– Durability of Response and Continued
Manageable Safety Profile for the Phase 1 and iMMagine-1 Studies
with Anito-cel in Patients with Relapsed/Refractory Multiple
Myeloma to be Presented by Partner Arcellx; Follows Progress with
First Patient Dosed in Phase 3 iMMagine-3 Study –
– Survival Rate for Yescarta® Supported by
Largest Real-World Analysis of CAR T for Second-Line Therapy in
Patients with Relapsed/Refractory Large B-Cell Lymphoma –
– Durability of Response and Long-Term
Survival with Yescarta® and Tecartus® in Multiple Blood Cancers
Observed in ZUMA-5, ZUMA-2, and ZUMA-3 Studies –
Kite, a Gilead Company (Nasdaq: GILD), will share 18
presentations, including six oral presentations, demonstrating the
strength of its CAR T-cell therapy portfolio across a spectrum of
blood cancers during the 66th American Society of Hematology (ASH)
Annual Meeting and Exposition (December 7-10).
“Our data underscore our commitment to helping people with blood
cancers live longer and demonstrate the benefit of CAR T-cell
therapy as a mainstay of blood cancer treatment,” said Dominique
Tonelli, M.D., VP, Global Head of Medical Affairs, Kite. “Notably
for this year, along with our partner Arcellx, we are excited to
share clinically meaningful data from the Phase 1 study and the
iMMagine-1 Phase 2 registrational study of anito-cel for the
treatment of relapsed/refractory multiple myeloma.”
Anito-cel Data from Partner,
Arcellx
Key presentations for anitocabtagene autoleucel (anito-cel)
include data from the Phase 1 study that demonstrate a 30.2-month
median progression-free survival (PFS) with a median follow-up of
38.1 months and the median overall survival not yet reached; and
preliminary results from 58 patients in the Phase 2 iMMagine-1
study that demonstrate a 95% objective response rate (ORR) and a
62% complete response / stringent complete response (CR/sCR) at a
median follow-up of 10.3 months. Additional patients with a more
recent data cut for the Phase 2 iMMagine-1 study will be presented
in an oral presentation.
Both the Phase 1 and Phase 2 iMMagine-1 studies highlight
durable responses in patients with relapsed or refractory (R/R)
multiple myeloma (MM) and show no delayed neurotoxicities have been
observed to date, including no parkinsonism, no cranial nerve
palsies, and no Guillain Barre syndrome.
Positive Survival Outcomes with
Yescarta® and
Tecartus®
Key presentations for Yescarta® (axicabtagene ciloleucel)
include a five-year follow-up analysis from ZUMA-5 evaluating
response rate and long-term survival in patients with R/R indolent
non-Hodgkin lymphoma (iNHL), including follicular lymphoma and
marginal zone lymphoma. Additionally, Yescarta is the only
treatment to have demonstrated superior overall survival versus
standard therapy for patients with early R/R large B-cell lymphoma
(LBCL), and this continues to be seen in the largest real-world
analysis of patients with R/R LBCL who received second-line
Yescarta. Additional research will focus on improvements in
Yescarta manufacturing for patients with R/R LBCL.
Key presentations for Tecartus® (brexucabtagene autoleucel)
include five-year outcomes from ZUMA-2 cohorts 1 and 2 and a
primary analysis of ZUMA-2 cohort 3, both highlighting durable
responses in adult patients with R/R mantle cell lymphoma (MCL) and
showing that Tecartus continues to deliver unprecedented efficacy
in R/R MCL three years after its approval. Also to be presented are
real-world outcomes in adults with R/R B-cell precursor acute
lymphoblastic leukemia (B-ALL) treated with Tecartus, highlighting
the CAR T-cell therapy’s high effectiveness in a broader R/R B-ALL
patient population.
Advancements in Kite’s pipeline will also be highlighted,
including data presented on Kite’s next generation CAR T-cell
therapy KITE-753, an autologous anti-CD19/CD20 CAR T-cell therapy
for the treatment of B-cell malignancies.
Kite is also collaborating with independent investigators and
respected institutions including The Lymphoma Study Association,
Sarah Cannon Transplant and Cellular Therapy Network, and
Dana-Farber Cancer Institute to share additional insights on Kite’s
CAR T-cell therapies.
