By Stephanie Armour
This article is being republished as part of our daily
reproduction of WSJ.com articles that also appeared in the U.S.
print edition of The Wall Street Journal (July 30, 2019).
Hospitals would have to disclose the discounted prices they
negotiate with insurance companies under a Trump administration
rule that could upend the $1 trillion hospital industry by
revealing rates long guarded as trade secrets.
Hospitals that fail to share the discounted prices in an online
form could be fined up to $300 a day, according to the proposal.
The price-disclosure requirements would cover all the more than
6,000 hospitals that accept Medicare, as well as some others, and
is likely to face fierce industry opposition.
Comments on the proposal would be due in September and, if
completed, the rule would take effect in January.
The initiative represents the Trump administration's growing
effort to shift away from rolling back the Affordable Care Act and
put its own stamp on health care instead. Central to that strategy
is the notion that more price transparency will inject greater
competition into the market and lower costs.
Industry groups have argued the requirement goes beyond the
executive branch's statutory authority and could backfire by
causing prices to rise if hospitals see their competitors are
getting higher insurer payments. The White House has lost in court
before: A rule requiring drug makers to post list prices in
television ads was blocked in June by a federal judge who said the
administration overstepped its regulatory authority.
Some Republicans praised the administration's focus. Sen. Lamar
Alexander (R., Tenn.) said the proposal complements provisions in
legislation he sponsored with Sen. Patty Murray (D., Wash.) to
lower health costs.
"We will carefully review how the proposed rule and our
legislation interact," he said.
The Trump administration's move contrasts sharply with proposals
by some leading Democratic presidential contenders who say Medicare
for All will drive down costs by lowering administrative overhead,
curbing spending and leveraging the federal government's
negotiating clout to drive down prices. It lands on the eve of the
second Democratic presidential debate Tuesday and Wednesday that is
expected to focus on health care, which polls show is a top issue
for voters in the 2020 election.
Hospitals would have to disclose the rates for services and
treatment that they have negotiated with individual insurance
companies such Cigna Corp., Anthem Inc. and CVS Health Corp.'s
Aetna under the proposal released Monday. The Trump administration
is also working on initiatives that could compel insurers to
disclose their rates, part of a push to publicize costs that is
likely to spur lawsuits and sharp resistance from the industry.
"It's very significant. It's a turning point in health care and
a turning point to the free market in health care," Seema Verma,
administrator of the Centers for Medicare and Medicaid Services,
said in an interview. "It hasn't been a competitive free-market
system."
Tom Nickels, executive vice president of the American Hospital
Association, said it is "a radical approach."
"This really is an extreme proposal in terms of what we all
expected," he said. "It raises a number of legal issues we'll have
to work through. It takes the concept to the extreme.
"Publicly disclosing competitively negotiated, proprietary rates
will push prices and premiums higher -- not lower -- for consumers,
patients and taxpayers," said Matt Eyles, president and CEO of
America's Health Insurance Plans, an industry trade group.
The proposed rule is estimated to cost hospitals around $6
million total. It would affect hospitals as well as their
subsidiaries, including outpatient health clinics. Hospitals must
already post their list prices for services.
The administration's proposal would expand that requirement to
include not only gross charges before discounts but also the
insurer-specific negotiated charges for all items and services. The
charges would have to be linked to the name of the insurer and
would have to be updated annually. The data would have to be
displayed in a machine-readable format so it could be processed by
a computer, and listed by common billing or accounting codes to
create a framework for comparing standard charges among
hospitals.
The proposal would also require hospitals to disclose
insurer-specific negotiated charges for about 300 services
consumers are likely to shop for before obtaining care, such as
X-rays, outpatient visits, lab tests or childbirth. That price data
would have to be made public in a prominent location online or in
written form on request.
The Trump administration said Monday that it is also seeking
comment for price information that would be useful for consumers,
as well as comment on the type of services that should be
included.
The rule, if finalized, would reveal how widely costs vary in
the U.S. for care. A magnetic-resonance image of the lower back
costs $141 at an imaging center in Jefferson, La., but runs $47,646
at a hospital in Torrance, Calif., according to data from Clear
Health Costs, a New York company that publishes information about
health-care costs.
"I would hope this drive on transparency would unify the left
and right, " Health and Human Services Secretary Alex Azar said in
an interview. "The opponents here are the proponents of the status
quo who will attack us."
Technology companies will use the information to make it
available for consumers and patients, he said. "Just imagine having
that information out there, how powerful it will be," he said.
Data on the effect of increasing price transparency in health
care shows mixed results. In some cases, consumers equate higher
cost with higher quality and can be attracted to higher-priced
treatments and services. Other studies show that only a fraction of
people who have price data actually use the information to shop
around for care. Many are already shielded from the full costs
because insurance covers the bulk of their treatments.
The proposal wouldn't affect hospitals run by Veterans Affairs,
Indian Health Services and Defense Department military treatment
centers. State-licensed hospitals would also be covered by the
proposal.
The administration is also proposing several policies aimed at
reducing payment differences between certain outpatient service
sites and expanding the types and number of services, such as total
knee replacements, that can be performed outpatient or in
ambulatory surgical centers. Those tend to cost less when done as
outpatient procedures.
Write to Stephanie Armour at stephanie.armour@wsj.com
(END) Dow Jones Newswires
July 30, 2019 02:47 ET (06:47 GMT)
Copyright (c) 2019 Dow Jones & Company, Inc.
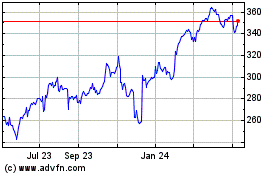
Cigna (NYSE:CI)
Historical Stock Chart
From Mar 2024 to Apr 2024
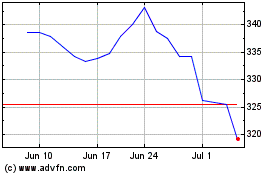
Cigna (NYSE:CI)
Historical Stock Chart
From Apr 2023 to Apr 2024