Centene Corporation (NYSE: CNC) today announced its financial
results for the quarter ended June 30, 2007. The revenues, general
and administrative expenses and related financial ratios included
in this release present premium taxes on a gross basis consistent
with our past reporting practice. � Q2 2007 Highlights Total
Revenues (in millions) $ 727.7 Medicaid/SCHIP HBR 80.6 % Diluted
EPS (as reported) $ 0.40 Diluted EPS excluding FirstGuard activity
� $ 0.27 � Second Quarter Summary Quarter-end Medicaid Managed Care
membership of 1.1 million Revenues of $727.7 million, a 46.9%
increase over the 2006 second quarter. Earnings per diluted share
of $0.27, excluding FirstGuard activity, compared to $0.11 in the
2006 second quarter. Health Benefits Ratio (HBR) for Centene�s
Medicaid and SCHIP populations, which reflects medical costs as a
percent of premium revenues, of 80.6%. Medicaid Managed Care
G&A expense ratio of 14.0% and Specialty Services G&A ratio
of 15.8%. Operating cash flows of $23.9 million. Days in claims
payable of 46.8. Other Events In April 2007, we acquired PhyTrust
of South Carolina, a physician-driven company that served over
31,100 members at June 30, 2007. In July 2007, we acquired a
minority interest in Access Health Solutions, LLC (Access), the
third largest Medicaid managed care entity in Florida. Access
currently serves approximately 90,000 members. Michael F. Neidorff,
Centene�s Chairman and Chief Executive Officer, stated, �During the
second quarter, overall results for revenue, membership growth and
earnings were consistent with our expectations, and our Medicaid
and SCHIP HBR improved by 170 basis points sequentially. �In Texas,
we continue to see growing membership in both SCHIP and SSI, with
the Texas STAR Plus overall membership consistent with our
expectations. To date, we have 31,400 Star Plus members under
management. Recently, the state of Texas indicated its intent to
delay the implementation of the Foster Care contract award, which
we won in March. We now expect operations to commence in 2008. The
state is currently working on its readiness review and we are
supporting them in this process. We remain confident that our
technology platform will enable us to provide the state more
effective tracking of these members and offer a more consistent
quality of healthcare for the recipients. �In Georgia, membership
was 281,400, within our guided range. While cost and utilization
trends in the state are high, we began to see those trends moderate
later in the quarter. We expect trends to continue to moderate as
our medical management initiatives take hold and have implemented
margin protection initiatives effective August 1 with the state.
�We will continue to focus our efforts on opportunities to
effectively manage our costs as we build the business. There remain
numerous avenues to grow on a sustainable basis in Medicaid managed
care.� concluded Neidorff. The following table depicts membership
in Centene�s managed care organizations by state at June 30, 2007
and 2006: � 2007 2006 Georgia 281,400 216,000 Indiana 161,700
193,000 New Jersey 59,100 59,000 Ohio 128,200 73,100 South Carolina
31,100 � Texas 333,900 235,800 Wisconsin 136,100 174,600 Subtotal
1,131,500 951,500 � Kansas and Missouri � 150,000 Total 1,131,500
1,101,500 The following table depicts membership in Centene�s
managed care organizations by member category at June 30, 2007 and
2006: � 2007 2006 Medicaid 846,900 755,400 SCHIP 216,500 179,700
SSI � 68,100 (a) � 16,400 (b) Subtotal 1,131,500 951,500 � Kansas
and Missouri Medicaid/SCHIP members � � � 150,000 Total � 1,131,500
� 1,101,500 � (a) 64,000 at-risk; 4,100 ASO (b) 8,900 at-risk;
7,500 ASO � � � � � � � Statement of Operations For the 2007 second
quarter, revenues increased 46.9% to $727.7 million from $495.3
million in the 2006 second quarter. The HBR for Centene�s Medicaid
and SCHIP populations, which reflects medical costs as a percent of
premium revenues, was 80.6%, a decrease of 3.4% over 2006. The HBR
for the three months ended June 30, 2006, includes approximately
2.2% ($9.7 million) for adverse medical cost development in
estimated medical claims liabilities from the first quarter of
2006. The decrease in the current year is primarily attributable to
the adverse development in the prior year and increased premium
taxes. Sequentially, our Medicaid and SCHIP HBR decreased from
82.3% in the 2007 first quarter to 80.6% because of decreases in
our Indiana, Texas, and Wisconsin markets, primarily related to
inpatient and pharmacy cost trends. The 2007 second quarter
reflects expected claims reserve development and is based on
consistent reserving methodology. G&A expense as a percent of
revenues for the Medicaid Managed Care segment was 14.0% in the
second quarter of 2007 compared to 12.3% in the second quarter of
2006. The increase in the Medicaid Managed Care G&A expense
ratio for the three months ended June 30, 2007 primarily reflects
increased premium taxes. Premium taxes were $19.9 million in the
2007 second quarter and $6.9 million in the 2006 second quarter.
