Amarin Corporation plc (NASDAQ:AMRN) supported new data, presented
at American Heart Association’s (AHA) Virtual Scientific Sessions
2020, held virtually from November 13 – 17, 2020, adding to the
growing body of knowledge on VASCEPA® (icosapent ethyl) and its
differentiated positioning in treating patients at risk for major
adverse cardiovascular events (MACE). The data, from a broad group
of clinicians and scientists, continues to reinforce the unique
mechanistic, clinical, and pharmacoeconomic impact of VASCEPA.
“The AHA Virtual Scientific Sessions 2020 is an
important opportunity for the medical community to advance its
understanding of how to best address the growing impact of
cardiovascular disease,” said Craig Granowitz, M.D., Ph.D.,
Amarin’s senior vice president and chief medical officer. “At
Amarin, we share this passion and are pleased to provide additional
insights into how VASCEPA, with its unique effects, properties, and
attributes, can potentially reduce cardiovascular disease in
appropriate patients.”
Featured
Amarin-supported data presented
at AHA Virtual Scientific Sessions 2020
included:
1) Findings regarding
the unique mechanistic effects of the active ingredient in
VASCEPA:
“Eicosapentaenoic Acid, but Not Docosahexaenoic
Acid or a Mixed Omega-3 Fatty Acid Supplement, Inhibits Low-density
Lipoprotein Oxidation in a Time-dependent Manner” – presented
on behalf of all authors by Samuel Sherratt, B.S., Elucida
Research, Beverly, MA
Highlights: The purpose of the
study was to compare the effects of eicosapentaenoic acid (EPA)
versus docosahexaenoic acid (DHA) and a mixed omega-3 fatty acid
(EPA/DHA) dietary supplement on oxidation of human low-density
lipoprotein (LDL) in vitro.
EPA, a stable form of which is the active
ingredient in icosapent ethyl, in laboratory or in vitro study,
significantly inhibited LDL oxidation compared to a control vehicle
and did so over a more sustained period of time than DHA and mixed
omega-3 fatty acid. Inhibiting LDL is associated with lowering
cholesterol and oxidation of LDL is associated with making LDL
atherogenic. Evaluation was made based on quantifying changes in
malondialdehyde (MDA), a reactive aldehyde produced by LDL
oxidation.
In the study, EPA after 4 hours inhibited MDA
levels by 96% compared with the control vehicle oxidation level.
DHA compared with the control vehicle inhibited MDA levels at 2
hours at a level which was less pronounced than EPA and this level
of antioxidant activity with DHA was lost within 4 hours. The mixed
omega-3 fatty acid, which is a dietary supplement, failed to show
any antioxidant activity through 4 hours. Fatty acid analysis
showed that the mixed omega-3 fatty acid dietary supplement, which
is widely used commercially, in addition to EPA and DHA, contained
more than 30 other fatty acids, including saturated fats, that may
have nullified any potential benefits.
These data support LDL antioxidant effects of
EPA that were sustained over time compared with DHA, which had a
transient effect, or a mixed omega-3 fatty acid dietary supplement,
which had no beneficial effect at all.
“Contrasting Effects of Phospholipid Linked
Eicosapentaenoic Acid (EPA) and Arachidonic Acid (AA) on Membrane
Structure and Stability” – presented on behalf of all authors
by Samuel Sherratt, B.S., Elucida Research, Beverly, MA
Highlights: The purpose of this
in vitro study was to compare the separate and combined effects of
phospholipid-linked EPA and AA on membrane structure. Small angle
x-ray diffraction approaches compared the effects of
1-palmitoyl-2-eicosapentaenoyl-sn-glycero-3-phosphocholine (PL-EPA)
and 1-palmitoyl-2-arachidonoyl-sn-glycero-3-phosphocholine (PL-AA)
at a 1:20 ratio in membranes composed of
1-palmitoyl-2-oleoyl-sn-glycero-3-phosphocholine (POPC) and
cholesterol (C) at a 0.3:1 C:PL ratio.
PL-EPA was shown to cause membrane stability,
which may improve the signaling and function of endothelial cells.
The PL-EPA effect on improving membrane stability was negatively
disrupted by the presence of PL-AA. The contrasting effects of
PL-EPA and PL-AA on membrane structure may contribute to
differences in biological activity between these two omega-3 fatty
acid molecules, EPA and AA.
