By Melanie Evans
Hospitals are holding off as long as possible before halting
procedures to make room for fresh waves of Covid-19 patients, a
reversal from earlier this year when facilities postponed care,
leading to steep financial losses and public-health risks.
National hospital chain Tenet Healthcare Corp. pushed ahead with
procedures as states permitted, such as knee and hip replacements,
colonoscopies, and surgery to implant pacemakers, through recent
surges in Alabama, California and elsewhere. In southeast
Wisconsin, where already rising Covid-19 hospitalizations jumped
35% in the first two weeks of the month, Advocate Aurora Health
continues nonessential surgery across a dozen hospitals.
HCA Healthcare Inc., one of the nation's largest hospital
systems, waited until last week to suspend some surgery in El Paso,
Texas, where a coronavirus surge sharply accelerated in recent
weeks. About 80% of the procedures there continue, however.
Nashville-based HCA stops surgery "as a last resort," said Jon
Foster, an HCA president who oversees 90 of the company's 186
hospitals.
Hospitals have grown more circumspect of shutdowns through new
waves of the virus after fallout from voluntary and state-ordered
shutdowns in March and April. And unlike last spring, fewer states
are ordering broad shutdowns, leaving it to hospitals.
Earlier this year, facilities postponed nonessential surgeries,
such as knee and hip replacements and cancer screenings. Hospital
and clinic revenue plummeted. The widespread halt to procedures led
to an average 30% to 40% drop in nonprofit hospital revenue,
Moody's Investors Service reported in May, as hospitals began to
resume surgery. During the second quarter -- the period in which
most of the surgical delays occurred -- the median for-profit
hospital revenue dropped 10%, the ratings agency said.
Health-care job losses followed, as did $175 billion in federal
spending for relief. Patients grew anxious, and some saw their
medical conditions worsen during delays.
Months later, hospitals have learned from previous surges to
better manage capacity, avoid temporarily halts in services and
rebound quickly from disruption, hospital executives said. Halting
surgery is also not as critical to preserve supplies, with
expanding production of protective equipment and testing
capacity.
"We realize and operate every day with the assumption that Covid
spikes will be part of what we face until a vaccine becomes widely
deployed," Tenet Chief Executive Ron Rittenmeyer said on a call
with analysts last week. "There is no perfect equation. But we do
believe our learnings from each spike improves our responsiveness,
our planning and furthers our effectiveness."
Tenet uses public-health data to monitor for an imminent influx
of Covid-19 patients, and its hospitals typically see surges crest
and begin to subside within four to six weeks, Saum Sutaria, the
company's president, told analysts.
The company now moves swiftly to resume typical operations on
that schedule, Dr. Sutaria said. "We have not had, especially in
recent surges, any need to shut down procedures or elective
surgeries, that's a very important point because we want to
maintain access for the community," he said. "And then as those
cases ramp back down, you know, we ramp back up very, very
quickly."
Many scheduled procedures are common and profitable, and the
loss of that business for weeks earlier this year drained
hospitals' cash reserves. The sector received an influx of federal
aid and loans and has rebounded more quickly than first expected,
however.
HCA monitors local coronavirus case trends and hospital data
including occupancy rates, health-care staff levels and stock of
critical supplies. Color-coded warnings on a dashboard used by HCA
management show markets where surge risk is rising, said Mr.
Foster, the HCA executive.
Local hospital officials also weigh in on the need for more
nurses, doctors, ventilators or other critical supplies. They relay
what they see to corporate headquarters, where executives use
experiences from multiple surges across the country to inform
decisions.
"The net effect of that is they are better able to manage
capacity and therefore defer as long as possible these decisions to
delay or to have to reschedule certain scheduled cases," Mr. Foster
said.
Health-care staff are often critical to meet rising Covid-19
demand without shuttering other services, he said. HCA has 70
nurses at or en route to its two hospitals in El Paso, Texas, and
has another 40 nurses waiting to be deployed. A surge that began in
September but rapidly accelerated this month didn't compel local
hospital executives to postpone surgery until last week, when they
scaled back a limited number of the least-urgent cases, Mr. Foster
said.
Hospital discretion over when to postpone surgery is a switch
from earlier this year, when more than 30 states ordered hospitals
to halt nonessential surgeries. Governors began to roll back
restrictions in late April, but some continue to intervene as the
pandemic flares.
Texas Gov. Greg Abbott in late June ordered hospitals in a
handful of hard-hit counties to halt some procedures, expanding the
temporary restrictions as the state's surge continued.
Other states set no requirements, including Wisconsin, where the
latest state data show the seven-day average hospital
intensive-care Covid-19 patients climbing steadily to reach around
86% occupancy. In June, when the state's Covid-19 hospitalizations
were largely stable, ICU occupancy was about 74% to 77%.
Advocate Aurora, which operates 16 Wisconsin hospitals, hasn't
postponed procedures and has no fixed, statewide threshold for when
to do so, said Jeff Bahr, chief Aurora medical group officer. "A
broad, general overarching rule fails to take into account the
necessary variations from community to community," Dr. Bahr
said.
The system is bringing nurses from its Illinois hospitals to
help in Wisconsin, where it can also transfer patients from crowded
hospitals to those without as many patients. "We are able to
coexist in the midst of Covid," he said.
Advocate Aurora saw hospitalizations drop about 9% during the
first six months of the year compared with the same period in 2019.
Last year's $314 million operating profit in the first half of the
year also evaporated, the system's financial statements show.
Advocate Aurora lost $246 million on operations through June of
this year. It has so far received about $362 million in federal
aid.
Hospitals cannot entirely avoid postponing surgeries as the
pandemic repeatedly surges across the U.S.
Waves of hospitalizations across the South and West this summer
prompted HCA to voluntarily halt electives across about 60% of its
markets, including Florida, Georgia, South Carolina, Tennessee and
Texas. Procedures have since resumed. The simultaneous surge across
so many markets left the company with fewer unaffected hospitals
able to redeploy extra staff to hard-hit areas, Mr. Foster
said.
The Billings Clinic in Montana began in late September to
evaluate each surgical case for urgency and is postponing those
that can wait. Operations have dropped about 10% since.
Billings Clinic's flagship hospital, located in Billings, is now
transferring patients daily to more than a dozen smaller hospitals
nearby to make room for urgent and emergency procedures, Chief
Executive Scott Ellner said.
How long that will remain an option is unclear. Open beds are
dwindling, he said. "They are starting to be stretched."
Write to Melanie Evans at Melanie.Evans@wsj.com
(END) Dow Jones Newswires
October 26, 2020 09:07 ET (13:07 GMT)
Copyright (c) 2020 Dow Jones & Company, Inc.
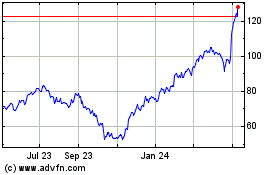
Tenet Healthcare (NYSE:THC)
Historical Stock Chart
From Mar 2024 to Apr 2024
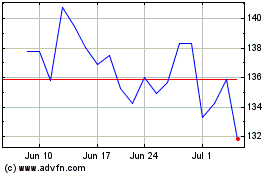
Tenet Healthcare (NYSE:THC)
Historical Stock Chart
From Apr 2023 to Apr 2024