Dates and times* for accepted abstracts and presentations of
note are as follows:
*Times listed are in PT
Oral Presentations
Abstract Details
Titles
Axicabtagene ciloleucel
Abstract #526
Sunday, December 8, 2024
10:15 AM
Marriott Marquis San Diego Marina, Pacific
Ballroom Salons 24-26
Real-World Early Outcomes of Second-Line
Axicabtagene Ciloleucel (Axi-Cel) Therapy in Patients (Pts) With
Relapsed or Refractory (R/R) Large B-Cell Lymphoma (LBCL)
Abstract #527
Sunday, December 8, 2024
10:30 AM
Marriott Marquis San Diego Marina, Pacific
Ballroom Salons 24-26
Real-world Trends of Cytokine Release
Syndrome and Neurologic Events, and Pattern of Their Management
among Patients Receiving Axicabtagene Ciloleucel for Relapsed or
Refractory (r/r) Large B-cell Lymphoma (LBCL) in the US: a CIBMTR
Report
Abstract #609
Sunday, December 8, 2024
12:30 PM
Marriott Marquis San Diego Marina,
Marriott Grand Ballroom 2-4
Predictors of Early Safety Outcomes with
Axicabtagene Ciloleucel (axi-cel) in Patients with Relapsed or
Refractory (R/R) Large B-Cell Lymphoma (LBCL)
Abstract #864
Monday, December 9, 2024
4:00 PM
Marriott Marquis San Diego Marina,
Marriott Grand Ballroom 11-13
5-Year Follow-Up Analysis From ZUMA-5: a
Phase 2 Trial of Axicabtagene Ciloleucel (Axi-Cel) in Patients With
Relapsed/Refractory Indolent Non-Hodgkin Lymphoma
Brexucabtagene autoleucel
Abstract #748
Monday, December 9, 2024
11:15 AM
Marriott Marquis San Diego Marina,
Marriott Grand Ballroom 8-9
Primary Analysis of ZUMA-2 Cohort 3:
Brexucabtagene Autoleucel (Brexu-Cel) in Patients (Pts) With
Relapsed/Refractory Mantle Cell Lymphoma (R/R MCL) Who Were Naive
to Bruton Tyrosine Kinase Inhibitors (BTKi)
Anitocabtagene autoleucel
Abstract #1031
Monday, December 9, 2024
5:30 PM
Marriott Marquis San Diego Marina, Pacific
Ballroom 24-26
Phase 2 Registrational Study of
Anitocabtagene Autoleucel for the Treatment of Patients With
Relapsed and/or Refractory Multiple Myeloma: Preliminary Results
From the iMMagine-1 Trial
*Led by Arcellx
Poster Presentations
Axicabtagene ciloleucel
Abstract #2367
Saturday, December 7, 2024
5:30 PM - 7:30 PM
San Diego Convention Center, Halls G-H
Treatment Patterns and Predictors of
Survival after First Line Therapy in Large B-Cell Lymphoma in a
Real-World US Cohort
Abstract #3347
Sunday, December 8, 2024
6:00 PM - 8:00 PM
San Diego Convention Center, Halls G-H
Improvements in Axicabtagene Ciloleucel
Manufacturing Result in High Delivery Success and More Predictable
Turnaround Time for Patients With Relapsed/Refractory Large B-Cell
Lymphoma
Abstract #4368
Monday, December 9, 2024
6:00 PM - 8:00 PM
San Diego Convention Center, Halls G-H
Impact of Inflammation, Tumor and Product
Attributes on Clinical Outcomes in Patients with
Relapsed/Refractory Follicular Lymphoma Treated with Axicabtagene
Ciloleucel
Abstract #5037
Monday, December 9, 2024
6:00 PM - 8:00 PM
San Diego Convention Center, Halls G-H
Estimating the Impact on Survival of Not
Receiving CAR T Therapy Despite Being Eligible in Relapsed or
Refractory (R/R) Diffuse Large B-Cell Lymphoma (DLBCL) Patients in
Germany
Brexucabtagene autoleucel
Abstract #4388
Monday, December 9, 2024
6:00 PM - 8:00 PM
San Diego Convention Center, Halls G-H
Five-Year Outcomes of Patients (Pts) With
Relapsed/Refractory Mantle Cell Lymphoma (R/R MCL) Treated With
Brexucabtagene Autoleucel (Brexu-cel) in ZUMA-2 Cohorts 1 and 2
Abstract #5092
Monday, December 9, 2024
6:00 PM - 8:00 PM
San Diego Convention Center, Halls G-H
Real-World (RW) Outcomes for
Brexucabtagene Autoleucel (Brexu-Cel) Treatment in Patients (Pts)
With Relapsed or Refractory B-Cell Acute Lymphoblastic Leukemia
(R/R B-ALL) by High-Risk Features and Prior Treatments: Updated
Evidence From the CIBMTR® Registry
Abstract #4193
Monday, December 9, 2024
6:00 PM - 8:00 PM
San Diego Convention Center, Halls G-H
Impact of disease burden, CAR-T expansion,
and mononuclear cell recovery on overall response and duration of
response in ZUMA-3 pivotal study
Anitocabtagene autoleucel
Abstract #4825
Monday, December 9, 2024
6:00 PM - 8:00 PM
San Diego Convention Center, Halls G-H
Phase 1 Study of Anitocabtagene Autoleucel
for the Treatment of Patients With Relapsed and/or Refractory
Multiple Myeloma (RRMM): Efficacy and Safety With 34-Month Median
Follow-up
*Led by Arcellx
Kite next generation CAR T-cell
therapies
Abstract #3481
Sunday, December 8, 2024
6:00 PM - 8:00 PM
San Diego Convention Center, Halls G-H
KITE-753: An Autologous Rapid Manufactured
Anti-CD19/CD20 CAR-T Product for the Treatment of B-cell
Malignancies
Investigator-Sponsored /
Collaboration**
Abstract #4505
Sunday, December 8, 2024
6:00 PM - 8:00 PM
San Diego Convention Center, Halls G-H
Health-related quality of life after
Axi-cel as a second-line therapy in patients with high-risk
relapsed/refractory large B-cell lymphoma who are ineligible for
autologous stem cell transplantation: results of the ALYCANTE phase
II trial
*Led by The Lymphoma Study Association
Abstract #4721
Monday, December 9, 2024
6:00 PM - 8:00 PM
San Diego Convention Center, Halls G-H
Health Related Quality of Life (HRQoL) in
Relapsed/Refractory Multiple Myeloma (RRMM): A Systematic
Literature Review (SLR) and Meta-Analysis
*Investigator led
Abstract #3734
Sunday, December 8, 2024
6:00 PM - 8:00 PM
San Diego Convention Center, Halls G-H
The Patient Journey and Treatment Outcomes