“Achieved Eicosapentaenoic Acid (EPA) Levels
Predicts Regression of Coronary Plaque Volumes by Coronary Computed
Tomography Angiography (CCTA) in the EVAPORATE Trial” –
presented on behalf of all authors by Suvasini Lakshmanan, M.D.,
M.S., Lundquist Institute at Harbor-UCLA Medical Center, Torrance,
CA
Highlights: EVAPORATE was a
randomized, double-blind, placebo-controlled trial enrolling a
total of 80 patients who had to have coronary atherosclerosis as
documented by multidetector computed tomography (MDCT) (1 or more
angiographic stenoses with ≥20% narrowing), be on statin therapy,
and have persistently elevated triglyceride (TG) levels. Patients
underwent an interim scan at 9 months and a final scan at 18 months
using Coronary Computed Tomography Angiography (CCTA) to evaluate
the effects of icosapent ethyl as an adjunct to statins on coronary
plaque volumes. The previously reported results of the prespecified
primary endpoint was a 17% regression in low attenuation plaque
(LAP) volume at 18 months for icosapent ethyl relative to placebo.
These results were previously presented with publication in the
European Heart Journal.
The pre-specified secondary endpoint was the
association of achieved serum EPA levels, and change in coronary
plaque volumes in the pooled cohort. At 18 months, higher serum EPA
levels were reported to predict regression of fibro-fatty plaque,
total non-calcified plaque (TNCP), and total plaque (TP), after
adjustment for age, sex, diabetes, hypertension, and baseline TG
levels.
“Effect of Icosapent Ethyl on Changes in
Coronary Plaque Characteristics at 9 Months in Patients With
Elevated Triglycerides on Statin Therapy: Insights From
EVAPORATE” – presented on behalf of all authors by Suvasini
Lakshmanan, M.D., M.S., Lundquist Institute at Harbor-UCLA Medical
Center, Torrance, CA
Highlights: In this analysis of
the EVAPORATE trial, plaque characteristics including lipid rich
necrotic core (LRNC), fibrous cap thickness, and intraplaque
hemorrhage (IPH) were assessed using vascuCAP® (Elucid Bioimaging
Inc., Boston, MA). A total of 60 patients had interpretable
images.
Relative to placebo, patients on icosapent ethyl
were reported to have decreased wall volume, LRNC, and IPH, as well
as increased cap thickness, indicating a migration to more stable
phenotypes. This study reported that icosapent ethyl, when added to
statin therapy, is associated with reduction in vulnerable plaque,
moving patients to a more stable plaque phenotype.
2) Findings further
supporting the robustness of the
clinical efficacy
demonstrated with VASCEPA:
“Icosapent Ethyl Reduces Ischemic Events in
Patients With Prior Coronary Artery Bypass Grafting: REDUCE-IT
CABG” – presented on behalf of all authors by Subodh Verma, M.D.,
Ph.D., University of Toronto, Toronto, Ontario, Canada
Highlights: VASCEPA, compared
with placebo, significantly reduced primary composite first and
total major adverse cardiovascular events (MACE) in post hoc
exploratory analyses of patients with a history of coronary artery
bypass grafting (CABG) procedures by 24% and 36%, respectively, and
key secondary composite first hard MACE, comprised of heart
attacks, stroke and cardiovascular death, by 31%.
As reported in a press release dated November
13, 2020, the REDUCE-IT® CABG analysis examined 1,837 (22.5%) of
the patients enrolled in REDUCE-IT, representing all patients who
had undergone a prior coronary artery bypass grafting (CABG)
procedure, a common form of surgical intervention to help treat
coronary heart disease. Baseline characteristics were similar among
patients randomized to VASCEPA versus placebo. Post hoc exploratory
analyses of this subgroup showed that, for the composite endpoint
of 5-point MACE, which was the prespecified primary endpoint for
the full REDUCE-IT study cohort, time to first event was
significantly reduced with VASCEPA versus placebo by 24% and total
(first and subsequent) events were also reduced by 36%. For the
REDUCE-IT study’s key secondary composite endpoint of 3-point MACE,
time to first event was reduced by 31% in the subgroup of patients
with a prior CABG.