This increase was offset by the leveraging of our expenses over
higher revenues, especially in our Georgia health plan. The second
quarter of 2006 included two months of Georgia implementation costs
for which there was no associated revenue. Operating earnings were
$16.9 million, including a $3.3 million gain on the sale of
FirstGuard Missouri and $3.4 million of net expense for other
FirstGuard activity. Excluding the gain and other FirstGuard
activity, operating earnings were $17.0 million compared to $6.3
million in the 2006 second quarter. The second quarter results
included a tax benefit from the stock abandonment of our Missouri
health plan, a gain from the sale of our Missouri health plan, a
contribution to our charitable foundation from the sale proceeds
and additional FirstGuard activity. The net effect of these
activities was $0.13 accretive to earnings per diluted share.
Earnings per diluted share of $0.40. Earnings per diluted share of
$0.27, excluding the FirstGuard activity, compared to $0.11 in the
2006 second quarter. For the six months ended June 30, 2007,
revenues increased 47.2% to $1.4 billion from $950.4 million for
the same period in the prior year. Medicaid Managed Care G&A
expenses as a percent of revenues increased to 13.5% in the first
six months of 2007 compared to 12.1% in the first six months of
2006. Earnings from operations, excluding the FirstGuard activity,
increased to $32.8 million in the first six months of 2007 from
$18.9 million in the first six months of 2006. Net earnings,
excluding the FirstGuard activity, were $23.6 million or $0.53 per
diluted share in the first six months of 2007. Balance Sheet and
Cash Flow At June 30, 2007, the Company had cash and investments of
$593.7 million, including $527.9 million held by its regulated
entities and $65.8 million held by its unregulated entities.
Medical claims liabilities totaled $295.3 million, representing
46.8 days in claims payable. Total debt was $201.1 million and debt
to capitalization was 34.0%. A reconciliation of the Company�s
change in days in claims payable from the immediately preceding
quarter-end is presented below: Days in claims payable, March 31,
2007 46.4 Remaining FirstGuard reserves 0.4 Days in claims payable,
June 30, 2007 46.8 Outlook The table below depicts the Company�s
guidance for the 2007 third quarter and full year. Q3 2007 (1) 2007
(1) Low High Low High Revenue (in millions) $ 740 $ 750 $ 2,900 $
2,940 Earnings per diluted share $ 0.35 $ 0.38 $ 1.36 $ 1.45 (1)
Excludes FirstGuard Activity � � � � � � � Eric R. Slusser,
Centene�s Chief Financial Officer, stated, �The 2007 third quarter
and full year guidance reflects continued in-range HBR performance,
reasonable rate increases, continued SSI earnings growth and
rigorous G&A focus. The tightened ranges for 2007 revenue and
earnings per share reflect the delay of the Texas Foster Care
Program from the 2007 fourth quarter to 2008.� Conference Call As
previously announced, the Company will host a conference call
Tuesday, July 24, 2007, at 8:30 A.M. (Eastern Time) to review the
financial results for the second quarter ended June 30, 2007, and
to discuss its business outlook. Michael F. Neidorff, Eric R.