Comparing Inpatient Versus Outpatient Axicabtagene Ciloleucel in
Non-Hodgkin’s Lymphoma (NHL) - a Large, Multicenter Study
*In collaboration with Sarah Cannon
Transplant and Cellular Therapy Network
Abstract #3124
Sunday, December 8, 2024
6:00 PM - 8:00 PM
San Diego Convention Center, Halls G-H
CAR T-cells for relapsed/refractory B-cell
lymphoma in people living with HIV (PLWH): a LYSA study from the
DESCAR-T registry
*Led by The Lymphoma Study Association
Abstract #2031
Saturday, December 7, 2024
6:00 PM - 8:00 PM
San Diego Convention Center, Halls G-H
Early MRD detection after CAR-T Associated
with Poor Outcome in LBCL
*In collaboration with Dana-Farber Cancer
Institute
Abstract #239
Saturday, December 7, 2024
3:00 PM
Session: 623 (2:00 - 3:30 PM)
Marriot Grand Ballroom 11-13
Outcome of patients with Mantle cell
lymphoma after failure of anti-CD19 CAR T-cell therapy: a DESCAR-T
Study By Lysa Group
*Led by The Lymphoma Study Association
Abstract #
Date TBD
Time TBD
Room TBD
A Real-World Weighted Comparison of
Tisagenlecleucel and Axicabtagene Ciloleucel CAR T Cells in
Relapsed or Refractory Diffuse Large B Cell Lymphoma Aged 75 Years
and Older: A Lysa Study from the Descar-T Registry
*Led by The Lymphoma Study Association
Publication Only
Abstract #7775
Real-World Interim PET/CT Scan Use During
Frontline (1L) Therapy and Subsequent Treatment Characteristics in
Patients with Refractory Diffuse Large B-Cell Lymphoma (DLBCL)
Abstract #7607
Short-term Costs Associated With
Outpatient Use of Axicabtagene Ciloleucel in Second-line
Relapsed/Refractory Large B-cell Lymphoma Based on ZUMA-24 Clinical
Trial
Abstract #7592
A United States (US) Cost-Effectiveness
Analysis of Axicabtagene Ciloleucel Compared to Odronextamab in
Third Line or Later (3L+) Diffuse Large B-Cell Lymphoma
Abstract #6962
Treatment Patterns and Outcomes in
Triple-Class Exposed Patients with Relapsed and Refractory Multiple
Myeloma: Findings from the Flatiron Database
Abstract #7159
In Vitro and In Vivo Characterization of
Axicabtagene Ciloleucel Identifies Features Associated with
Treatment Resistance in Patients, Including a Dysfunctional CD8+ T
Cell State Characterized by Overexpression of GATA3 Transcript
For more information, including a complete list of abstract
titles at the meeting, please visit:
https://ash.confex.com/ash/2024/webprogram/start.html
**Presentations independently led and sponsored feature Kite CAR
T-cell therapies but are not included in total number of Kite
accepted abstracts.
About Yescarta
Please see full Prescribing Information, including BOXED
WARNING and Medication Guide.
YESCARTA is a CD19-directed genetically modified autologous T
cell immunotherapy indicated for the treatment of:
- Adult patients with large B-cell lymphoma that is refractory to
first-line chemoimmunotherapy or that relapses within 12 months of
first-line chemoimmunotherapy.
- Adult patients with relapsed or refractory large B-cell
lymphoma after two or more lines of systemic therapy, including
diffuse large B-cell lymphoma (DLBCL) not otherwise specified,
primary mediastinal large B-cell lymphoma, high grade B-cell
lymphoma, and DLBCL arising from follicular lymphoma. Limitations
of Use: YESCARTA is not indicated for the treatment of patients
with primary central nervous system lymphoma.
- Adult patients with relapsed or refractory follicular lymphoma
(FL) after two or more lines of systemic therapy. This indication
is approved under accelerated approval based on response rate.
Continued approval for this indication may be contingent upon
verification and description of clinical benefit in confirmatory
trial(s).
U.S. IMPORTANT SAFETY INFORMATION
BOXED WARNING: CYTOKINE RELEASE SYNDROME, NEUROLOGIC
TOXICITIES and SECONDARY HEMATOLOGICAL MALIGNANCIES
- Cytokine Release Syndrome (CRS), including fatal or
life-threatening reactions, occurred in patients receiving
YESCARTA. Do not administer YESCARTA to patients with active
infection or inflammatory disorders. Treat severe or
life-threatening CRS with tocilizumab or tocilizumab and
corticosteroids.
- Neurologic toxicities, including fatal or life-threatening
reactions, occurred in patients receiving YESCARTA, including
concurrently with CRS or after CRS resolution. Monitor for
neurologic toxicities after treatment with YESCARTA. Provide
supportive care and/or corticosteroids, as needed.
- T cell malignancies have occurred following treatment of
hematologic malignancies with BCMA- and CD19-directed genetically
modified autologous T cell immunotherapies, including
YESCARTA.
- YESCARTA is available only through a restricted program
under a Risk Evaluation and Mitigation Strategy (REMS) called the
YESCARTA and TECARTUS REMS Program.
CYTOKINE RELEASE SYNDROME (CRS)
CRS, including fatal or life-threatening reactions, occurred
following treatment with YESCARTA. CRS occurred in 90% (379/422) of
patients with non-Hodgkin lymphoma (NHL) receiving YESCARTA,
including ≥ Grade 3 (Lee grading system1) CRS in 9%. CRS occurred
in 93% (256/276) of patients with large B-cell lymphoma (LBCL),
including ≥ Grade 3 CRS in 9%. Among patients with LBCL who died
after receiving YESCARTA, four had ongoing CRS events at the time
of death. For patients with LBCL in ZUMA-1, the median time to
onset of CRS was 2 days following infusion (range: 1 to 12 days)
and the median duration of CRS was 7 days (range: 2 to 58 days).
