Centene Corporation (NYSE: CNC) today announced its net earnings
from continuing operations for the quarter ended March 31, 2009
were $18.9 million, or $0.43 per diluted share, compared to $24.9
million, or $0.56 per diluted share in the 2008 first quarter. The
prior year first quarter results include the benefit of the July 1
through December 31, 2007 rate increase for Georgia, amounting to
$12.6 million of earnings from continuing operations or $0.28 per
diluted share. The results of operations for University Health
Plans, or UHP, our New Jersey health plan, are classified as
discontinued operations. Unless specifically noted, the discussions
below are in the context of continuing operations and all financial
ratios are calculated using revenues excluding premium taxes and
investment income.
First Quarter Highlights
- Quarter-end managed care at-risk
membership of 1.25 million.
- Revenues of $932.4 million, or
$908.9 million net of premium taxes.
- Health Benefits Ratio (HBR),
which reflects medical costs as a percent of premium revenues, of
83.5%.
- General and administrative
(G&A) expense ratio of 13.5%.
- Cash flow from operations of
$23.4 million.
- Days in claims payable of
45.3.
- Diluted earnings per share from
continuing operations of $0.43.
Other Events
- In February 2009, we began
converting�non-risk managed care membership in Florida from Access
Health Solutions, LLC, or Access, to our wholly owned subsidiary,
Sunshine State Health Plan on an at-risk basis. We previously
accounted for our Florida investment using the equity method of
accounting. Beginning with the first quarter of 2009, we have
reported our investment in Access as a consolidated subsidiary in
our financial statements.
- In March 2009, we completed the
previously announced acquisition of certain assets of Amerigroup
Community Care of South Carolina.
- In March 2009,
our�Celtic�unit�was awarded�a contract in Massachusetts
to�serve�uninsured�individuals through a joint venture with�a
leading, local provider, Caritas Christi Health Care.�Effective
July 1, 2009, the joint venture will serve the Central, Northern,
Boston and Southern regions operating as CeltiCare Health Plan of
Massachusetts.
- We were awarded Silver Honors
for Best Practices in Health Management by URAC, a leading
healthcare accreditation organization, for Connections PLUS, a
free, pre-programmed cell phone program developed for high-risk
members who do not have steady access to a telephone.
Michael F. Neidorff, Centene�s Chairman and Chief Executive
Officer, stated, �Our first quarter results reflect favorably on
our�focus on fundamentals and teamwork. We will continue to work to
maintain this momentum going forward.�
The following table depicts membership in Centene�s managed care
organizations, by state, at March 31, 2009 and 2008:
� �
March 31, 2009 � �
2008 Arizona 15,500 �
Florida 29,100 � Georgia 289,300 282,700 Indiana 179,100 161,300
Ohio 137,000 131,100 South Carolina 48,500 2,200 Texas 421,100
365,500 Wisconsin 127,700 126,900 Total at-risk membership
1,247,300 1,069,700 Non-risk membership 96,000 30,600 Total
1,343,300 1,100,300
The following table depicts membership in Centene�s managed care
organizations, by member category, at March 31, 2009 and 2008:
� �
March 31, 2009 � �
2008 Medicaid 921,100
802,400 CHIP & Foster Care 256,900 206,300 ABD & Medicare
69,300 61,000
Total at-risk membership
1,247,300 1,069,700 Non-risk membership 96,000 30,600 Total
1,343,300 1,100,300
Statement of Operations
- For the 2009 first quarter,
revenues, net of premium taxes, increased 20.0% to $908.9 million
from $757.3 million in the 2008 first quarter. The increase was
primarily driven by membership growth, especially related to the
Foster Care contract in Texas, the commencement of our Arizona
acute care contract in October 2008, the consolidation of Access
and conversion of members to at-risk, premium rate increases and
the recent acquisition of Celtic in July 2008.
- The consolidated HBR, which
reflects medical costs as a percent of premium revenues, was 83.5%,
an increase from 82.7% in the 2008 first quarter. The retroactive
Georgia premium rate increase in the first quarter of 2008 had the
effect of decreasing the HBR for this period by 2.4%. Adjusting for
the impact due to the Georgia rate increase, our HBR decreased from
85.1% in 2008 to 83.5% in 2009. This is due to a decrease in
respiratory illness as a result of a lighter cold and flu season.