Slusser and J. Per Brodin will host the conference call. Investors
are invited to participate in the conference call by dialing
800-273-1254 in the U.S. and Canada, 706-679-8592 from abroad, or
via a live internet broadcast on the Company's website at
www.centene.com, under the Investor Relations section. A replay
will be available for on-demand listening shortly after the
completion of the call until 11:59 P.M. (Eastern Time) on August 7,
2007 at the aforementioned URL, or by dialing 800-642-1687 in the
U.S. and Canada, or 706-645-9291 from abroad, and entering access
code 1100685. Non-GAAP Financial Presentation The Company is
providing certain non-GAAP financial measures in this release as
the Company believes that these figures are helpful in allowing
individuals to more accurately assess the ongoing nature of the
Company's operations and measure the Company's performance more
consistently. The non-GAAP information presented above in the
�highlights� table, third bullet under "Second Quarter Summary" and
fourth through seventh bullets under "Statement of Operations"
excludes the tax benefit related to the stock of our Kansas and
Missouri health plans and other activity for the Kansas and
Missouri health plans, collectively, FirstGuard Activity. This
exclusion has been made in the non-GAAP financial measures as
management believes that the tax benefit is an unusual event and
the Kansas and Missouri health plans are not indicative of future
company operations. The Company uses the presented non-GAAP
financial measures internally to focus management on
period-to-period changes in the Company's core business operations.
Therefore, the Company believes that this information is meaningful
in addition to the information contained in the GAAP presentation
of financial information. The presentation of this additional
non-GAAP financial information is not intended to be considered in
isolation or as a substitute for the financial information prepared
and presented in accordance with GAAP. The following table
reconciles the Company�s Statement of Operations for the second
quarter of 2007 on a GAAP basis to a non-GAAP basis. The non-GAAP
basis excludes the FirstGuard Activity (in thousands, except share
data). Three Months Ended June 30, 2007 GAAP FirstGuard Activity
Non-GAAP � Total revenues $ 727,738 $ 7 $ 727,731 Expenses: Medical
costs 574,862 (284 ) 575,146 Cost of services 16,670 � 16,760
General and administrative expenses 122,596 3,715 118,881 Gain on
sale of FirstGuard Missouri � (3,254 ) � (3,254 ) � � Total
operating expenses � 710,874 � 177 � 710,697 Earnings (loss) from
operations 16,864 (170 ) 17,034 Investment and other income, net �
1,735 � (640 ) � 2,375 Earnings (loss) before income taxes 18,599
(810 ) 19,409 Income tax (benefit) expense � 817 � (6,557 ) � 7,374
Net earnings $ 17,782 $ 5,747 $ 12,035 � Diluted earnings per
common share $ 0.40 $ 0.27 Premium Tax Presentation The Company
reports premium taxes as a component of revenues and general and
administrative expenses (gross basis). The following table shows
the Company�s Medicaid/SCHIP HBR and the Medicaid Managed Care
G&A ratio on a gross basis as reported as well as on a net
basis with premium taxes recorded as a reduction of revenues for
analytical purposes. Premium Taxes (in thousands) Medicaid/SCHIP
HBR Medicaid Managed Care G&A Ratio Current (Gross) Net Current
(Gross) Net 2007 Q1 $ 18,216 82.3 % 84.8 % 13.0 % 10.5 % Q2 �
19,874 80.6 83.1 14.0 11.5 Year to Date $ 38,090 81.5 84.0 13.5
11.0 � 2006 Q1 $ 4,305 82.8 % 83.7 % 11.9 % 11.0 % Q2 6,876 84.0
85.3 12.3 11.0 Q3 13,830 82.0 84.0 13.0 11.0 Q4 � 17,442 82.1 84.4
12.7 10.4 Total Year $ 42,453 82.6 84.3 12.6 10.8 About Centene
Corporation Centene Corporation is a leading multi-line healthcare
enterprise that provides programs and related services to
individuals receiving benefits under Medicaid, including the State
Children�s Health Insurance Program (SCHIP) and Supplemental
Security Income (SSI). The Company operates health plans in
Georgia, Indiana, New Jersey, Ohio, South Carolina, Texas and
Wisconsin. In addition, the Company contracts with other healthcare
and commercial organizations to provide specialty services
including behavioral health, health management, long-term care,
managed vision, nurse triage, pharmacy benefits management and
treatment compliance. Information regarding Centene is available
via the Internet at www.centene.com. The information provided in
this press release contains forward-looking statements that relate
to future events and future financial performance of Centene.
