Research based on Sun Life's high-cost claims data also
shows:
- Million-dollar+ claims increased 37% from 2018 to
2021
- Highest-dollar claims were due to combinations of in-patient
hospitalization, injectable/specialty drugs, comorbid conditions
and complicated surgeries
- Highest-cost claim in 2021 was $6.23
million, for hemophilia
- High-cost mental health claims increased 21% from 2020 to
2021
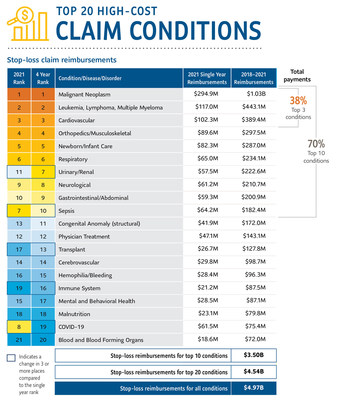
WELLESLEY, Mass., June 21,
2022 /PRNewswire/ -- Sun Life U.S. has released its
10th annual report on high-cost medical claims, analyzing its
stop-loss claims data and medical trends from 2018 – 2021. COVID-19
rose to a top 10 costliest condition in 2021, with the highest-cost
COVID-19 claim reaching $1.75
million. Other categories of medical claims, including
cancer and mental health claims, showed increases as well. The
report reviewed nearly 50,000 Sun Life member claims from more than
2,800 self-funded employer clients around the country, providing
research and data indicative of U.S. healthcare trends. The rise in
claims over the study period are the result of increases in
underlying medical claims cost as well as changes to Sun Life's
book of covered business.
According to the Kaiser Foundation's annual report on employee
benefits, 64 percent of employees in the U.S. are enrolled in
self-funded health plans. As the largest independent stop-loss
provider in the U.S., currently covering 5.3 million lives, Sun
Life covers high-dollar claims for employers who self-fund their
employee health plans. Sun Life also provides members with health
advisory and care navigation services through its Health Navigator
solution, powered by PinnacleCare.
"From COVID-19 to mental health, new treatments and healthcare
trends are continuously emerging and evolving, and self-funded
employers need guidance as they consider health plan designs and
how to best support their employees' health," said Jen Collier, senior vice president of Sun Life
U.S. Health and Risk Solutions. "Compiling this research every year
allows us to understand and provide analysis and insights on the
evolution of clinical and drug treatments and trends for the
highest-cost diagnoses. This helps employers understand how to
anticipate the potential frequency and costs of claims, as well as
assess risk factors and improve health outcomes. When we arm our
clients with the best information and expertise, they can make the
best decisions for the health of their employees."
Other key takeaways from the report:
Two years of COVID-19
- In 2021 COVID-19 was a top 10 condition with a total spend of
$114 million; in the four-year
ranking for 2018-2021, COVID-19 was still in the top 20 despite
only having claims for two of the four years.
- COVID-19 claims that were severe enough to breach stop-loss
deductibles averaged $231,300, with
the highest claim at $1.75
million.
- COVID-19 also contributed to the cost of care for two members
with primary conditions of sepsis with a total spend of over
$3 million each.
Mental health claims on the rise
- Total spend on mental and behavioral health claims rose by 22%
in 2021; the average cost per claim remained relatively flat at
$68,300, indicating that the increase
was mostly due to more members having high-cost mental health
claims, not higher costs of care.
- Depressive disorders saw the most significant growth at 85%,
while sleep/wake disorders rose by 68%, and alcohol- and
opioid-related claims increased as well.
Multi-million-dollar claims continue to rise
- From 2020-2021 the number of million-dollar+ claims increased
by 21% and increased 37% from 2018-2021 (adjusted for changes in
number of covered lives)
- In 2021 the conditions with the most frequent million-dollar+
claims were cancer, complications around newborn/infant care and
COVID-19.