Sequentially, our consolidated HBR increased from 82.3% in the 2008
fourth quarter to 83.5% as a result of normal seasonality and the
addition of a new state and acquired members.
- Consolidated G&A expense as
a percent of premium and service revenues was 13.5% in the first
quarter of 2009, an increase from 12.6% in the first quarter of
2008. The retroactive Georgia premium rate increase in the first
quarter of 2008 had the effect of decreasing the G&A ratio for
this period by 0.4%. Adjusting for the impact due to the Georgia
rate increase, our G&A expense ratio increased from 13.0% in
2008 to 13.5% in 2009. G&A increased in the quarter ended March
31, 2009 compared to 2008 primarily due to the acquisition of
Celtic. Sequentially, our G&A ratio decreased from 13.8% in the
fourth quarter of 2008 to 13.5% in the first quarter of 2009.
Balance Sheet and Cash Flow
At March 31, 2009, the Company had cash and investments of
$845.7 million, including $816.8 million held by its regulated
entities and $28.9 million held by its unregulated entities.
Medical claims liabilities totaled $372.5 million, representing
45.3 days in claims payable, a decrease of 3.2 days from December
31, 2008. Total debt was $290.3 million and debt to capitalization
was 34.6%. Year to date cash flow from operations was $23.4
million.
A reconciliation of the Company�s change in days in claims
payable from the immediately preceding quarter-end is presented
below:
Days in claims payable, December 31, 2008 � � 48.5 Timing of claims
payments (1.4 ) Change in medical cost mix (1.0 ) High dollar
claims inventory reduction (0.7 ) Other (0.1 ) Days in claims
payable, March 31, 2009 * 45.3 �
* The Company has used a
consistent and conservative actuarial reserving methodology and the
decline in days in claims payable was not the result of a reserve
release.
Outlook
The table below depicts the Company�s annual guidance for
2009:
� �
Full Year 2009 Low � �
High Revenue (in
millions)1 $ 3,650 $ 3,775 Earnings per diluted share $ 1.84 $ 1.94
�
1 Revenue net of premium tax
The Company is adjusting the lower end of its earnings guidance
to reflect a lower effective tax rate which is partially offset by
the startup costs associated with the new Massachusetts CeltiCare
contract that commences July 1, 2009.
Conference Call
As previously announced, the Company will host a conference call
Tuesday, April 28, 2009, at 8:30 A.M. (Eastern Time) to review the
financial results for the first quarter ended March 31, 2009, and
to discuss its business outlook. Michael F. Neidorff and Eric R.
Slusser will host the conference call. Investors are invited to
participate in the conference call by dialing 800-273-1254 in the
U.S. and Canada, 973-638-3440 from abroad, or via a live internet
broadcast on the Company�s website at www.centene.com, under the
Investor Relations section. A replay will be available for
on-demand listening shortly after the completion of the call until
11:59 P.M. (Eastern Time) on May 12, 2009 at the aforementioned
URL, or by dialing 800-642-1687 in the U.S. and Canada, or
706-645-9291 from abroad, and entering access code 93132567.
About Centene Corporation
Centene Corporation is a leading multi-line healthcare
enterprise that provides programs and related services to
individuals receiving benefits under Medicaid, including the
Children�s Health Insurance Program (CHIP), as well as Aged, Blind,
or Disabled (ABD), Foster Care, Long-Term Care and Medicare
(Special Needs Plans). The Company operates local health plans and
offers a wide range of health insurance solutions to individuals
and the rising number of uninsured Americans. It also contracts
with other healthcare and commercial organizations to provide
specialty services including behavioral health, life and health
management, managed vision, telehealth services, pharmacy benefits
management and medication adherence. Information regarding Centene
is available via the Internet at www.centene.com.
The information provided in this press release contains
forward-looking statements that relate to future events and future
financial performance of Centene. Subsequent events and
developments may cause the Company�s estimates to change. The
Company disclaims any obligation to update this forward-looking
financial information in the future. Readers are cautioned that
matters subject to forward-looking statements involve known and
unknown risks and uncertainties, including economic, regulatory,
competitive and other factors that may cause Centene�s or its
industry�s actual results, levels of activity, performance or
achievements to be materially different from any future results,
levels of activity, performance or achievements expressed or
implied by these forward-looking statements. Actual results may
differ from projections or estimates due to a variety of important
factors, including Centene�s ability to accurately predict and
effectively manage health benefits and other operating expenses,
competition, changes in healthcare practices, changes in federal or
state laws or regulations, inflation, provider contract changes,
new technologies, reduction in provider payments by governmental
payors, major epidemics, disasters and numerous other factors
affecting the delivery and cost of healthcare. The expiration,
cancellation or suspension of Centene�s Medicaid Managed Care
contracts by state governments would also negatively affect
Centene.