“Significant Reductions in Both Adjudicated and
Investigator-Reported Ischemic Events in REDUCE-IT” –
presented on behalf of all authors by Deepak L. Bhatt, M.D.,
M.P.H., Brigham and Women’s Hospital, Boston, MA
Highlights: The REDUCE-IT
ADJUDICATION analysis sought to determine whether there were any
differences in the effect of icosapent ethyl whether endpoints were
investigator-reported or blindly adjudicated. Icosapent ethyl
significantly reduced primary and key secondary composite first
MACE by 26% and 25%, respectively, as reported by the site
investigators. There was a high degree of concordance between
investigator-reported and adjudicated endpoints, underscoring the
robustness of the cardiovascular benefits of icosapent ethyl seen
in REDUCE-IT.
3) Findings regarding
the cost-effectiveness of VASCEPA:
“Consistent Cost-effectiveness of Icosapent Ethyl Across Patient
Profiles From REDUCE-IT” – presented on behalf of all authors
by Zugui Zhang, Ph.D., ChristianaCare Health System, Newark, DE
Highlights: The purpose of this
study was to conduct subgroup analyses of lifetime
cost-effectiveness (CE) of icosapent ethyl (IPE) compared to
standard care (SC) alone. The analysis used cardiovascular event
reduction data demonstrated with IPE in the REDUCE-IT study and
third-party data regarding the cost associated with treating such
high-risk patients, including costs for treating heart attacks and
strokes if they are not reduced by IPE.
Based on the results of this analysis, IPE was
found to be a dominant strategy over the lifetime in 69.7% of
simulations with the probability of CE at the nominal $50,000,
$100,000, and $150,000 thresholds being replicated in 87.9%, 98.6%,
and 99.9% of simulations, respectively. Being a dominant strategy
means that not only is the therapy found to be cost-effective based
on typical quality-adjusted life year (QALY) criteria but also that
the therapy in most scenarios saves money for society. While the
REDUCE-IT study was not powered for subgroup analysis, CE analysis
was also conducted for subgroups of age, sex, diabetic status and
whether they were secondary or primary prevention patients at the
time of being enrolled into the REDUCE-IT study. In multiple
subgroups, IPE was reported to be a dominant strategy over
lifetime, in particular the subgroups of: age <65 years; male
sex; subjects with diabetes; subjects without diabetes; secondary
prevention cohort, TG levels ≥200 mg/dL; TG levels ≥150 mg/dL; and
baseline LDL ≥70 mg/dL. In multiple subgroups IPE was found to be
cost effective but did not reach the rarely achieved cost dominant
threshold. In subgroups for female sex and the primary prevention
cohort, IPE was found to be cost effective with an incremental cost
of $16,660 or $21,890 per QALY gained, respectively, which are both
well below the most stringent typical criteria for assessing
cost-effectiveness of medical therapy.
In all subgroups, IPE at the cost of therapy
used per the analysis per third-party reference was shown to be
cost effective at a willingness-to-pay threshold of $50,000 per
QALY and was a dominant treatment strategy in most subgroups.
4) Findings further
supporting the broad global need for
preventive cardiovascular
care:
“Are the Results of Clinical Trials Relevant in
the Real World? The Applicability of REDUCE-IT to the Fast-MI
Registry” – presented on behalf of all authors by Jean
Ferrières, M.D., M.Sc., Toulouse Rangueil University Hospital,
Toulouse, France
Highlights: In order to
evaluate the applicability of results of the REDUCE-IT
cardiovascular outcomes study in a segment of the French
population, the inclusion and exclusion criteria of the landmark
REDUCE-IT study were applied to French patients who were admitted
to coronary or intensive care units within 48 hours of symptom
onset during a 1-month period (French Registry on Acute
ST-elevation and non-ST-elevation Myocardial Infarction [FAST-MI],
2010 and 2015). The results support that, even in this limited
registry of patients, many French patients would qualify for the
inclusion criteria of REDUCE-IT in which patients treated with
VASCEPA experienced significant reductions in major adverse
cardiovascular events. These results were previously presented with
publication in Clinical Lipidology.
All analyses highlighted above were funded by
Amarin.
Additional information on AHA Virtual Scientific
Sessions 2020 can be found here.
Audio Webcast InformationAmarin
will host an audio webcast today, November 18, 2020, at 4:30 p.m.
EST to further discuss these and other VASCEPA-related findings
presented during the AHA Virtual Scientific Sessions 2020. The
discussion will include various clinicians and scientists and will
be moderated by Amarin’s chief medical officer, Craig Granowitz,
M.D., Ph.D. To listen please register here, listen live on the
investor relations section of the company's website at
www.amarincorp.com, or via telephone by dialing 877-407-8033 within
the United States, 201-689-8033 from outside the United States.