For patients with LBCL in ZUMA-7, the median time to onset of CRS
was 3 days following infusion (range: 1 to 10 days) and the median
duration was 7 days (range: 2 to 43 days).
CRS occurred in 84% (123/146) of patients with indolent
non-Hodgkin lymphoma (iNHL) in ZUMA-5, including ≥ Grade 3 CRS in
8%. Among patients with iNHL who died after receiving YESCARTA, one
patient had an ongoing CRS event at the time of death. The median
time to onset of CRS was 4 days (range: 1 to 20 days) and the
median duration was 6 days (range: 1 to 27 days) for patients with
iNHL.
Key manifestations of CRS (≥ 10%) in all patients combined
included fever (85%), hypotension (40%), tachycardia (32%), chills
(22%), hypoxia (20%), headache (15%), and fatigue (12%). Serious
events that may be associated with CRS include, cardiac arrhythmias
(including atrial fibrillation and ventricular tachycardia), renal
insufficiency, cardiac failure, respiratory failure, cardiac
arrest, capillary leak syndrome, multi-organ failure, and
hemophagocytic lymphohistiocytosis/macrophage activation syndrome
(HLH/MAS).
The impact of tocilizumab and/or corticosteroids on the
incidence and severity of CRS was assessed in two subsequent
cohorts of LBCL patients in ZUMA-1. Among patients who received
tocilizumab and/or corticosteroids for ongoing Grade 1 events. CRS
occurred in 93% (38/41), including 2% (1/41) with Grade 3 CRS; no
patients experienced a Grade 4 or 5 event. The median time to onset
of CRS was 2 days (range: 1 to 8 days) and the median duration of
CRS was 7 days (range: 2 to 16 days).
Prophylactic treatment with corticosteroids was administered to
a cohort of 39 patients for 3 days beginning on the day of infusion
of YESCARTA. Thirty-one of the 39 patients (79%) developed CRS at
which point the patients were managed with tocilizumab and/or
therapeutic doses of corticosteroids with no patients developing
Grade 3 or higher CRS. The median time to onset of CRS was 5 days
(range: 1 to 15 days) and the median duration of CRS was 4 days
(range: 1 to 10 days). Although there is no known mechanistic
explanation, consider the risk and benefits of prophylactic
corticosteroids in the context of pre-existing comorbidities for
the individual patient and the potential for the risk of Grade 4
and prolonged neurologic toxicities.
Ensure that 2 doses of tocilizumab are available prior to
infusion of YESCARTA. Monitor patients at least daily for 7 days at
the certified healthcare facility following infusion for signs and
symptoms of CRS. Monitor patients for signs or symptoms of CRS for
4 weeks after infusion. Counsel patients to seek immediate medical
attention should signs or symptoms of CRS occur at any time. At the
first sign of CRS, institute treatment with supportive care,
tocilizumab, or tocilizumab and corticosteroids as indicated.
NEUROLOGIC TOXICITIES
Neurologic toxicities (including immune effector cell-associated
neurotoxicity syndrome) that were fatal or life- threatening
occurred. Neurologic toxicities occurred in 78% (330/422) of all
patients with NHL receiving YESCARTA, including ≥ Grade 3 in 25%.
Neurologic toxicities occurred in 87% (94/108) of patients with
LBCL in ZUMA-1, including ≥ Grade 3 in 31% and in 74% (124/168) of
patients in ZUMA-7 including ≥ Grade 3 in 25%. The median time to
onset was 4 days (range: 1-43 days) and the median duration was 17
days for patients with LBCL in ZUMA-1. The median time to onset for
neurologic toxicity was 5 days (range:1- 133 days) and median
duration was 15 days in patients with LBCL in ZUMA-7. Neurologic
toxicities occurred in 77% (112/146) of patients with iNHL,
including ≥ Grade 3 in 21%. The median time to onset was 6 days
(range: 1-79 days) and the median duration was 16 days.
Ninety-eight percent of all neurologic toxicities in patients with
LBCL and 99% of all neurologic toxicities in patients with iNHL
occurred within the first 8 weeks of YESCARTA infusion. Neurologic
toxicities occurred within the first 7 days of infusion for 87% of
affected patients with LBCL and 74% of affected patients with
iNHL.
The most common neurologic toxicities (≥ 10%) in all patients
combined included encephalopathy (50%), headache (43%), tremor
(29%), dizziness (21%), aphasia (17%), delirium (15%), and insomnia
(10%). Prolonged encephalopathy lasting up to 173 days was noted.
Serious events, including aphasia, leukoencephalopathy, dysarthria,
lethargy, and seizures occurred. Fatal and serious cases of
cerebral edema and encephalopathy, including late-onset
encephalopathy, have occurred.
The impact of tocilizumab and/or corticosteroids on the
incidence and severity of neurologic toxicities was assessed in 2
subsequent cohorts of LBCL patients in ZUMA-1. Among patients who
received corticosteroids at the onset of Grade 1 toxicities,
neurologic toxicities occurred in 78% (32/41) and 20% (8/41) had
Grade 3 neurologic toxicities; no patients experienced a Grade 4 or
5 event. The median time to onset of neurologic toxicities was 6
days (range: 1-93 days) with a median duration of 8 days (range:
1-144 days). Prophylactic treatment with corticosteroids was
administered to a cohort of 39 patients for 3 days beginning on the
day of infusion of YESCARTA. Of those patients, 85% (33/39)
developed neurologic toxicities, 8% (3/39) developed Grade 3, and
5% (2/39) developed Grade 4 neurologic toxicities. The median time
to onset of neurologic toxicities was 6 days (range: 1-274 days)
with a median duration of 12 days (range: 1-107 days). Prophylactic
corticosteroids for management of CRS and neurologic toxicities may
result in higher grade of neurologic toxicities or prolongation of
neurologic toxicities, delay the onset and decrease the duration of
CRS.