�
CENTENE CORPORATION AND
SUBSIDIARIES
�
CONSOLIDATED BALANCE
SHEETS
(In thousands, except share
data)
� � �
March 31,
2009
� �
December 31,
2008
(Unaudited) ASSETS Current assets: Cash and cash
equivalents of continuing operations $ 334,623 $ 370,999 Cash and
cash equivalents of discontinued operations � 7,606 � 8,100 Total
cash and cash equivalents 342,229 379,099 Premium and related
receivables, net of allowance for uncollectible accounts of $138
and $595, respectively 147,899 92,531 Short-term investments, at
fair value (amortized cost $74,780 and $108,469, respectively)
75,400 109,393 Other current assets 63,497 75,333 Current assets of
discontinued operations other than cash � 8,226 � 9,987 Total
current assets 637,251 666,343 Long-term investments, at fair value
(amortized cost $416,265 and $329,330, respectively) 422,873
332,411 Restricted deposits, at fair value (amortized cost $12,660
and $9,124, respectively) 12,774 9,254 Property, software and
equipment, net of accumulated depreciation of $80,742 and $74,194,
respectively 176,719 175,858 Goodwill 218,216 163,380 Intangible
assets, net 23,603 17,575 Other long-term assets 34,077 59,083
Long-term assets of discontinued operations � 27,317 � 27,248 Total
assets $ 1,552,830 $ 1,451,152
LIABILITIES AND STOCKHOLDERS�
EQUITY Current liabilities: Medical claims liability $ 372,522
$ 373,037 Accounts payable and accrued expenses 194,132 219,566
Unearned revenue 63,336 17,107 Current portion of long-term debt
20,608 255 Current liabilities of discontinued operations � 30,865
� 31,013 Total current liabilities 681,463 640,978 Long-term debt
269,711 264,637 Other long-term liabilities 51,434 43,539 Long-term
liabilities of discontinued operations � 700 � 726 Total
liabilities 1,003,308 949,880 � Commitments and contingencies �
Stockholders� equity: Common stock, $.001 par value; authorized
100,000,000 shares; issued and outstanding 43,159,131 and
42,987,764 shares, respectively 43 43 Additional paid-in capital
227,327 222,841 Accumulated other comprehensive income: Unrealized
gain on investments, net of tax 5,136 3,152 Retained earnings �
293,694 � 275,236 Total Centene stockholder�s equity 526,200
501,272 Non-controlling interest � 23,322 � � Total stockholders�
equity � 549,522 � 501,272 Total liabilities and stockholders�
equity $ 1,552,830 $ 1,451,152 �
CENTENE CORPORATION AND
SUBSIDIARIES
�
CONSOLIDATED STATEMENTS OF
OPERATIONS
(In thousands, except share
data)
� � �
Three Months Ended
March 31,
2009 � �
2008 (Unaudited) Revenues:
Premium $ 885,006 $ 736,814 Premium tax 23,580 21,884 Service �
23,849 � � 20,530 � Total revenues � 932,435 � � 779,228 �
Expenses: Medical costs 739,340 609,374 Cost of services
15,962 16,176 General and administrative expenses 122,279 95,493
Premium tax � 23,942 � � 21,884 � Total operating expenses �
901,523 � � 742,927 � Earnings from operations 30,912 36,301
Other income (expense): Investment and other income 3,613
7,582 Interest expense � (3,986 ) � (3,994 ) Earnings from
continuing operations, before income tax expense 30,539 39,889
Income tax expense � 10,845 � � 14,956 � Earnings from
continuing operations, net of income tax expense 19,694 24,933
Discontinued operations, net of income tax (benefit) expense of
$(160) and $264 � (449 ) � 690 � Net earnings 19,245 25,623
Less: Non-controlling interest � 787 � ?