About Amarin Amarin Corporation
plc is a rapidly growing, innovative pharmaceutical company focused
on developing and commercializing therapeutics to cost-effectively
improve cardiovascular health. Amarin’s lead product, VASCEPA®
(icosapent ethyl), is available by prescription in the United
States, Canada, Lebanon and the United Arab Emirates. VASCEPA is
not yet approved and available in any other countries. Amarin, on
its own or together with its commercial partners in select
geographies, is pursuing additional regulatory approvals for
VASCEPA in China, Europe and the Middle East. For more information
about Amarin, visit www.amarincorp.com.
About Cardiovascular RiskThe
number of deaths in the United States attributed to cardiovascular
disease continues to rise. There are 605,000 new and 200,000
recurrent heart attacks per year (approximately 1 every 40
seconds), in the United States. Stroke rates are 795,000 per year
(approximately 1 every 40 seconds), accounting for 1 of every 19
U.S. deaths. Cardiovascular disease results in 859,000 deaths per
year in the United States.1 In aggregate, there are more than 2.4
million major adverse cardiovascular events per year from
cardiovascular disease or, on average, one every 13 seconds in the
United States alone.
Controlling bad cholesterol, also known as
LDL-C, is one way to reduce a patient’s risk for cardiovascular
events, such as heart attack, stroke or death. However, even with
the achievement of target LDL-C levels, millions of patients still
have significant and persistent risk of cardiovascular events,
especially those patients with elevated triglycerides. Statin
therapy has been shown to control LDL-C, thereby reducing the risk
of cardiovascular events by 25-35%.2 Significant cardiovascular
risk remains after statin therapy. People with elevated
triglycerides have 35% more cardiovascular events compared to
people with normal (in range) triglycerides taking
statins.3,4,5
About REDUCE-IT®REDUCE-IT was a
global cardiovascular outcomes study designed to evaluate the
effect of VASCEPA in adult patients with LDL-C controlled to
between 41-100 mg/dL (median baseline 75 mg/dL) by statin therapy
and various cardiovascular risk factors including persistent
elevated triglycerides between 135-499 mg/dL (median baseline 216
mg/dL) and either established cardiovascular disease (secondary
prevention cohort) or diabetes mellitus and at least one other
cardiovascular risk factor (primary prevention cohort).
REDUCE-IT, conducted over seven years and
completed in 2018, followed 8,179 patients at over 400 clinical
sites in 11 countries with the largest number of sites located
within the United States. REDUCE-IT was conducted based on a
special protocol assessment agreement with FDA. The design of the
REDUCE-IT study was published in March 2017 in Clinical
Cardiology.6 The primary results of REDUCE-IT were published in The
New England Journal of Medicine in November 2018.7 The total events
results of REDUCE-IT were published in the Journal of the American
College of Cardiology in March 2019.8 These and other publications
can be found in the R&D section on the company’s website at
www.amarincorp.com.
About
VASCEPA®
(icosapent ethyl)
CapsulesVASCEPA (icosapent ethyl) capsules are the
first-and-only prescription treatment approved by the FDA comprised
solely of the active ingredient, icosapent ethyl (IPE), a unique
form of eicosapentaenoic acid. VASCEPA was initially launched in
the United States in 2013 based on the drug’s initial FDA approved
indication for use as an adjunct therapy to diet to reduce
triglyceride levels in adult patients with severe (≥500 mg/dL)
hypertriglyceridemia. Since launch, VASCEPA has been prescribed
over eight million times. VASCEPA is covered by most major medical
insurance plans. The new, cardiovascular risk indication for
VASCEPA was approved by the FDA in December 2019.
Indications and Limitation of UseVASCEPA is
indicated:
- As an adjunct to maximally
tolerated statin therapy to reduce the risk of myocardial
infarction, stroke, coronary revascularization and unstable angina
requiring hospitalization in adult patients with elevated
triglyceride (TG) levels (≥ 150 mg/dL) and
- established cardiovascular disease
or
- diabetes mellitus and two or more
additional risk factors for cardiovascular disease.
- As an adjunct to diet to reduce TG
levels in adult patients with severe (≥ 500 mg/dL)
hypertriglyceridemia.
