By Ted Alcorn
The crowd at the New Orleans health clinic in late June filled
the seats and overflowed into the wings. Louisiana Gov. John Bel
Edwards was there, as were employees from Gilead Science's
affiliate Asegua Therapeutics. They had gathered to launch a plan
for the statewide elimination of hepatitis C, which killed more
than 17,000 Americans in 2017.
The event, however, wasn't prompted by the discovery of a new
cure. Officials were unveiling a new way of paying for an existing
therapy.
It is rare for government officials and companies to celebrate a
financial agreement. But in recent years, progress in addressing
hepatitis C has been hampered not by a lack of innovative drugs but
by a marketplace that fails to make those drugs widely available.
When breakthrough therapies that rapidly cure the chronic infection
were introduced starting in late 2013, manufacturers charged prices
in the tens of thousands of dollars per course of therapy. Many
insurers proved willing to pay, bringing the drug companies tens of
billions of dollars.
But many health-care payers with fixed budgets such as state
Medicaid programs and correctional health systems balked at the
prices, and set criteria that effectively reduced the number of
infected patients eligible for treatment. Louisiana exemplified the
problem: An estimated 39,000 people in the state's Medicaid program
or in its prisons are infected with hepatitis C, but in 2018 just
over 1,000 were treated.
So shortly after her appointment in 2016, Louisiana Secretary of
Health Rebekah Gee decided it was time for a new approach. "I found
it unacceptable that people would get sick and die from a disease
that is curable," she says.
Early on, Dr. Gee played hardball, openly exploring whether to
ask the federal government to invoke a century-old provision of
patent law that would force the manufacture of the drugs for the
public good, at a vastly discounted price. The proposal, strongly
opposed by drugmakers, may have helped bring them to the
negotiating table, where a framework for a voluntary agreement
began to emerge.
Sealed after nearly two years of subsequent negotiation, the
final agreement effectively made Asegua the primary provider of
hepatitis C therapies for the state's Medicaid and correctional
populations for the next five years.
In return, the drug company agrees to de-link the volume of
drugs it provides from the payments received. That means instead of
selling the medication by the dose, the company will provide as
much as the state can dispense to the Medicaid and correctional
populations. This arrangement has been likened to a Netflix
"subscription," where the price customers pay isn't linked to the
volume of movies they stream, and their total consumption isn't
capped. The state will effectively pay a fixed price to access all
of the drugs it can use. The agreement sets this amount at roughly
$60 million, equivalent to what the state paid in the 2019 fiscal
year.
Crucially, where Louisiana previously saw costs increase with
every patient it enrolled in treatment, this arrangement
incentivizes the state to identify and treat as many people as
possible because the marginal cost of each additional patient is
essentially zero. With the new contract signed, the state has
promised to treat 80% of both Medicaid and correctional populations
by 2024.
If it achieves that goal, by treating more than 31,000 people in
five years, the cost per patient will be less than $10,000. Experts
say that is likely lower than the price paid by many other states
but still highly profitable for Asegua, as the company has long
since recouped its investment in hepatitis C therapies. Ingredients
to make a course of treatment are estimated to cost less than
$100.
For Asegua, which declined to comment on the price per patient,
the deal gives it guaranteed income and a chance to claim credit
for helping expand treatment at a time when public anger about high
drugs prices is growing. "Partnering with Louisiana on this unique
model was born from our commitment to making our innovative
medicines accessible to those who need them," the company said in a
statement.
Enormous promise
Health-policy experts say the agreement -- the first of its kind
for a U.S. state -- could serve as a model for other health-care
payers increasingly looking for innovative ways to manage costs and
pay more directly for health itself.
A month after Louisiana's agreement was revealed, Washington
state announced a similar arrangement with drugmaker AbbVie. Other
states have expressed interest in these approaches, too, though
none have confirmed they are developing their own models. "We're
all sort of learning from each other and trying to figure out what
works best," says Judy Zerzan, chief medical officer of Washington
state's Health Care Authority.
Although the hepatitis C epidemic is unique in many respects --
there is a large and clearly defined population of infected people
who lack access to treatment, all of whom can be effectively cured
with a single therapy, and multiple, competing manufacturers
capable of providing it -- experts say the subscription model could
have applications for other diseases, as well.
