By Sarah Krouse and Brianna Abbott
Companies are racing to bolster Covid-19 testing as schools
reopen and flu season approaches, saying they aim to avoid a repeat
of July when overwhelming demand for testing led to long delays for
results.
In a Boston lab where technicians have programmed yeast to
produce cannabinoid molecules for medical-marijuana products,
scientists are now working to develop a Covid-19 testing system
that searches for the virus's genetic code. The company, Ginkgo
Bioworks Inc., hopes by the fall to create a system that will use
analyzers the size of washing machines to process 100,000 tests a
day.
Meanwhile, scientists at Sonora Quest Laboratories LLC are
assembling new equipment that might soon deliver a 10-fold increase
in molecular coronavirus-testing capacity at one of Arizona's
largest private labs. Other companies including Abbott Laboratories
and public-health authorities are aiming for broader Covid-19
diagnosis and screening with large-scale production of rapid
antigen tests that don't need to be shipped to laboratories for
processing.
The combined goal of these efforts is to quickly diversify and
grow the U.S.'s Covid-19 testing infrastructure as the flu season
approaches. This fall, doctors are concerned about a potential
swell of people with respiratory symptoms who might seek testing to
figure out which virus they have, stressing capacity and supplies
of components needed for both kinds of tests.
"I see this like us ramping up as a nation after Pearl Harbor
was bombed, " Emily Volk, president of the College of American
Pathologists, said of the U.S. building up Covid-19 testing
capacity. "I think right now, it's the calm before the storm with
the fall flu season."
Dr. Volk, who is also the senior vice president of clinical
services at University Health System in San Antonio, said she is
pushing the lab's suppliers to ensure there will be enough swabs
and transport liquid -- needed both for flu and Covid-19 laboratory
tests.
Flu season complicates Covid-19 testing efforts, public-health
officials say, because both ailments can have similar symptoms like
fever and fatigue, along with other viruses such as respiratory
syncytial virus, or RSV.
Tests that can detect several pathogens such as the flu and
Covid-19, called multiplex tests, are also slowly coming to market
and might help doctors avoid diagnostic trial and error.
Companies including Salt Lake City-based BioFire Diagnostics
have received emergency approval for a test that detects several
pathogens, in addition to a multiplex test from the Centers for
Disease Control and Prevention. San Diego-based Quidel Corp., which
is ramping up production of its Covid-19 rapid antigen test, which
looks for virus proteins, aims to introduce a test that
simultaneously checks for coronavirus antigens and the flu by the
end of next month.
Supply shortages persist for chemicals needed to process tests,
and are likely to continue, in part because most flu tests rely on
the same components, equipment and personnel as Covid-19 tests,
pathologists say. Around 30 components feed into a Covid-19 test,
said Eric Blank, an official at the Association of Public Health
Laboratories. A shortage in any one of the components holds up
capacity.
A surge in demand for testing in July as the new coronavirus
spread in the South and West of the country strained capacity and
led to weekslong delays for some test results, stymying
contact-tracing and containment efforts.
The virus spread fast as states reopened before hitting
public-health checkpoints -- and as some Americans refused to wear
masks. Efforts to expand testing capacity couldn't keep pace,
supply-chain constraints persisted, and big diagnostic companies,
including Quest Diagnostics Inc. and Laboratory Corporation of
America Holdings, or LabCorp, were quickly overwhelmed with
demand.
A spokeswoman for Quest says that the company is continuing to
coordinate with its suppliers and preparing additional testing
options for Covid-19 and other respiratory illnesses. By Labor Day,
the company expects to have the capacity to run 185,000 Covid-19
molecular tests a day, which is 60,000 more than the capacity in
mid-July, she said.
A significant increase in demand and supply-chain constraints in
early July meant LabCorp's average turnaround time for results
briefly shifted to four to six days, but is now one or two days, a
company spokeswoman said. It is expanding capacity as equipment and
supplies are available, she added, and preparing for flu and
Covid-19 testing.
Testing capacity in the U.S. expanded through the end of July,
but it wasn't enough to meet a wave of demand for tests.
Some states have since revised criteria for who should be
prioritized for a test, which, along with long wait-times, has
tamped down some demand for testing. The CDC has also dialed back
guidelines for who should be tested, saying close contacts of those
with confirmed Covid-19 cases don't necessarily need to get tested
if they don't have symptoms. The agency didn't say the guideline
was changed as a result of capacity concerns.