Subsequent events and developments may cause the Company's
estimates to change. The Company disclaims any obligation to update
this forward-looking financial information in the future. Readers
are cautioned that matters subject to forward-looking statements
involve known and unknown risks and uncertainties, including
economic, regulatory, competitive and other factors that may cause
Centene's or its industry's actual results, levels of activity,
performance or achievements to be materially different from any
future results, levels of activity, performance or achievements
expressed or implied by these forward-looking statements. Actual
results may differ from projections or estimates due to a variety
of important factors, including Centene's ability to accurately
predict and effectively manage health benefits and other operating
expenses, competition, changes in healthcare practices, changes in
federal or state laws or regulations, inflation, provider contract
changes, new technologies, reduction in provider payments by
governmental payors, major epidemics, disasters and numerous other
factors affecting the delivery and cost of healthcare. The
expiration, cancellation or suspension of Centene's Medicaid
Managed Care contracts by state governments would also negatively
affect Centene. � CENTENE CORPORATION AND SUBSIDIARIES �
CONSOLIDATED BALANCE SHEETS (In thousands, except share data) �
June 30, 2007 December 31, 2006 (Unaudited) ASSETS Current assets:
Cash and cash equivalents $ 236,443 $ 271,047 Premium and related
receivables 113,491 91,664 Short-term investments, at fair value
(amortized cost $43,636 and $67,199, respectively) 43,360 66,921
Other current assets � 46,257 � � 22,189 � Total current assets
439,551 451,821 Long-term investments, at fair value (amortized
cost $288,993 and $146,980, respectively) 287,719 145,417
Restricted deposits, at fair value (amortized cost $26,328 and
$25,422, respectively) 26,220 25,265 Property, software and
equipment, net 131,829 110,688 Goodwill 136,316 135,877 Other
intangible assets, net 14,472 16,202 Other assets � 13,895 � �
9,710 � Total assets $ 1,050,002 � $ 894,980 � � LIABILITIES AND
STOCKHOLDERS� EQUITY Current liabilities: Medical claims
liabilities $ 295,340 $ 280,441 Accounts payable and accrued
expenses 111,697 72,723 Unearned revenue 42,019 33,816 Current
portion of long-term debt � 972 � � 971 � Total current liabilities
450,028 387,951 Long-term debt 200,162 174,646 Other liabilities �
8,779 � � 5,960 � Total liabilities 658,969 568,557 Stockholders�
equity: Common stock, $.001 par value; authorized 100,000,000
shares; issued and outstanding 43,664,105 and 43,369,918 shares,
respectively 44 44 Additional paid-in capital 217,705 209,340
Accumulated other comprehensive income: Unrealized loss on
investments, net of tax (1,046 ) (1,251 ) Retained earnings �
174,330 � � 118,290 � Total stockholders� equity � 391,033 � �
326,423 � Total liabilities and stockholders� equity $ 1,050,002 �
$ 894,980 � � CENTENE CORPORATION AND SUBSIDIARIES � CONSOLIDATED
STATEMENTS OF OPERATIONS (In thousands, except share data) � For
the Three MonthsEnded June 30, For the Six Months Ended June 30,