Rena Conti, an associate professor at Boston University's
Questrom School of Business who helped Louisiana develop its
agreement, says the model might be applied to purchases of
medications for pre-exposure prophylaxis for HIV, known as PrEP.
She also points to products that are on the horizon, including gene
and stem-cell therapies to treat children with congenital disorders
like sickle cell anemia.
The U.K., meanwhile, recently announced it will test a
subscription agreement to purchase antibiotics. Unlike Louisiana,
which sought to expand treatment, the U.K. hopes to reduce
drugmakers' incentives to widely market their products, limiting
unnecessary use that can contribute to antimicrobial
resistance.
These endeavors are part of a larger wave of innovative payment
models that attempt to better align the price of drugs with the
scale and pace of benefit they provide. Oklahoma, Colorado, and
Michigan recently obtained federal approval to negotiate new
value-based agreements with drugmakers, like scaling payment for a
drug to the health benefit it yields. And the Senate's leading
effort to reduce drug prices, introduced by Sens. Chuck Grassley
and Ron Wyden in late July, would allow installment plans for some
expensive one-time therapies, so insurers could gradually pay for
them as treated patients accrue benefit from them.
"There is enormous promise in the idea," says Josh Sharfstein, a
vice dean at the Johns Hopkins Bloomberg School of Public Health.
"Way too much of the discussion on drug pricing is about the cost
per pill, and way too little is about whether we're really
improving the health of the community,"
Clearing hurdles
Louisiana's payment model may sound simple, but the route to it
was far from straightforward.
In addition to getting drugmakers to the negotiating table,
Louisiana had to overcome federal regulations meant to keep drugs
affordable for the poorest patients. By law, drugmakers must offer
their drugs to state Medicaid programs at the best price they sell
to any other payer. It wasn't until June that the Centers for
Medicare and Medicaid Services authorized Louisiana to implement
its subscription agreement outside of the "best price" rule, which
could have forced Asegua to revise its Medicaid contracts with
other states.
When the Louisiana agreement went into effect on July 15,
Cassandra Youmans, a doctor who has been treating patients with
hepatitis C at University Medical Center New Orleans since 2008,
combed through her records to identify Medicaid patients who had
previously been denied treatment.
In the first week, she started 65 of them on medications, more
than she has ever initiated in a comparable period. And a
once-labyrinthine process of getting insurers' approval was now
instantaneous and nearly seamless: She could see a patient for the
first time, order a prescription at the pharmacy downstairs and
begin the patient's treatment immediately.
"This new program has revolutionized treatment," she says.
Making medications accessible is a crucial step, but officials
acknowledge that on its own, it isn't sufficient to end the
hepatitis C epidemic. Most people with hepatitis C are early in
what can be a decadeslong progression of disease, and are unaware
they are infected. To help identify those patients, Louisiana is
asking health-care providers to begin offering opt-out testing to
people who visit their emergency departments, among many other
changes.
In Australia, which adopted a subscription model for hepatitis C
treatment in 2016 but didn't pair it with broad screening of the
population, treatment numbers spiked at first, but then tapered
off.
"Subscription models are great if they are a holistic program
that includes screening, linkage to care, and treatment," says
Homie Razavi, who directs the nonprofit Centers for Disease
Analysis Foundation, which has modeled hepatitis C elimination
strategies for both the Australian and Louisianian governments.
"But if the focus is only treatment, it's going to fizzle out in a
few years."
Mr. Alcorn is a writer in New York. Email him at
reports@wsj.com.
(END) Dow Jones Newswires
September 13, 2019 10:05 ET (14:05 GMT)
Copyright (c) 2019 Dow Jones & Company, Inc.
AbbVie (NYSE:ABBV)
Historical Stock Chart
From Mar 2024 to Apr 2024
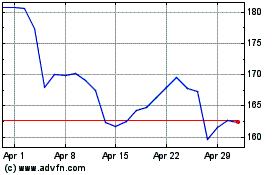
AbbVie (NYSE:ABBV)
Historical Stock Chart
From Apr 2023 to Apr 2024