Net earnings
attributable to Centene Corporation $ 18,458 � $ 25,623 � �
Amounts attributable to Centene Corporation common
shareholders: Earnings from continuing operations, net of
income tax expense 18,907 24,933 Discontinued operations, net of
income tax (benefit) expense � (449 ) � 690 � Net earnings $ 18,458
� $ 25,623 � �
Net earnings (loss) per share attributable to
Centene Corporation: Basic: Continuing operations $ 0.44 $ 0.57
Discontinued operations � (0.01 ) � 0.02 � Earnings per common
share $ 0.43 � $ 0.59 � Diluted: Continuing operations $ 0.43 $
0.56 Discontinued operations � (0.01 ) � 0.01 � Earnings per common
share $ 0.42 � $ 0.57 � �
Weighted average number of shares
outstanding: Basic 43,067,992 43,538,207 Diluted 44,238,863
44,742,893 �
CENTENE CORPORATION AND
SUBSIDIARIES
�
CONSOLIDATED STATEMENTS OF CASH
FLOWS
(In thousands)
� � �
Three Months Ended March 31, 2009 � �
2008 (Unaudited) �
Cash flows from operating
activities: Net earnings $ 19,245 $ 25,623 Adjustments to
reconcile net earnings to net cash provided by operating activities
Depreciation and amortization 10,233 7,798 Stock compensation
expense 3,789 4,013 Loss on sale of investments, net 439 28
Deferred income taxes 2,282 9,472 Changes in assets and liabilities
� Premium and related receivables (39,396 ) 8,612 Other current
assets (1,397 ) (2,634 ) Other assets (497 ) (1,031 ) Medical
claims liabilities (1,232 ) 11,608 Unearned revenue 44,507 (41,788
) Accounts payable and accrued expenses (15,277 ) 4,489 Other
operating activities � 722 � � 526 � Net cash provided by operating
activities � 23,418 � � 26,716 �
Cash flows from investing
activities: Capital expenditures (11,157 ) (19,879 ) Purchases
of investments (292,964 ) (86,025 ) Sales and maturities of
investments 224,312 70,888 Investments in acquisitions, net of cash
acquired, and investment in equity method investee � (5,191 ) �
(2,194 ) Net cash used in investing activities � (85,000 ) �
(37,210 )
Cash flows from financing activities: Proceeds
from exercise of stock options 890 1,148 Proceeds from borrowings
108,000 26,005 Payment of long-term debt (82,573 ) (17,148 )
Dividend to non-controlling interest (1,181 ) ? Excess tax benefits
from stock compensation (17 ) 2,638 Common stock repurchases � (407
) � (6,953 ) Net cash provided by financing activities � 24,712 � �
5,690 � Net decrease in cash and cash equivalents � (36,870 ) �
(4,804 )
Cash and cash equivalents, beginning of period �
379,099 � � 268,584 �
Cash and cash equivalents, end of
period $ 342,229 � $ 263,780 � � Supplemental disclosures of cash
flow information: Interest paid $ 724 $ 463 Income taxes paid $
18,602 $ 792 �
CENTENE CORPORATION
�
CONTINUING OPERATIONS
SUPPLEMENTAL FINANCIAL DATA
� � �
Q1 � �
Q4 � �
Q3 � �
Q2 � �
Q1 2009 2008 2008 2008
2008 MEMBERSHIP Managed Care: Arizona 15,500 14,900 �
� � Florida 29,100 � � � � Georgia 289,300 288,300 283,900 278,800
282,700 Indiana 179,100 175,300 172,400 161,700 161,300 Ohio
137,000 133,400 132,500 137,300 131,100 South Carolina 48,500
31,300 26,600 22,500 2,200 Texas 421,100 428,000 433,200 423,700
365,500 Wisconsin � 127,700 � � 124,800 � � 122,500 � � 124,800 � �
126,900 � Total at-risk membership � 1,247,300 � � 1,196,000 � �
1,171,100 � � 1,148,800 � � 1,069,700 � Non-risk membership �
96,000 � � 3,700 � � 3,700 � � 3,500 � � 30,600 �
TOTAL �
1,343,300 � �
1,199,700 � �
1,174,800 � �
1,152,300 � �
1,100,300 � � Medicaid 921,100 877,400
850,500 828,700 802,400 SCHIP & Foster Care 256,900 257,300
261,800 256,900 206,300 ABD & Medicare � 69,300 � � 61,300 � �
58,800 � � 63,200 � � 61,000 � Total at-risk membership � 1,247,300
� � 1,196,000 � � 1,171,100 � � 1,148,800 � � 1,069,700 � Non-risk
membership � 96,000 � � 3,700 � � 3,700 � � 3,500 � � 30,600 �
TOTAL �
1,343,300 � �
1,199,700 � �
1,174,800 � �
1,152,300 � �
1,100,300 � �
Specialty Services(a): Cenpatico Behavioral Health Arizona 104,700
105,000 102,400 99,400 97,900 Kansas 40,600 41,100 40,100 40,000
39,400 Bridgeway Health Solutions Long-term Care � 2,300 � � 2,100
� � 1,900 � � 1,800 � � 1,700 �
TOTAL �
147,600 � �
148,200 � �
144,400 � �
141,200 � �
139,000 � �
(a) Includes external Specialty
Service membership only.
