ 18,248
$ 59,956 $ 62,074
Amounts attributable to Centene
Corporation common shareholders: Earnings from continuing
operations, net of income tax expense $ 22,728 $ 18,099 $ 62,350 $
60,915 Discontinued operations, net of income tax (benefit) expense
(1,460 ) 149 (2,394 ) 1,159 Net
earnings $ 21,268 $ 18,248 $ 59,956 $ 62,074
Net earnings
(loss) per share attributable to Centene Corporation: Basic:
Continuing operations $ 0.53 $ 0.42 $ 1.45 $ 1.40 Discontinued
operations (0.04 ) ― (0.06 ) 0.03
Earnings per common share $ 0.49 $ 0.42 $ 1.39 $ 1.43 Diluted:
Continuing operations $ 0.51 $ 0.41 $ 1.41 $ 1.37 Discontinued
operations (0.03 ) ― (0.05 ) 0.02
Earnings per common share $ 0.48 $ 0.41 $ 1.36 $ 1.39
Weighted average number of shares outstanding: Basic
43,001,870
43,232,941
43,023,431 43,381,819 Diluted 44,291,604
44,530,347
44,247,153 44,541,424
CENTENE CORPORATION AND
SUBSIDIARIES
CONSOLIDATED STATEMENTS OF CASH
FLOWS
(In thousands)
Nine Months Ended September 30, 2009
2008 Cash flows from operating
activities: Net earnings $ 62,474 $ 62,074 Adjustments to
reconcile net earnings to net cash provided by operating activities
Depreciation and amortization 30,800 26,018 Stock compensation
expense 11,428 11,576 Loss on sale of investments, net 261 4,923
Deferred income taxes 4,516 13,987 Changes in assets and
liabilities — Premium and related receivables (381 ) (50,797 )
Other current assets (2,595 ) (6,422 ) Other assets (593 ) (713 )
Medical claims liabilities 31,612 28,109 Unearned revenue 54,725
(37,931 ) Accounts payable and accrued expenses (17,656 ) 74,723
Other operating activities 2,386 967 Net cash
provided by operating activities 176,977 126,514
Cash flows from investing activities: Capital expenditures
(42,696 ) (52,588 ) Purchases of investments (647,086 ) (372,221 )
Sales and maturities of investments 546,640 356,367 Investments in
acquisitions, net of cash acquired, and investment in equity method
investee (31,533 )
(83,509
) Net cash used in investing activities (174,675 )
(151,951 )
Cash flows from financing activities: Proceeds
from exercise of stock options 1,717 4,770 Proceeds from borrowings
468,500 152,005 Payment of long-term debt (456,059 ) (109,410 )
Distributions to noncontrolling interest (3,171 ) ― Contribution
from noncontrolling interest 7,495 ― Excess tax benefits from stock
compensation 43 3,016 Common stock repurchases (5,539 ) (18,244 )
Debt issue costs (405 ) ― Net cash provided by
financing activities 12,581 32,137 Net increase in
cash and cash equivalents 14,883 6,700
Cash and
cash equivalents, beginning of period 379,099
268,584
Cash and cash equivalents, end of period $ 393,982 $
275,284 Supplemental disclosures of cash flow information:
Interest paid $ 8,556 $ 8,467 Income taxes paid $ 43,308 $ 28,370
Supplemental disclosure of non-cash investing and financing
activities: Contribution from noncontrolling interest $ 5,491 $ ―
CENTENE CORPORATION
CONTINUING OPERATIONS
SUPPLEMENTAL FINANCIAL DATA
Q3 Q2 Q1 Q4 Q3
2009 2009 2009 2008 2008
MEMBERSHIP Managed Care: Arizona 17,400 16,200 15,500 14,900
— Florida 84,400 22,300 29,100 — — Georgia 303,400 292,800 289,300
288,300 283,900 Indiana 200,700 196,100 179,100 175,300 172,400
Massachusetts 500 — — — — Ohio 151,200 141,200 137,000 133,400
132,500 South Carolina 46,100 46,000 48,500 31,300 26,600 Texas
450,200 443,200 421,100 428,000 433,200 Wisconsin 132,500
131,200 127,700 124,800 122,500 Total
at-risk membership 1,386,400 1,289,000 1,247,300
1,196,000 1,171,100 Non-risk membership 63,200
114,000 96,000 3,700 3,700
TOTAL 1,449,600 1,403,000
1,343,300 1,199,700 1,174,800
Medicaid 1,040,500 958,600 921,100 877,400 850,500
CHIP & Foster Care 263,400 261,400 256,900 257,300 261,800 ABD
& Medicare 82,500 69,000 69,300 61,300
58,800 Total at-risk membership 1,386,400
1,289,000 1,247,300 1,196,000 1,171,100
Non-risk membership 63,200 114,000 96,000
3,700 3,700
TOTAL 1,449,600
1,403,000 1,343,300 1,199,700
1,174,800 Specialty Services(a):
Cenpatico Behavioral Health Arizona 117,300 110,500 104,700 105,000
102,400 Kansas 41,000 41,100 40,600 41,100 40,100 Bridgeway Health
Solutions Long-term Care 2,500 2,400 2,300
2,100 1,900
TOTAL 160,800
154,000 147,600 148,200
144,400 (a) Includes external membership only.