2007 2006 2007 2006 (Unaudited) (Unaudited) � Revenues: Premium $
707,723 $ 476,079 $ 1,356,966 $ 911,641 Service 20,015 19,214
41,607 38,730 Total revenues 727,738 495,293 1,398,573 950,371
Expenses: Medical costs 574,862 400,229 1,110,268 761,901 Cost of
services 16,670 14,317 32,300 29,905 General and administrative
expenses 122,596 74,441 229,462 139,663 Gain on sale of FirstGuard
Missouri (3,254 ) � (7,472 ) � Total operating expenses 710,874
488,987 1,364,558 931,469 Earnings from operations 16,864 6,306
34,015 18,902 Other income (expense): Investment and other income
5,948 3,891 10,449 7,431 Interest expense (4,213 ) (2,456 ) (7,345
) (4,454 ) Earnings before income taxes 18,599 7,741 37,119 21,879
Income tax (benefit) expense 817 2,776 (18,874 ) 8,148 Net earnings
$ 17,782 $ 4,965 $ 55,993 $ 13,731 � Earnings per share: Basic
earnings per common share $ 0.41 $ 0.12 $ 1.29 $ 0.32 Diluted
earnings per common share $ 0.40 $ 0.11 $ 1.25 $ 0.31 � Weighted
average number of shares outstanding: Basic 43,617,360 43,169,590
43,525,848 43,079,243 Diluted 44,815,369 44,839,149 44,871,114
44,794,558 � CENTENE CORPORATION AND SUBSIDIARIES � CONSOLIDATED
STATEMENTS OF CASH FLOWS (In thousands) � Six Months Ended June 30,
2007 2006 (Unaudited) � Cash flows from operating activities: Net
earnings $ 55,993 $ 13,731 Adjustments to reconcile net earnings to
net cash provided by operating activities � Depreciation and
amortization 12,991 9,541 Stock compensation expense 7,837 7,154
Deferred income taxes (327 ) (287 ) Gain on sale of FirstGuard
Missouri (7,472 ) � Changes in assets and liabilities � Premium and
related receivables (21,823 ) (45,710 ) Other current assets
(24,583 ) 1,859 Other assets (931 ) (1,123 ) Medical claims
liabilities 15,035 16,690 Unearned revenue 8,203 1,705 Accounts
payable and accrued expenses 11,832 10,658 Other operating
activities � 3,119 � 224 Net cash provided by operating activities
� 59,874 � 14,442 Cash flows from investing activities: Purchases
of property, software and equipment (29,352 ) (23,472 ) Purchases
of investments (290,962 ) (113,665 ) Sales and maturities of
investments 196,407 97,445 Proceeds from asset sales 14,102 �
Acquisitions, net of cash acquired � (5,336 ) � (60,710 ) Net cash
used in investing activities � (115,141 ) � (100,402 ) Cash flows
from financing activities: Proceeds from exercise of stock options
2,651 3,761 Proceeds from borrowings 191,000 71,967 Payment of
long-term debt (165,484 ) (4,487 ) Excess tax benefits from stock
compensation 797 1,977 Common stock repurchases (3,231 ) (3,180 )
Debt issue costs � (5,070 ) � � Net cash provided by financing
activities � 20,663 � 70,038 Net decrease in cash and cash
equivalents � (34,604 ) � (15,922 ) Cash and cash equivalents,
beginning of period � 271,047 � 147,358 Cash and cash equivalents,
end of period $ 236,443 $ 131,436 � Interest paid $ 3,738 $ 4,598
Income taxes paid $ 6,049 $ 1,645 � CENTENE CORPORATION �
SUPPLEMENTAL FINANCIAL DATA � Q2 Q1 Q4 Q3 2007 2007 2006 2006
MEMBERSHIP Medicaid Managed Care: Georgia 281,400 291,300 308,800
252,600 Indiana 161,700 176,700 183,100 198,100 New Jersey 59,100
59,100 58,900 59,100 Ohio 128,200 118,300 109,200 88,300 South