Monitor patients for signs and symptoms of neurologic toxicities
at least daily for 7 days at the certified healthcare facility, and
for 4 weeks thereafter, and treat promptly.
REMS
Because of the risk of CRS and neurologic toxicities, YESCARTA
is available only through a restricted program called the YESCARTA
and TECARTUS REMS Program which requires that: Healthcare
facilities that dispense and administer YESCARTA must be enrolled
and comply with the REMS requirements and must have on-site,
immediate access to a minimum of 2 doses of tocilizumab for each
patient for infusion within 2 hours after YESCARTA infusion, if
needed for treatment of CRS. Certified healthcare facilities must
ensure that healthcare providers who prescribe, dispense, or
administer YESCARTA are trained about the management of CRS and
neurologic toxicities. Further information is available at
www.YescartaTecartusREMS.com or 1-844-454-KITE (5483).
HYPERSENSITIVITY REACTIONS
Allergic reactions, including serious hypersensitivity reactions
or anaphylaxis, may occur with the infusion of YESCARTA.
SERIOUS INFECTIONS
Severe or life-threatening infections occurred. Infections (all
grades) occurred in 45% of patients with NHL. Grade 3 or higher
infections occurred in 17% of patients, including ≥ Grade 3 or
higher infections with an unspecified pathogen in 12%, bacterial
infections in 5%, viral infections in 3%, and fungal infections in
1%. YESCARTA should not be administered to patients with clinically
significant active systemic infections. Monitor patients for signs
and symptoms of infection before and after infusion and treat
appropriately. Administer prophylactic antimicrobials according to
local guidelines.
Febrile neutropenia was observed in 36% of all patients with NHL
and may be concurrent with CRS. In the event of febrile
neutropenia, evaluate for infection and manage with broad-spectrum
antibiotics, fluids, and other supportive care as medically
indicated.
In immunosuppressed patients, including those who have received
YESCARTA, life-threatening and fatal opportunistic infections
including disseminated fungal infections (e.g., candida sepsis and
aspergillus infections) and viral reactivation (e.g., human herpes
virus-6 [HHV-6] encephalitis and JC virus progressive multifocal
leukoencephalopathy [PML]) have been reported. The possibility of
HHV-6 encephalitis and PML should be considered in immunosuppressed
patients with neurologic events and appropriate diagnostic
evaluations should be performed. Hepatitis B virus (HBV)
reactivation, in some cases resulting in fulminant hepatitis,
hepatic failure, and death, can occur in patients treated with
drugs directed against B cells, including YESCARTA. Perform
screening for HBV, HCV, and HIV in accordance with clinical
guidelines before collection of cells for manufacturing.
PROLONGED CYTOPENIAS
Patients may exhibit cytopenias for several weeks following
lymphodepleting chemotherapy and YESCARTA infusion. ≥ Grade 3
cytopenias not resolved by Day 30 following YESCARTA infusion
occurred in 39% of all patients with NHL and included neutropenia
(33%), thrombocytopenia (13%), and anemia (8%). Monitor blood
counts after infusion.
HYPOGAMMAGLOBULINEMIA
B-cell aplasia and hypogammaglobulinemia can occur.
Hypogammaglobulinemia was reported as an adverse reaction in 14% of
all patients with NHL. Monitor immunoglobulin levels after
treatment and manage using infection precautions, antibiotic
prophylaxis, and immunoglobulin replacement. The safety of
immunization with live viral vaccines during or following YESCARTA
treatment has not been studied. Vaccination with live virus
vaccines is not recommended for at least 6 weeks prior to the start
of lymphodepleting chemotherapy, during YESCARTA treatment, and
until immune recovery following treatment.
SECONDARY MALIGNANCIES
Patients treated with YESCARTA may develop secondary
malignancies. T cell malignancies have occurred following treatment
of hematologic malignancies with BCMA- and CD19-directed
genetically modified autologous T cell immunotherapies, including
YESCARTA. Mature T cell malignancies, including CAR-positive
tumors, may present as soon as weeks following infusion, and may
include fatal outcomes.
Monitor life-long for secondary malignancies. In the event that
a secondary malignancy occurs, contact Kite at 1-844-454-KITE
(5483) to obtain instructions on patient samples to collect for
testing.
EFFECTS ON ABILITY TO DRIVE AND USE MACHINES
Due to the potential for neurologic events, including altered
mental status or seizures, patients are at risk for altered or
decreased consciousness or coordination in the 8 weeks following
YESCARTA infusion. Advise patients to refrain from driving and
engaging in hazardous occupations or activities, such as operating
heavy or potentially dangerous machinery, during this initial
period.
ADVERSE REACTIONS
The most common non-laboratory adverse reactions (incidence ≥
20%) in patients with LBCL in ZUMA-7 included fever, CRS, fatigue,
hypotension, encephalopathy, tachycardia, diarrhea, headache,
musculoskeletal pain, nausea, febrile neutropenia, chills, cough,
infection with unspecified pathogen, dizziness, tremor, decreased
appetite, edema, hypoxia, abdominal pain, aphasia, constipation,
and vomiting.