REVENUE PER MEMBER(b) $ 222.77 $ 219.75 $
220.29 $ 218.52 $ 213.28
CLAIMS(b) Period-end
inventory
414,900
362,200
325,000
269,300
323,200
Average inventory 227,100 234,500 267,600 288,600 298,400
Period-end inventory per member 0.30 0.28 0.26 0.23 0.28
(b) Revenue per member and claims information are presented
for the Managed Care at-risk members.
Q3
Q2 Q1 Q4 Q3 2009 2009
2009 2008 2008 DAYS IN CLAIMS
PAYABLE (c) 47.1 47.5 45.3 48.5 47.9 (c) Days in Claims
Payable is a calculation of Medical Claims Liabilities at the end
of the period divided by average claims expense per calendar day
for such period.
CASH AND INVESTMENTS (in millions)
Regulated $ 911.4 $ 825.8 $ 816.8 $ 798.0 $ 692.6 Unregulated
27.6 27.0 28.9 24.1 26.8
TOTAL $ 939.0 $ 852.8 $ 845.7 $ 822.1 $ 719.4
DEBT TO CAPITALIZATION (d) 31.9 % 33.0
% 34.6 % 34.6% 34.4 % (d) Debt to Capitalization is calculated as
follows: total debt divided by (total debt + total equity).
OPERATING RATIOS:
Three Months Ended
September 30,
Nine Months Ended
September 30,
2009 2008 2009
2008 Health Benefits Ratios: Medicaid and CHIP 84.7 % 81.3 %
84.4 % 80.7 % ABD and Medicare 81.1 88.1 81.7 91.4 Specialty
Services 80.5 79.9 79.6 82.9 Total 83.7 82.2 83.4 82.6
General & Administrative Expense Ratio 13.2 % 14.2 % 13.5 %
13.5 %
MEDICAL CLAIMS LIABILITY (In
thousands)Four rolling quarters of the changes in medical
claims liability are summarized as follows:
Balance, September 30, 2008 $ 349,502 Acquisitions —
Incurred related to: Current period 3,051,905 Prior period
(45,634 ) Total incurred 3,006,271 Paid related to:
Current period 2,654,707 Prior period 290,069 Total
paid 2,944,776
Balance, September 30, 2009 $
410,997
Centene’s claims reserving process utilizes a consistent
actuarial methodology to estimate Centene’s ultimate liability. Any
reduction in the “Incurred related to: Prior period” amount may be
offset as Centene actuarially determines “Incurred related to:
Current period.” As such, only in the absence of a consistent
reserving methodology would favorable development of prior period
claims liability estimates reduce medical costs. Centene believes
it has consistently applied its claims reserving methodology in
each of the periods presented.
The amount of the “Incurred related to: Prior period” above
includes the effects of reserving under moderately adverse
conditions, new markets where we use a conservative approach in
setting reserves during the initial periods of operations,
increased receipts from other third party payors related to
coordination of benefits and lower medical utilization and cost
trends for dates of service prior to September 30, 2008.
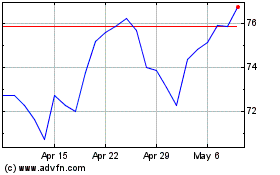
Centene (NYSE:CNC)
Historical Stock Chart
From May 2024 to Jun 2024
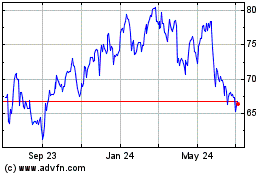
Centene (NYSE:CNC)
Historical Stock Chart
From Jun 2023 to Jun 2024