By Christopher Weaver, Anna Wilde Mathews and Tom McGinty
Thousands of Covid-19 rapid-testing devices are sitting idle in
nursing homes around the country, even as some of the facilities
face delays in getting results from outside labs, according to
federal data.
The federal government spent more than $100 million to send
rapid-testing equipment to the vast majority of the nation's
nursing homes, but some industry executives say they are concerned
about the accuracy of the point-of-care tests, the staff time
involved in using them, and guidelines in some states that
discourage use of the tests.
Nearly 30% of 13,150 facilities that had rapid-testing equipment
for at least two weeks hadn't used it to test a single resident or
staff member, according to a federal survey of nursing homes.
During weeks when regulations from the Centers for Medicare and
Medicaid Services required them to do testing due to local
outbreaks, hundreds of facilities didn't use the rapid-testing
equipment at all, the survey shows.
The equipment, which allows nursing homes to perform tests on
the premises and get fast results, is supposed to help ensure that
facilities can catch coronavirus infections early, before they
spread. Long-term care facilities have been tied to more than
88,000 Covid-19 deaths in the U.S. since the start of the pandemic,
according to a Journal tally of recent state, local and federal
data.
"They need accurate testing with rapid turnaround that isn't
adding an additional burden on nursing-home staff," said Michael L.
Barnett, an assistant professor at the Harvard T.H. Chan School of
Public Health. The federally-supplied machines "are not providing
what they need, and they're voting with their feet."
As Covid-19 cases surge around the country, more people are
seeking tests. "There's absolutely waste" in providing nursing
homes with testing machines that aren't being used, Dr. Barnett
said.
"It's not what we need," said Barbara Klick, chief executive of
Sholom Community Alliance, a nonprofit that uses a lab to test
around 500 staffers a week at its two nursing homes in St. Paul and
St. Louis Park, Minn. Using the rapid-testing equipment sent by the
federal government requires too much staff time, largely for
documentation and filing results with the government, she said.
Ms. Klick also worries about the risk of false negative and
false positive results from the rapid tests: "It's too
unreliable."
In addition to the nursing homes that haven't yet used the
devices, another 16% reported using them on fewer than 20 residents
and workers, according to the survey data, which is released weekly
by CMS and currently updated through the week ending Oct. 25.
Almost half, or 48%, of the nursing homes reported they hadn't
used their rapid testing equipment in the most recent week included
in the data. Among nursing homes that were required under federal
rules to test staff at least once a week due to local outbreaks,
41% said they hadn't used it in the most recent week.
Around 4,900 nursing homes that hadn't used the rapid-testing
devices in the most recent week said in the survey that instead
they were waiting a day or more for test results from labs.
The rapid tests the federal government provided to nursing
homes, known as antigen tests, focus on virus proteins, while
molecular tests, the type generally done by labs, look for the
virus's genetic material. Lab-based molecular assays tend to be
more precise than the fast antigen tests.
Because of concerns about possible false negative and false
positive results with antigen tests, particularly when used to
screen people without symptoms, public-health officials recommend
follow-up confirmatory testing under some circumstances.
The Department of Health and Human Services in July announced
plans to ship rapid antigen testing machines made by Becton
Dickinson & Co. and Quidel Corp. to about 14,000 nursing homes
around the country. An HHS spokeswoman said the cost of the effort
has been around $116 million.
"This new testing initiative is critical for keeping vulnerable
older adults safe," CMS administrator Seema Verma said in a
statement at the time. The department later announced it also would
send nursing homes a rapid antigen test made by Abbott
Laboratories, known as the BinaxNOW COVID-19 Ag Card, a device
roughly the size of a credit card.
Brett Giroir, the assistant secretary at the Department of
Health and Human Services who oversaw the program, said 99.3% of
nursing homes had recently reported being able to test their entire
staffs, a key to keeping the virus out of their facilities. He said
it was "fine" for facilities to use the point-of-care devices from
the government or other methods.
"We are providing options to meet CMS requirements," Dr. Giroir
said, referring to the rules from the Medicare agency that require
testing.
An HHS spokeswoman said nursing homes had ordered an additional
4.2 million tests from Becton Dickinson, showing they are using the
equipment.
Dr. Giroir has previously defended the performance of the rapid
antigen tests. The Food and Drug Administration this week warned
about the potential for false positive results, noting that they
sometimes occur when users don't follow the manufacturers'
instructions.
Quidel, Becton Dickinson and Abbott all said their devices
perform very well when used correctly. A spokeswoman for Quidel
said it offers customers "a multifaceted approach to training,"
including a lot of support.
Becton Dickinson said in a statement that testing, including
rapid antigen tests, plays "an essential role in detecting Covid-19
and helping to disrupt community spread." Most nursing homes that
have its machines are getting regular reorders of tests, the
company said.
Abbott said it has worked with nursing homes "proactively to
ensure they have the resources needed to best deploy BinaxNOW,
including conducting webinars and reaching out to facilities
individually."
The HHS spokeswoman said it wasn't clear whether nursing homes
were including the Abbott tests in their answers to the federal
survey, and that some facilities may be using rapid tests to check
visitors.
Some states have discouraged use of the rapid antigen tests.
Massachusetts, for instance, has said they can't be used to satisfy
state testing mandates for nursing homes.
In North Dakota, where Covid-19 cases are rising, an October
state guidance urged cautious procedures in using the antigen
tests, suggesting that negative results don't rule out Covid-19 and
some positives need to be re-tested.
"The state's not accepting them yet as valid tests," said Sandy
Gerving, the administrator of Marian Manor Healthcare Center, an
independent nonprofit nursing home in Glen Ullin, N.D. Using the
device HHS distributed "seemed like a waste of effort," she
said.
Marian Manor had an outbreak in September, Ms. Gerving said, as
the virus spread widely in the surrounding community. Thirteen
patients died of the virus, federal survey data show. Ms. Gerving
said the outbreak at the facility was over. She said the facility
had had to test the entire staff 23 times as of Tuesday under state
and federal guidelines, sending samples to an outside lab.
Meantime, Marian Manor's point-of-care testing device and its
supplies are still in their boxes, Ms. Gerving said. "We're waiting
to see, do we send it back or whatever," she said.
Officials at North Dakota's health department didn't immediately
respond to requests for comment.
--Brianna Abbott contributed to this article.
Write to Christopher Weaver at christopher.weaver@wsj.com, Anna
Wilde Mathews at anna.mathews@wsj.com and Tom McGinty at
tom.mcginty@wsj.com
(END) Dow Jones Newswires
November 07, 2020 12:31 ET (17:31 GMT)
Copyright (c) 2020 Dow Jones & Company, Inc.
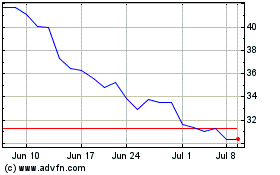
QuidelOrtho (NASDAQ:QDEL)
Historical Stock Chart
From Oct 2024 to Nov 2024
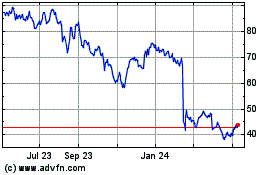
QuidelOrtho (NASDAQ:QDEL)
Historical Stock Chart
From Nov 2023 to Nov 2024