The most common adverse reactions (incidence ≥ 20%) in patients
with LBCL in ZUMA-1 included CRS, fever, hypotension,
encephalopathy, tachycardia, fatigue, headache, decreased appetite,
chills, diarrhea, febrile neutropenia, infections with pathogen
unspecified, nausea, hypoxia, tremor, cough, vomiting, dizziness,
constipation, and cardiac arrhythmias.
The most common non-laboratory adverse reactions (incidence ≥
20%) in patients with iNHL in ZUMA-5 included fever, CRS,
hypotension, encephalopathy, fatigue, headache, infections with
pathogen unspecified, tachycardia, febrile neutropenia,
musculoskeletal pain, nausea, tremor, chills, diarrhea,
constipation, decreased appetite, cough, vomiting, hypoxia,
arrhythmia, and dizziness.
About Tecartus
Please see full FDA Prescribing Information, including BOXED
WARNING and Medication Guide.
Tecartus is a CD19-directed genetically modified autologous T
cell immunotherapy indicated for the treatment of:
- Adult patients with relapsed or refractory mantle cell lymphoma
(MCL). This indication is approved under accelerated approval based
on overall response rate and durability of response. Continued
approval for this indication may be contingent upon verification
and description of clinical benefit in a confirmatory trial.
- Adult patients with relapsed or refractory B-cell precursor
acute lymphoblastic leukemia (ALL).
U.S. IMPORTANT SAFETY INFORMATION
BOXED WARNING: CYTOKINE RELEASE SYNDROME, NEUROLOGIC
TOXICITIES and SECONDARY HEMATOLOGICAL MALIGNANCIES
- Cytokine Release Syndrome (CRS), including life-threatening
reactions, occurred in patients receiving Tecartus. Do not
administer Tecartus to patients with active infection or
inflammatory disorders. Treat severe or life-threatening CRS with
tocilizumab or tocilizumab and corticosteroids.
- Neurologic toxicities, including life-threatening reactions,
occurred in patients receiving Tecartus, including concurrently
with CRS or after CRS resolution. Monitor for neurologic toxicities
after treatment with Tecartus. Provide supportive care and/or
corticosteroids as needed.
- T cell malignancies have occurred following treatment of
hematologic malignancies with BCMA- and CD19-directed genetically
modified autologous T cell immunotherapies
- Tecartus is available only through a restricted program
under a Risk Evaluation and Mitigation Strategy (REMS) called the
Yescarta and Tecartus REMS Program.
Cytokine Release Syndrome (CRS), including
life-threatening reactions, occurred following treatment with
Tecartus. CRS occurred in 92% (72/78) of patients with ALL,
including ≥ Grade 3 (Lee grading system) CRS in 26% of patients.
Three patients with ALL had ongoing CRS events at the time of
death. The median time to onset of CRS was five days (range: 1 to
12 days) and the median duration of CRS was eight days (range: 2 to
63 days) for patients with ALL.
Ensure that a minimum of two doses of tocilizumab are available
for each patient prior to infusion of Tecartus. Following infusion,
monitor patients for signs and symptoms of CRS daily for at least
seven days at the certified healthcare facility, and for four weeks
thereafter. Counsel patients to seek immediate medical attention
should signs or symptoms of CRS occur at any time. At the first
sign of CRS, institute treatment with supportive care, tocilizumab,
or tocilizumab and corticosteroids as indicated.
Neurologic Events, including those that were fatal or
life-threatening, occurred following treatment with Tecartus.
Neurologic events occurred in 87% (68/78) of patients with ALL,
including ≥ Grade 3 in 35% of patients. The median time to onset
for neurologic events was seven days (range: 1 to 51 days) with a
median duration of 15 days (range: 1 to 397 days) in patients with
ALL. For patients with MCL, 54 (66%) patients experienced CRS
before the onset of neurological events. Five (6%) patients did not
experience CRS with neurologic events and eight patients (10%)
developed neurological events after the resolution of CRS.
Neurologic events resolved for 119 out of 134 (89%) patients
treated with Tecartus. Nine patients (three patients with MCL and
six patients with ALL) had ongoing neurologic events at the time of
death. For patients with ALL, neurologic events occurred before,
during, and after CRS in 4 (5%), 57 (73%), and 8 (10%) of patients;
respectively. Three patients (4%) had neurologic events without
CRS. The onset of neurologic events can be concurrent with CRS,
following resolution of CRS or in the absence of CRS.
The most common neurologic events (>10%) were similar in MCL
and ALL and included encephalopathy (57%), headache (37%), tremor
(34%), confusional state (26%), aphasia (23%), delirium (17%),
dizziness (15%), anxiety (14%), and agitation (12%). Serious events
including encephalopathy, aphasia, confusional state, and seizures
occurred after treatment with Tecartus.
Monitor patients daily for at least seven days for patients with
MCL and at least 14 days for patients with ALL at the certified
healthcare facility and for four weeks following infusion for signs
and symptoms of neurologic toxicities and treat promptly.
REMS Program: Because of the risk of CRS and neurologic
toxicities, Tecartus is available only through a restricted program
under a Risk Evaluation and Mitigation Strategy (REMS) called the
Yescarta and Tecartus REMS Program which requires that:
- Healthcare facilities that dispense and administer Tecartus
must be enrolled and comply with the REMS requirements. Certified
healthcare facilities must have on-site, immediate access to
tocilizumab, and ensure that a minimum of two doses of tocilizumab
are available for each patient for infusion within two hours after
Tecartus infusion, if needed for treatment of CRS.
- Certified healthcare facilities must ensure that healthcare
providers who prescribe, dispense, or administer Tecartus are
trained in the management of CRS and neurologic toxicities. Further
information is available at www.YescartaTecartusREMS.com or
1-844-454-KITE (5483).