- The $6.23 million claim for
hemophilia was driven almost entirely by injectable drug
costs.
- The highest-cost claim driven primarily by in-patient care was
for $5.43 million, for a congenital
anomaly (condition present at birth), with a comorbidity of
septicemia.
- Ten members had claims over $3
million in 2021, for conditions including hemophilia,
sepsis, cancer, burns, and complications around newborn/infant
care.
- Cost drivers for these claims include extended in-patient
hospitalization, complicated surgeries, injectable drugs/Rx
treatment, and comorbidities such as COVID-19, kidney failure, or
cardiac complications.
Medical vs. Rx/pharmacy costs
- Claims for three conditions – malnutrition, transplant and
hemophilia – had at least 70% of total costs from drugs.
- The cost of conditions like COVID-19 or complications around
newborn/infant care were driven almost entirely by medical spend
(not pharmacy), largely due to in-patient hospitalization.
Cancer trends
- The highest-cost cancer claim in 2021 was $5.41 million, driven by a combination of
in-patient care, complicated surgeries, and injectable drugs.
- Cancer has dominated the list of costliest conditions for ten
straight years, due to both overall cost and frequency of
claims.
- Eleven of the top 20 costliest injectable drugs are used to
treat cancer.
Sun Life's high-dollar claims report also offers employers
guidance on optimizing care and improving health outcomes which can
result in cost savings as well. Care navigation, site of care
changes, expert claims review, and employee wellness programs can
all help reduce the cost of care while improving the member's
medical journey.
Sun Life's recent webinar presenting additional insights from
the report is available to view here.
About Sun Life
Sun Life is a leading international financial services
organization providing asset management, wealth, insurance and
health solutions to individual and institutional Clients. Sun Life
has operations in a number of markets worldwide, including
Canada, the United States, the United Kingdom, Ireland, Hong
Kong, the Philippines,
Japan, Indonesia, India, China,
Australia, Singapore, Vietnam, Malaysia and Bermuda. As of March
31, 2022, Sun Life had total assets under management of
C$1.35 trillion. For more
information, please visit www.sunlife.com.
Sun Life Financial Inc. trades on the Toronto (TSX), New
York (NYSE) and Philippine (PSE) stock exchanges under the
ticker symbol SLF.
In the United States, Sun Life
is one of the largest group benefits providers, serving more than
55,000 employers in small, medium and large workplaces across the
country. Sun Life's broad portfolio of insurance products and
services in the U.S. includes disability, absence management, life,
dental, vision, voluntary and medical stop-loss. Sun Life and its
affiliates in asset management businesses in the U.S. employ
approximately 8,000 people. Group insurance policies are issued by
Sun Life Assurance Company of Canada (Wellesley
Hills, Mass.), except in New
York, where policies are issued by Sun Life and Health
Insurance Company (U.S.) (Lansing,
Mich.). For more information, please visit
www.sunlife.com/us.
|
Media
contacts:
|
|
|
Devon
Fernald
|
Anjie Coplin
|
|
Sun Life
U.S.
|
Sun Life
U.S.
|
|
781-800-3609
|
214-549-1553
|
|
Devon.Portney.Fernald@sunlife.com
|
Anjie.Coplin@sunlife.com
|
Connect with Sun Life U.S.
https://www.facebook.com/SLFUnitedStates
https://www.linkedin.com/company/sun-life-financial
https://twitter.com/SunLifeUS
 View original content to download
multimedia:https://www.prnewswire.com/news-releases/covid-19-was-one-of-the-costliest-medical-conditions-in-2021--with-the-highest-claim-reaching-1-75-million-sun-life-claims-data-shows-301571409.html
View original content to download
multimedia:https://www.prnewswire.com/news-releases/covid-19-was-one-of-the-costliest-medical-conditions-in-2021--with-the-highest-claim-reaching-1-75-million-sun-life-claims-data-shows-301571409.html
SOURCE Sun Life U.S.