�
REVENUE PER MEMBER(b) $ 220.29 $ 218.52 $ 213.28 $
214.76 $ 215.39 �
CLAIMS(b) Period-end inventory
325,000
�
269,300
�
323,200
�
389,100
�
411,700
�
Average inventory 267,600 288,600 298,400 235,300 285,700
Period-end inventory per member 0.26 0.23 0.28 0.34 0.37 �
(b) Revenue per member and claims
information are presented for the Medicaid Managed Care segment for
at-risk members.
� �
Q1 � �
Q4 � �
Q3 � �
Q2 � �
Q1 2009 2008 2008 2008
2008 �
DAYS IN CLAIMS
PAYABLE(c)
45.3 48.5 47.9 47.8 48.3 � (c) Days in Claims Payable is a
calculation of Medical Claims Liabilities at the end of the period
divided by average claims expense per calendar day for such period.
�
CASH AND INVESTMENTS (in millions) Regulated $ 816.8 $
798.0 $ 692.6 $ 653.1 $ 627.1 Unregulated � 28.9 � � 24.1 � � 26.8
� � 29.0 � � 25.8 �
TOTAL $ 845.7 � $ 822.1 � $ 719.4 � $
682.1 � $ 652.9 � �
DEBT TO
CAPITALIZATION(d)
34.6 % 34.6 % 34.4 % 32.6 % 32.8 % � (d) Debt to Capitalization is
calculated as follows: total debt divided by (total debt + total
equity). �
OPERATING RATIOS:
� � �
Three Months Ended
March 31,
2009 � �
2008 Health Benefits Ratios Medicaid and
SCHIP 84.8 % 79.2 % ABD and Medicare 81.4 97.5 Specialty Services
78.3 84.1 Total 83.5 82.7 � General & Administrative Expense
Ratios Medicaid Managed Care 10.3 % 9.9 % Specialty Services 15.7
14.9 Total 13.5 12.6 �
MEDICAL CLAIMS LIABILITIES (In
thousands) Four rolling quarters of the changes in medical
claims liabilities are summarized as follows: �
Balance, March 31, 2008 � � $ 323,302 Acquisitions 15,398
Incurred related to: Current period 2,793,935 Prior period �
(23,634 ) Total incurred � 2,770,301 � Paid related to: Current
period 2,448,657 Prior period � 287,822 � Total paid � 2,736,479 �
Balance, March 31, 2009 $ 372,522 �
Centene�s claims reserving process utilizes a consistent
actuarial methodology to estimate Centene�s ultimate liability. Any
reduction in the �Incurred related to: Prior period� claims may be
offset as Centene actuarially determines �Incurred related to:
Current period.� As such, only in the absence of a consistent
reserving methodology would favorable development of prior period
claims liability estimates reduce medical costs. Centene believes
it has consistently applied its claims reserving methodology in
each of the periods presented.
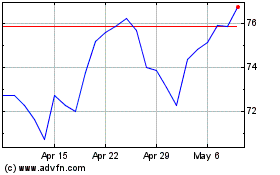
Centene (NYSE:CNC)
Historical Stock Chart
From Jun 2024 to Jul 2024
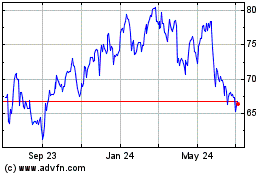
Centene (NYSE:CNC)
Historical Stock Chart
From Jul 2023 to Jul 2024