Hypersensitivity Reactions: Serious hypersensitivity
reactions, including anaphylaxis, may occur due to dimethyl
sulfoxide (DMSO) or residual gentamicin in Tecartus.
Severe Infections: Severe or life-threatening infections
occurred in patients after Tecartus infusion. Infections (all
grades) occurred in 56% (46/82) of patients with MCL and 44%
(34/78) of patients with ALL. Grade 3 or higher infections,
including bacterial, viral, and fungal infections, occurred in 30%
of patients with ALL and MCL. Tecartus should not be administered
to patients with clinically significant active systemic infections.
Monitor patients for signs and symptoms of infection before and
after Tecartus infusion and treat appropriately. Administer
prophylactic antimicrobials according to local guidelines.
Febrile neutropenia was observed in 6% of patients with MCL and
35% of patients with ALL after Tecartus infusion and may be
concurrent with CRS. The febrile neutropenia in 27 (35%) of
patients with ALL includes events of “febrile neutropenia” (11
(14%)) plus the concurrent events of “fever” and “neutropenia” (16
(21%)). In the event of febrile neutropenia, evaluate for infection
and manage with broad spectrum antibiotics, fluids, and other
supportive care as medically indicated.
In immunosuppressed patients, life-threatening and fatal
opportunistic infections have been reported. The possibility of
rare infectious etiologies (e.g., fungal and viral infections such
as HHV-6 and progressive multifocal leukoencephalopathy) should be
considered in patients with neurologic events and appropriate
diagnostic evaluations should be performed.
Hepatitis B virus (HBV) reactivation, in some cases resulting in
fulminant hepatitis, hepatic failure, and death, can occur in
patients treated with drugs directed against B cells. Perform
screening for HBV, HCV, and HIV in accordance with clinical
guidelines before collection of cells for manufacturing.
Prolonged Cytopenias: Patients may exhibit cytopenias for
several weeks following lymphodepleting chemotherapy and Tecartus
infusion. In patients with MCL, Grade 3 or higher cytopenias not
resolved by Day 30 following Tecartus infusion occurred in 55%
(45/82) of patients and included thrombocytopenia (38%),
neutropenia (37%), and anemia (17%). In patients with ALL who were
responders to Tecartus treatment, Grade 3 or higher cytopenias not
resolved by Day 30 following Tecartus infusion occurred in 20%
(7/35) of the patients and included neutropenia (12%) and
thrombocytopenia (12%); Grade 3 or higher cytopenias not resolved
by Day 60 following Tecartus infusion occurred in 11% (4/35) of the
patients and included neutropenia (9%) and thrombocytopenia (6%).
Monitor blood counts after Tecartus infusion.
Hypogammaglobulinemia: B cell aplasia and
hypogammaglobulinemia can occur in patients receiving treatment
with Tecartus. Hypogammaglobulinemia was reported in 16% (13/82) of
patients with MCL and 9% (7/78) of patients with ALL. Monitor
immunoglobulin levels after treatment with Tecartus and manage
using infection precautions, antibiotic prophylaxis, and
immunoglobulin replacement.
The safety of immunization with live viral vaccines during or
following Tecartus treatment has not been studied. Vaccination with
live virus vaccines is not recommended for at least six weeks prior
to the start of lymphodepleting chemotherapy, during Tecartus
treatment, and until immune recovery following treatment with
Tecartus.
Secondary Malignancies may develop. T cell malignancies
have occurred following treatment of hematologic malignancies with
BCMA- and CD19-directed genetically modified autologous T cell
immunotherapies. Mature T cell malignancies, including CAR-positive
tumors, may present as soon as weeks following infusion, and may
include fatal outcomes. Monitor life-long for secondary
malignancies. In the event that one occurs, contact Kite at
1-844-454-KITE (5483) to obtain instructions on patient samples to
collect for testing.
Effects on Ability to Drive and Use Machines: Due to the
potential for neurologic events, including altered mental status or
seizures, patients are at risk for altered or decreased
consciousness or coordination in the 8 weeks following Tecartus
infusion. Advise patients to refrain from driving and engaging in
hazardous activities, such as operating heavy or potentially
dangerous machinery, during this period.
Adverse Reactions: The most common non-laboratory adverse
reactions (≥ 20%) were fever, cytokine release syndrome,
hypotension, encephalopathy, tachycardia, nausea, chills, headache,
fatigue, febrile neutropenia, diarrhea, musculoskeletal pain,
hypoxia, rash, edema, tremor, infection with pathogen unspecified,
constipation, decreased appetite, and vomiting. The most common
serious adverse reactions (≥ 2%) were cytokine release syndrome,
febrile neutropenia, hypotension, encephalopathy, fever, infection
with pathogen unspecified, hypoxia, tachycardia, bacterial
infections, respiratory failure, seizure, diarrhea, dyspnea, fungal
infections, viral infections, coagulopathy, delirium, fatigue,
hemophagocytic lymphohistiocytosis, musculoskeletal pain, edema,
and paraparesis.
Please see full Prescribing Information, including BOXED
WARNING and Medication Guide.
About Kite
Kite, a Gilead Company, is a global biopharmaceutical company
based in Santa Monica, California, focused on cell therapy to treat
and cure cancer. As the global cell therapy leader, Kite has
treated more patients with CAR T-cell therapy than any other
company. Kite has the largest in-house cell therapy manufacturing
network in the world, spanning process development, vector
manufacturing, clinical trial supply and commercial product
manufacturing. For more information on Kite, please visit
www.kitepharma.com.
