By Drew Hinshaw and Gabriele Steinhauser
Rich countries have preordered more than three billion doses of
Covid-19 vaccines, threatening to leave poor nations struggling to
inoculate more than a fraction of their billions of people and
raising the prospect that the disease could spread for years to
come.
Now, with three Western vaccines showing promising effectiveness
and a coalition of international health agencies gaining traction,
there is cautious optimism in the world's poorest countries as they
scramble to secure some doses.
Europe and America have reserved enough Covid-19 vaccine doses
to inoculate their entire populations, claiming the shots before
they are even manufactured and squeezing supply for other
countries. Meanwhile, China has mainly allocated its vaccines for
its own 1.4 billion citizens, outside of a few thousand people in
the United Arab Emirates and Bahrain.
That has left many governments in Africa, Latin America and
South Asia dependent on a small cluster of international and
nongovernmental health agencies based in Switzerland, particularly
the World Health Organization, and GAVI, a Geneva-based
organization that stockpiles vaccines. Collectively, those agencies
hope to vaccinate at best 20% of the population of the world's 92
poorest countries by the end of next year, primarily health-care
workers, the elderly and those with other diseases that make
Covid-19 more deadly.
That effort has been picking up steam in recent days.
On Monday, AstraZeneca PLC and the University of Oxford
announced their vaccine appears to be up to 90% effective. The
developing world has laid its hopes on that vaccine, since it is
priced at just a few dollars a dose and can be transported and
stored for six months in ordinary refrigerators, making it best
suited for countries that lack a sophisticated network of ultracold
freezers. GAVI has purchased some 300 million doses of the vaccine,
enough to inoculate around 100 million people, assuming that some
doses will go to waste because of refrigeration problems or other
issues.
But other vaccines are gaining some traction in the global South
as well. GAVI says it is in talks over whether to buy doses from
Pfizer Inc., which now says its vaccine, produced at ultralow
temperatures, can be stored in ordinary refrigerators for up to
five days. It is also in discussions with Moderna Inc., which says
its vaccine can last for a month in a fridge.
GAVI has raised the $2 billion it needed this year to fund
vaccine purchases, though officials there said they would need to
find another $5 billion next year. The institution expects to hold
talks soon with President-elect Joe Biden's team on increasing U.S.
support for the global vaccination drive.
It is still an uphill battle. "What we need to recognize is that
first and foremost we are going to be in a situation of short
supply of vaccines for the year ahead of us," said Managing
Director Aurélia Nguyen of GAVI's vaccination effort. "Something
like this has never been attempted before."
At stake is whether the developing world becomes a reservoir for
an airborne disease that could continue to circulate and claim
lives on the back of global trade and travel. In many low-income
countries, lockdowns and other restrictions on social and economic
activity have already rolled back decades of progress in health
care, schooling and poverty reduction. Delays in getting a vaccine
would push them still further behind.
As vaccines emerge, global public-health specialists worry about
a future in which the burden of Covid-19 shifts onto much poorer
countries, where the virus may linger, perhaps for years.
WHO officials have raised the possibility that, given the
challenges of vaccinating the entire global population, the new
coronavirus might never go away, and will instead become endemic to
the human population, like other vaccinable diseases such as
measles.
Only two diseases have ever been eradicated using a vaccine:
smallpox, and the cattle-spread viral infection rinderpest. Others
have proven stubbornly resistant, like polio, which was only fully
eradicated from Europe in 2002, half a century after a vaccine
emerged, and which remains present in Afghanistan and Pakistan.
For Covid-19, the potential cost in lives is considerable: If
the world's 50 richest countries secure the first two billion doses
of vaccines, the pandemic's ultimate death toll will be twice as
large as it would be if supply was shared more evenly, a study
funded by the Bill & Melinda Gates Foundation and conducted at
Northeastern University found in September.
And there are other risks: Some virologists worry that the virus
could mutate in ways that render current vaccines ineffective.
"It is absolutely in the U.S. interest to make sure the world
gets vaccinated as well," said former U.S. Centers for Disease
Control and Prevention Director Tom Frieden. "This isn't just an
ethical position, though it is of course ethically correct. It's a
practical issue."
So far, it isn't clear whether the current vaccines, which have
proven to work well in more-developed countries, will be as
effective in poorer parts of the world. Differences in nutrition
and the prevalence of other health conditions, such as HIV, could
make vaccines less effective in poorer countries, vaccine experts
warn.
That has been the case with other vaccines, such as the one
against rotavirus, which can cause severe diarrhea in children. The
data supporting the announcements from Pfizer, Moderna and
AstraZeneca stems from trials in rich countries like the U.S. and
the U.K. and middle-income countries such as Brazil.
Even if developing countries can secure enough doses, huge
logistical challenges remain to get them to the people who need
them. Just 10% of health centers in developing countries have
reliable electricity supply, while about half have no electricity
at all, according to GAVI.
That means even keeping doses refrigerated between 2 and 8
degrees Celsius can be difficult, said Marco Gaudesi, a pharmacist
who manages temperature-controlled supply chains and other
logistics for Doctors Without Borders.
Health-care workers in poor countries also usually have
less-specialized training, so may struggle with vaccines that
require mixing different vials before being administered or have to
be thawed from subzero temperatures. "There are so many smaller
differences that might not have an impact in developed countries
that may have an impact in a different context," said Mr.
Gaudesi.
Still, WHO officials are less concerned about so-called cold
chain issues than they once were. After detailed discussions with
drugmakers over transportation requirements and packaging, GAVI and
the WHO have decided they don't need to massively invest in the
kind of extensive array of ultracold freezers they used to
distribute an Ebola vaccine in the Democratic Republic of Congo.
AstraZeneca's vaccine doesn't require that kind of storage, and
Moderna's candidates can be dispatched in refrigerated
vehicles.
"Based on the analytics that we have, it's not that we have to
expand the cold chain to some extraordinary degree we've never seen
before," said a senior WHO official. "It's not the major
issue...it's something you can plan for."
Write to Drew Hinshaw at drew.hinshaw@wsj.com and Gabriele
Steinhauser at gabriele.steinhauser@wsj.com
(END) Dow Jones Newswires
November 25, 2020 08:14 ET (13:14 GMT)
Copyright (c) 2020 Dow Jones & Company, Inc.
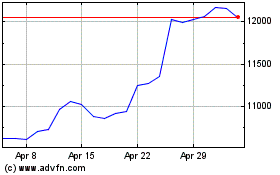
Astrazeneca (LSE:AZN)
Historical Stock Chart
From Mar 2024 to Apr 2024
Astrazeneca (LSE:AZN)
Historical Stock Chart
From Apr 2023 to Apr 2024