Carolina 31,100 � � � Texas 333,900 318,500 298,500 259,900
Wisconsin 136,100 139,400 164,800 167,100 Subtotal 1,131,500
1,103,300 1,123,300 1,025,100 Kansas and Missouri � � 138,900
144,600 TOTAL 1,131,500 1,103,300 1,262,200 1,169,700 � Medicaid
846,900 839,600 887,300 818,000 SCHIP 216,500 211,200 216,200
189,100 SSI 68,100 52,500 19,800 18,000 Subtotal 1,131,500
1,103,300 1,123,300 1,025,100 Kansas and Missouri Medicaid and
SCHIP members � � 138,900 144,600 TOTAL 1,131,500 1,103,300
1,262,200 1,169,700 � Specialty Services(a): Arizona 95,200 93,600
94,500 94,500 Kansas 37,500 36,600 36,600 37,500 TOTAL 132,700
130,200 131,100 132,000 � (a) Includes behavioral health contracts
only. � REVENUE PER MEMBER(b) $ 198.98 $ 185.90 $ 173.75 $ 169.98 �
CLAIMS(b) Period-end inventory 284,800 326,000 296,100 233,500
Average inventory 244,600 239,400 195,700 188,600 Period-end
inventory per member 0.26 0.30 0.23 0.20 � (b) Revenue per member
and claims information are presented for the Medicaid Managed Care
segment. � Q2 Q1 Q4 Q3 2007 2007 2006 2006 DAYS IN CLAIMS PAYABLE
(c) 46.8 46.4 46.4 45.3 (c) Days in Claims Payable is a calculation
of Medical Claims Liabilities at the end of the period divided by
average claims expense per calendar day for such period. � CASH AND
INVESTMENTS (in millions) Regulated $ 527.9 $ 491.0 $ 479.8 $ 411.1
Unregulated � 65.8 � 71.8 � 28.9 � 29.0 TOTAL $ 593.7 $ 562.8 $
508.7 $ 440.1 � DEBT TO CAPITALIZATION (d) 34.0% 35.3% 35.0% 35.6%
(d)Debt to Capitalization is calculated as follows: total debt
divided by (total debt + equity). � HEALTH BENEFITS RATIO BY
CATEGORY: � � Three Months Ended June 30, Six Months Ended June 30,
2007 2006 2007 2006 Medicaid and SCHIP 80.6 % 84.0 % 81.5 % 83.4 %
SSI 87.5 87.6 87.2 87.6 Specialty Services 75.9 83.7 77.5 83.9
GENERAL AND ADMINISTRATIVE EXPENSE RATIO BY BUSINESS SEGMENT: � �
Three Months Ended June 30, Six Months Ended June 30, 2007 2006
2007 2006 Medicaid Managed Care 14.0 % 12.3 % 13.5 % 12.1 %
Specialty Services 15.8 17.4 15.8 19.3 MEDICAL CLAIMS LIABILITIES
(In thousands) Four rolling quarters of the changes in medical
claims liabilities are summarized as follows: � Balance, June 30,
2006 $ 187,204 Acquisitions 1,788 Incurred related to: Current
period 2,180,604 Prior period � (12,426 ) Total incurred �
2,168,178 Paid related to: Current period 1,889,731 Prior period �
172,099 Total paid � 2,061,830 Balance, June 30, 2007 $ 295,340
Centene�s claims reserving process utilizes a consistent actuarial
methodology to estimate Centene�s ultimate liability. Any reduction
in the �Incurred related to: Prior period� claims may be offset as
Centene actuarially determines �Incurred related to: Current
period.� As such, only in the absence of a consistent reserving
methodology would favorable development of prior period claims
liability estimates reduce medical costs. Centene believes it has
consistently applied its claims reserving methodology in each of
the periods presented.
Centene (NYSE:CNC)
Historical Stock Chart
From Jun 2024 to Jul 2024
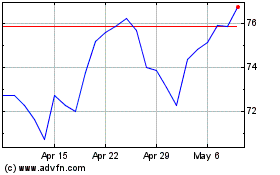
Centene (NYSE:CNC)
Historical Stock Chart
From Jul 2023 to Jul 2024