The effect of VASCEPA on the risk for
pancreatitis in patients with severe hypertriglyceridemia has not
been determined.
Important Safety Information
- VASCEPA is contraindicated in
patients with known hypersensitivity (e.g., anaphylactic reaction)
to VASCEPA or any of its components.
- VASCEPA was associated with an
increased risk (3% vs 2%) of atrial fibrillation or atrial flutter
requiring hospitalization in a double-blind, placebo-controlled
trial. The incidence of atrial fibrillation was greater in patients
with a previous history of atrial fibrillation or atrial
flutter.
- It is not known whether patients
with allergies to fish and/or shellfish are at an increased risk of
an allergic reaction to VASCEPA. Patients with such allergies
should discontinue VASCEPA if any reactions occur.
- VASCEPA was associated with an
increased risk (12% vs 10%) of bleeding in a double-blind,
placebo-controlled trial. The incidence of bleeding was greater in
patients receiving concomitant antithrombotic medications, such as
aspirin, clopidogrel or warfarin.
- Common adverse reactions in the cardiovascular outcomes trial
(incidence ≥3% and ≥1% more frequent than placebo): musculoskeletal
pain (4% vs 3%), peripheral edema (7% vs 5%), constipation (5% vs
4%), gout (4% vs 3%), and atrial fibrillation (5% vs 4%).
- Common adverse reactions in the hypertriglyceridemia trials
(incidence >1% more frequent than placebo): arthralgia (2% vs
1%) and oropharyngeal pain (1% vs 0.3%).
- Adverse events may be reported by
calling 1-855-VASCEPA or the FDA at 1-800-FDA-1088.
- Patients receiving VASCEPA and
concomitant anticoagulants and/or anti-platelet agents should be
monitored for bleeding.
Key clinical effects of VASCEPA on major adverse
cardiovascular events are included in the Clinical Studies section
of the prescribing information for VASCEPA as set forth below:
Effect of
VASCEPA on Time to First Occurrence of
Cardiovascular Events in Patients with Elevated
Triglyceride levels and Other Risk Factors for Cardiovascular
Disease in REDUCE-IT
|
|
VASCEPA |
Placebo |
VASCEPA vs Placebo |
|
N = 4089n (%) |
Incidence Rate (per 100 patient
years) |
N = 4090n (%) |
Incidence Rate (per 100 patient
years) |
Hazard Ratio (95% CI) |
|
Primary composite endpoint |
|
Cardiovascular death, myocardial infarction, stroke, coronary
revascularization, hospitalization for unstable angina (5-point
MACE) |
705(17.2) |
4.3 |
901(22.0) |
5.7 |
0.75(0.68, 0.83) |
|
Key secondary composite endpoint |
|
Cardiovascular death, myocardial infarction, stroke (3-point
MACE) |
459(11.2) |
2.7 |
606(14.8) |
3.7 |
0.74(0.65, 0.83) |
|
Other secondary endpoints |
|
Fatal or non-fatal myocardial infarction |
250(6.1) |
1.5 |
355(8.7) |
2.1 |
0.69(0.58, 0.81) |
|
Emergent or urgent coronary revascularization |
216(5.3) |
1.3 |
321(7.8) |
1.9 |
0.65(0.55, 0.78) |
|
Cardiovascular death [1] |
174(4.3) |
1.0 |
213(5.2) |
1.2 |
0.80(0.66, 0.98) |
|
Hospitalization for unstable angina [2] |
108(2.6) |
0.6 |
157(3.8) |
0.9 |
0.68(0.53, 0.87) |
|
Fatal or non-fatal stroke |
98(2.4) |
0.6 |
134(3.3) |
0.8 |
0.72(0.55, 0.93) |
|
[1] Includes adjudicated cardiovascular deaths and deaths of
undetermined causality.[2] Determined to be caused by myocardial
ischemia by invasive/non-invasive testing and requiring emergent
hospitalization. |
FULL VASCEPA
PRESCRIBING INFORMATION CAN BE FOUND
AT
WWW.VASCEPA.COM.
