By Melanie Evans and Elizabeth Findell
Advances in Covid-19 treatment have shortened hospital stays,
easing capacity strains. But doctors and health-care disaster
experts say the gains are not enough to meet a sustained rise in
hospitalizations, particularly in remote pockets of the country
that have smaller hospitals and fewer medical professionals.
Nationally, a spring surge of Covid-19 hospitalizations peaked
in mid-April and was followed by a second wave in late July. The
latest rise began in late September, data from the Covid Tracking
Project show, with the number soaring 60% from the low point that
month. People hospitalized with Covid-19 in the U.S. and its
territories reached 46,095 on Thursday.
Treatment of the disease remains limited and too many patients
with lengthy stays can still overwhelm available doctors and nurses
and swamp emergency departments and intensive-care units, they
say.
Those risks are greater now as fatigue with restrictions on
public life is complicating efforts to stem contagion. The virus is
also reaching more sparsely populated regions of the U.S. where
many hospitals are small and farther apart. Coinciding with the
latest surge, the nation has entered flu season, which typically
fills hospital beds each year.
"It's just a numbers game," said Dixie Harris, an intensive-care
doctor in Utah, who is anxiously making her own calculations for
how long beds will remain available at her hospital in Salt Lake
City.
Dr. Harris saw firsthand the consequences of overwhelmed
hospitals when she volunteered in New York in April. "You don't
want to be in an ICU without enough nursing," she said. "When you
don't get good nursing care, it's harder to survive."
The rise in hospitalizations is troubling but doesn't fully
reflect the risk to hospitals and patients from the latest wave,
health-care officials and disaster-response experts said.
"A couple things are not obvious just looking at the national
numbers," said Eric Toner, a senior scholar with the Johns Hopkins
Center for Health Security. The latest wave is spreading across a
wider geographic area, he said.
Locales swamped by Covid-19 in the spring were concentrated in a
few spots, primarily New York, Dr. Toner said. As patients now
stream into hospitals across many states, there are fewer
unaffected areas able to send relief, such as temporary nurses and
doctors.
New York and New Jersey hospitals accounted for nearly half --
45% -- of hospitalizations in the U.S. and territories at the peak
of the spring surge, Covid Tracking Project data show. The second
wave was concentrated in California, Florida and Texas, which had
49% of hospitalizations at the late July peak. Now, about the same
percentage is spread across nine states: Texas, California,
Illinois, Florida, Georgia, Indiana, Ohio, Wisconsin and
Tennessee.
"It is much more difficult when everyone is feeling the pain at
the same time," said Jonathan Greene, an official dealing with
preparedness and response within the U.S. Department of Health and
Human Services. "There is a finite number of resources."
Mr. Greene oversees some health-care workers deployed to provide
federal relief in disasters. During the pandemic, many such
personnel have already been sent more than once to help with
Covid-19 emergencies, he said.
Cases are also surging across rural regions of the country. The
total numbers of Covid-19 hospital patients are smaller but so too
is the number of hospitals in remote areas, Mr. Greene said.
Without another hospital nearby, more outside aid is needed.
In Red Lodge, Mont., the local 10-bed hospital is now often over
capacity, placing overflow patients in beds normally used for those
needing temporary observation, said Kelley Evans, chief executive
of the hospital, Beartooth Billings Clinic.
The Red Lodge facility is one of 14 small hospitals owned by, or
have agreements with, the Billings Clinic. The small hospitals,
separated by as many 470 miles, typically transfer sicker patients
to the flagship Billings Clinic hospital in Billings, Mont.
But as coronavirus cases surge in the state, the 290-bed
flagship hospital is sending Covid-19 patients to Beartooth, which
also continues to care for local patients. As occupancy across the
region rises, Beartooth and other hospitals are swapping staff to
fill emergency shortages when health-care workers enter quarantine
after being exposed to the virus.
Beartooth had one radiology technician to cover the emergency
room around the clock after two other technicians needed to
quarantine, Ms. Evans said. Doctors would hastily meet to consider
options for how to treat trauma patients without diagnostic imaging
before temporary help arrived from another hospital, she said.