Cases have also fallen in states that had outbreaks earlier in
the summer and the total amount of testing done has declined. The
seven-day average of new daily tests in the U.S. was 696,886 as of
Friday, down from 812,260 a month earlier, according to the Covid
Tracking Project.
Experts say that prevention efforts could yet mitigate both
Covid-19 and the flu season, but they aren't counting on that and
say the U.S. must prepare for surges in Covid-19 cases along with
similar-looking respiratory viruses.
As many as 45 million people in the U.S. get the flu every year,
leading to more than 34,000 deaths, according to the CDC. Not
everyone is typically tested for it.
Testing capacity continues to grow, said Brett Giroir, the Trump
administration's testing coordinator, and the U.S. should have more
than 90 million coronavirus tests available in the month of
September compared with 25 million done in July. The U.S.'s growing
testing capacity is adequate, he said, but isn't enough for every
American to regularly get tested.
One major lesson from July: The lab-based molecular tests that
comprise the bulk of the U.S.'s current testing infrastructure
can't scale fast enough to keep up with large surges in demand.
That makes additional forms of testing key, some pathologists and
public-health officials say.
At Sonora Quest, Chief Executive David Dexter formed a plan in
late June to expand the number of Covid-19 tests the company could
process from 6,000 a day -- which was lower than usual because of
limited reagent supplies -- to 15,000.
When he presented his idea to state health officials and
executives at one of the lab's parent companies, they urged him to
boost capacity to 60,000 within the next two months, he said.
The lab hired 200 additional staff members and built new
equipment as testing demand surged. By early August, the company
had cleared a backlog that had grown to 65,000 tests the month
before, and shortened turnaround times to one to three days from a
week or more.
Sonora Quest can now handle about 30,000 tests a day and expects
to meet a goal of 60,000 by mid-September.
"I'm not spiking the ball and saying it's a complete success
because we still have a lot of work to do," Mr. Dexter said.
To turbocharge U.S. testing capacity, some biotechnology and
life-science companies are also developing new testing methods that
can process thousands of samples simultaneously.
Ginkgo is planning to use technology that looks for the virus's
genetic material in a large number of samples at the same time. It
is one of several companies that has received funding through a
National Institutes of Health competition meant to speed up the
development of diagnostic technologies.
"We saw this as essentially a logistics and scale problem,"
Jason Kelly, Ginkgo's founder, said of U.S. Covid-19 testing.
Rapid antigen testing is also growing in the U.S., with many
public-health experts pushing for more widespread use of the
technology.
A coalition of more than two dozen states, cities and tribes has
partnered with the Rockefeller Foundation to place large orders of
antigen tests and the analyzers that run them.
Accurate, rapid antigen tests can help doctors quickly determine
whether a person has Covid-19, making them a critical tool for the
coming flu season, said Rachel Levine, health secretary at the
Pennsylvania Department of Health at a media briefing earlier in
August.
Several companies are also working on rapid tests that could be
done at home like a pregnancy test, though those aren't yet on the
market.
Abbott last week received emergency authorization for a $5 rapid
antigen test the size of a credit card that is run by a health-care
professional and intended for people with symptoms within seven
days of their onset. The Trump administration has agreed to buy 150
million of those tests, an order an Abbott spokeswoman said the
company plans to fulfill.
Write to Sarah Krouse at sarah.krouse@wsj.com and Brianna Abbott
at brianna.abbott@wsj.com
(END) Dow Jones Newswires
August 30, 2020 15:46 ET (19:46 GMT)
Copyright (c) 2020 Dow Jones & Company, Inc.
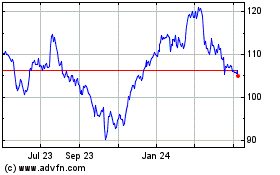
Abbott Laboratories (NYSE:ABT)
Historical Stock Chart
From Mar 2024 to Apr 2024
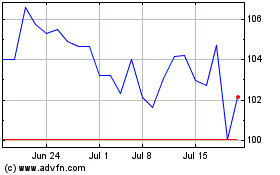
Abbott Laboratories (NYSE:ABT)
Historical Stock Chart
From Apr 2023 to Apr 2024