Forward-Looking Statements This
press release contains forward-looking statements, including
statements regarding the potential impact of VASCEPA in various
clinical uses. These forward-looking statements are not promises or
guarantees and involve substantial risks and uncertainties. Among
the factors that could cause actual results to differ materially
from those described or projected herein include the following:
uncertainties associated generally with research and development
and clinical trials such as further clinical evaluations failing to
confirm earlier findings. A further list and description of these
risks, uncertainties and other risks associated with an investment
in Amarin can be found in Amarin's filings with the U.S. Securities
and Exchange Commission, including its most recent Quarterly Report
on Form 10-Q. Existing and prospective investors are cautioned not
to place undue reliance on these forward-looking statements, which
speak only as of the date hereof. Amarin undertakes no obligation
to update or revise the information contained in this press
release, whether as a result of new information, future events or
circumstances or otherwise. Amarin’s forward-looking statements do
not reflect the potential impact of significant transactions the
company may enter into, such as mergers, acquisitions,
dispositions, joint ventures or any material agreements that Amarin
may enter into, amend or terminate.
Availability of Other Information About
AmarinInvestors and others should note that Amarin
communicates with its investors and the public using the company
website (www.amarincorp.com), the investor relations website
(investor.amarincorp.com), including but not limited to investor
presentations and investor FAQs, Securities and Exchange Commission
filings, press releases, public conference calls and webcasts. The
information that Amarin posts on these channels and websites could
be deemed to be material information. As a result, Amarin
encourages investors, the media, and others interested in Amarin to
review the information that is posted on these channels, including
the investor relations website, on a regular basis. This list of
channels may be updated from time to time on Amarin’s investor
relations website and may include social media channels. The
contents of Amarin’s website or these channels, or any other
website that may be accessed from its website or these channels,
shall not be deemed incorporated by reference in any filing under
the Securities Act of 1933.
Amarin Contact
InformationInvestor Inquiries:Investor RelationsAmarin
Corporation plcIn U.S.: +1 (908) 719-1315IR@amarincorp.com
(investor inquiries)
Solebury Troutlstern@soleburytrout.com
Media Inquiries:Alina
KolomeyerCommunicationsAmarin Corporation plcIn U.S.: +1 (908)
892-2028 PR@amarincorp.com (media inquiries)
1 American Heart Association. Heart Disease and
Stroke Statistics—2020 Update: A Report From the American Heart
Association. Circulation. 2020;141:e139–e596.2 Ganda OP,
Bhatt DL, Mason RP, et al. Unmet need for adjunctive dyslipidemia
therapy in hypertriglyceridemia management. J Am Coll Cardiol.
2018;72(3):330-343.3 Budoff M. Triglycerides and
triglyceride-rich lipoproteins in the causal pathway of
cardiovascular disease. Am J Cardiol.
2016;118:138-145.4 Toth PP, Granowitz C, Hull M, et al.
High triglycerides are associated with increased cardiovascular
events, medical costs, and resource use: A real-world
administrative claims analysis of statin-treated patients with high
residual cardiovascular risk. J Am Heart Assoc.
2018;7(15):e008740.5 Nordestgaard BG. Triglyceride-rich
lipoproteins and atherosclerotic cardiovascular disease - New
insights from epidemiology, genetics, and biology. Circ Res.
2016;118:547-563.6 Bhatt DL, Steg PG, Brinton E, et al.,
on behalf of the REDUCE-IT Investigators. Rationale and Design of
REDUCE‐IT: Reduction of Cardiovascular Events with Icosapent
Ethyl–Intervention Trial. Clin Cardiol.
2017;40:138-148.7 Bhatt DL, Steg PG, Miller M, et al.,
on behalf of the REDUCE-IT Investigators. Cardiovascular Risk
Reduction with Icosapent Ethyl for Hypertriglyceridemia. N Engl J
Med. 2019;380:11-22.8 Bhatt DL, Steg PG, Miller M, et
al., on behalf of the REDUCE-IT Investigators. Reduction in first
and total ischemic events with icosapent ethyl across baseline
triglyceride tertiles. J Am Coll Cardiol. 2019;74:1159-1161.
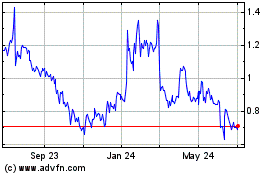
Amarin (NASDAQ:AMRN)
Historical Stock Chart
From Mar 2024 to Apr 2024
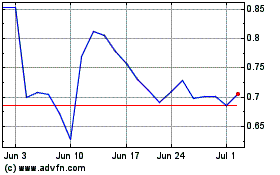
Amarin (NASDAQ:AMRN)
Historical Stock Chart
From Apr 2023 to Apr 2024