Beartooth sent nurses to Billings briefly, but couldn't afford
to go long without them. "It's tight," Ms. Evans said. "It's
completely tight. We all have to take a deep breath and say 'We can
do this today.' "
So far, Beartooth hasn't seen patients with influenza, but the
seasonal virus typically fills some hospital beds each year. "It's
keeping me up at night," Ms. Evans said. "I don't know how much
longer this is sustainable."
Last year, the flu sent about 400,000 people to U.S. hospitals
in what the Centers for Disease Control and Prevention called a
moderate season. Officials fear the flu-virus overlap with Covid-19
could mean little relief for hospitals in coming months.
"This is a sign of things to come," said Jim Murphy, Montana's
administrator of the Communicable Disease and Laboratory Services
Division for the Montana Department of Public Health & Human
Services.
HCA Healthcare Inc., one of the nation's largest hospital
systems, saw its ICU capacity increase as the Nashville-based
company used data analytics to monitor care of critically ill
patients and ventilator use, Chief Executive Sam Hazen told
analysts earlier this month. "It creates a lower length of stay for
the patient and ultimately a much better outcome," he said.
New treatments, though limited, have also helped improve care
and shorten hospital stays for Covid-19 patients. Those gains and a
rising number of infections among young people -- who are the least
likely to die if infected -- have probably helped lower the death
rate, according to epidemiologists, though measuring that rate is
challenging.
Steroids and remdesivir are "great weapons in the arsenal of
Covid 19" and have shortened hospital stays, said Ryan Mielke,
spokesman for the University Medical Center in El Paso.
But the benefit of improved care and shorter hospital stays can
be overmatched if people relax health precautions, he said.
A month ago, University Medical Center had 30 Covid-19 patients.
Thursday, it had 206, many of them in tents serving as makeshift
ICUs in a city that has seen a sustained rise in coronavirus cases
for weeks, he said.
"It's fatigue," Mr. Mielke said. "Mitigation efforts such as
staying away from groups start to get put aside and people want to
see their friends, they want to go to a restaurant. People are not
wearing masks."
Officials said the majority of new cases involve people under
30, but they are spreading their infection to more-vulnerable
populations.
New cases of Covid-19 have been steadily rising for a month in
El Paso, Texas's sixth largest city, and hospital administrators
have warned that facilities were approaching capacity. El Paso
County has averaged 942 new cases daily in the past two weeks --
the most in Texas -- up from a daily average of 137 in September.
Deaths, which typically lag behind new cases by a few weeks, have
stayed in the single digits. The region appealed to the state for
help as Covid patients filled more than a third of its hospital
beds.
Other hospitals in El Paso treating coronavirus patients have
added tents. But some patients are being flown to hospitals in
cities hundreds of miles away, such as Dallas and San Antonio. The
Texas Division of Emergency Management is sending medical equipment
and personnel to turn the El Paso Convention and Performing Arts
Center into a temporary hospital with up to 100 beds. The state has
also assisted hospitals with extra beds and more than 900 medical
workers.
"The alternate care site and auxiliary medical units will reduce
the strain on hospitals in El Paso as we contain the spread of
Covid-19 in the region," Gov. Greg Abbott said in a news
release.
Write to Melanie Evans at Melanie.Evans@wsj.com and Elizabeth
Findell at Elizabeth.Findell@wsj.com
(END) Dow Jones Newswires
October 30, 2020 16:30 ET (20:30 GMT)
Copyright (c) 2020 Dow Jones & Company, Inc.
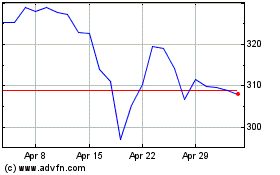
HCA Healthcare (NYSE:HCA)
Historical Stock Chart
From Mar 2024 to Apr 2024
HCA Healthcare (NYSE:HCA)
Historical Stock Chart
From Apr 2023 to Apr 2024