About Gilead Sciences
Gilead Sciences, Inc. is a biopharmaceutical company that has
pursued and achieved breakthroughs in medicine for more than three
decades, with the goal of creating a healthier world for all
people. The company is committed to advancing innovative medicines
to prevent and treat life-threatening diseases, including HIV,
viral hepatitis, COVID-19, cancer, and inflammation. Gilead
operates in more than 35 countries worldwide, with headquarters in
Foster City, Calif. Gilead acquired Kite in 2017.
About Arcellx and Kite
Collaboration
Arcellx and Kite, a Gilead Company, formed a global strategic
collaboration and license agreement to co-develop and
co-commercialize anito-cel for patients with relapsed or refractory
multiple myeloma, RRMM. Anito-cel is currently being developed in a
Phase 2 registrational pivotal study and a Phase 3 randomized
controlled study for RRMM. Kite and Arcellx will jointly
commercialize the anito-cel asset in the United States, and Kite
will commercialize the product outside the United States.
About Anitocabtagene autoleucel
(anito-cel)
Anitocabtagene autoleucel (anito-cel, previously CART-ddBCMA) is
the first BCMA-directed CAR T-cell therapy to be investigated in
multiple myeloma that utilizes Arcellx’s novel and compact binder
known as the D-Domain. Anito-cel has been granted Fast Track,
Orphan Drug, and Regenerative Medicine Advanced Therapy
Designations by the U.S. Food and Drug Administration.
About iMMagine-3 Global Phase 3
Randomized Controlled Clinical Study
iMMagine-3 is a global Phase 3, randomized controlled study
designed to compare the efficacy and safety of anitocabtagene
autoleucel (anito-cel) with standard of care (SOC) in patients with
relapsed and/or refractory multiple myeloma (RRMM) who have
received one to three prior lines of therapy, including an
immunomodulatory drug (lMiD) and an anti-CD38 monoclonal
antibody.
iMMagine-3 will enroll approximately 450 adult patients. Prior
to randomization, investigator’s choice of SOC regimens include:
pomalidomide, bortezomib, and dexamethasone (PVd); daratumumab,
pomalidomide, and dexamethasone (DPd); carfilzomib, daratumumab and
dexamethasone (KDd); or carfilzomib and dexamethasone (Kd).
Patients in the anito-cel arm will undergo leukapheresis and
optional bridging therapy (with the SOC regimen selected by the
investigator prior to randomization) followed by lymphodepleting
chemotherapy (fludarabine 30 mg/m2/d and cyclophosphamide 300
mg/m2/d for 3 days) and one infusion of anito-cel (115×106 CAR+ T
cells) on Day 1.
The primary endpoint is progression free survival (PFS) per
blinded independent review according to the 2016 IMWG uniform
response criteria for MM with the hypothesis that anito-cel will
prolong PFS compared to SOC. Key secondary endpoints include
complete response rate (CR/sCR), minimal residual disease
negativity, overall survival, and safety.
The iMMagine-3 study initiated in the second half of 2024 at
approximately 130 study sites across North America, Europe, and
rest of world.
Forward-Looking
Statements
This press release includes forward-looking statements, within
the meaning of the Private Securities Litigation Reform Act of 1995
that are subject to risks, uncertainties and other factors,
including the ability of Gilead and Kite to initiate, progress or
complete clinical trials within currently anticipated timelines or
at all, and the possibility of unfavorable results from ongoing or
additional clinical studies, including those involving Tecartus,
Yescarta anito-cel and KITE-753 (such as iMMagine-1, ZUMA-2, ZUMA-3
and ZUMA-5); uncertainties relating to regulatory applications and
related filing and approval timelines, including pending or
potential applications for indications currently under evaluation;
the possibility that Gilead and Kite may make a strategic decision
to discontinue development of these programs and, as a result,
these programs may never be successfully commercialized for the
indications currently under evaluation; and any assumptions
underlying any of the foregoing. These and other risks,
uncertainties and other factors are described in detail in Gilead’s
Quarterly Report on Form 10-Q for the quarter ended June 30, 2024,
as filed with the U.S. Securities and Exchange Commission. These
risks, uncertainties and other factors could cause actual results
to differ materially from those referred to in the forward-looking
statements. All statements other than statements of historical fact
are statements that could be deemed forward-looking statements. The
reader is cautioned that any such forward-looking statements are
not guarantees of future performance and involve risks and
uncertainties and is cautioned not to place undue reliance on these
forward-looking statements. All forward-looking statements are
based on information currently available to Gilead and Kite, and
Gilead and Kite assume no obligation and disclaim any intent to
update any such forward-looking statements.
Tecartus, Yescarta, Gilead, the Gilead logo,
Kite, the Kite logo are trademarks of Gilead Sciences, Inc., or its
related companies.
For more information on Kite, please visit the
company’s website at www.kitepharma.com. Follow Kite on social
media on X (@KitePharma) and LinkedIn.
View source
version on businesswire.com: https://www.businesswire.com/news/home/20241105435302/en/
Meaghan Smith, Gilead Media public_affairs@gilead.com
Jacquie Ross, Investors investor_relations@gilead.com
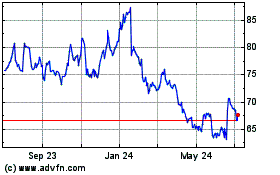
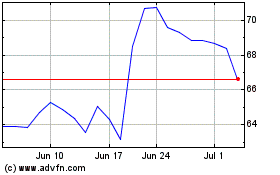
Gilead Sciences (NASDAQ:GILD)
Historical Stock Chart
From Oct 2024 to Nov 2024
Gilead Sciences (NASDAQ:GILD)
Historical Stock Chart
From Nov 2023 to Nov 2024