By Joseph Walker, Peter Loftus and Jared S. Hopkins
For drug companies, there is suddenly only one priority: the
coronavirus.
More than 140 experimental drug treatment and vaccines for the
coronavirus are in development world-wide, most in early stages but
including 11 already in clinical trials, according to Informa
Pharma Intelligence.
Counting drugs approved for other diseases, there are 254
clinical trials testing treatments or vaccines for the virus, many
spearheaded by universities and government research agencies, with
hundreds more trials planned. Researchers have squeezed timelines
that usually total months into weeks or even days.
"We have never gone so fast with so many resources in such a
short time frame," said Paul Stoffels, chief scientific officer of
Johnson & Johnson.
Even so, for most treatments and vaccines it will be midsummer
before human testing reveals whether they are safe to take, not to
mention if they work. J&J is excited about a vaccine prospect
but won't be able to start testing it in humans until September.
Research progress that is remarkable by usual standards remains far
behind the racing virus.
Health officials are warning Americans to brace for the most
difficult days this week, with the number of infections in the
nation's hardest hit cities expected to peak. More than 1.2 million
people have been infected around the globe as of Sunday, according
to data compiled by Johns Hopkins University. In the U.S., more
than 9,400 people have died from Covid-19, the respiratory disease
caused by the coronavirus. The White House projects the U.S. could
see 100,000 to 240,000 deaths from Covid-19.
Vaccines to prevent infections and drugs to treat them can't
come soon enough. Without them, health authorities have had to rely
on containment measures such as travel bans and social distancing,
while doctors sometimes give patients unproven agents with the hope
they will work.
It usually takes years to develop a new drug treatment or
vaccine. After finding prospects, researchers must tweak them to
maximize their disease-fighting potency and minimize the risk of
unwanted side effects. The compounds must be tested in the lab, in
animals and extensively in humans. If they succeed, more time is
needed to manufacture large numbers of doses.
The urgent, high-speed search is moving on three fronts. One is
to get a vaccine that could provide immunity, allowing a return to
normalcy.
Among the farthest along is a vaccine hatched by government
researchers and Moderna Inc., a biotechnology company in Cambridge,
Mass., for which safety testing in humans has begun. If this and
all later clinical studies succeed, it could be ready for use as
soon as early next year, researchers say.
In addition, Inovio Pharmaceuticals Inc. of Plymouth Meeting,
Pa., said human trials are starting today for an experimental
vaccine it is developing. Chinese company CanSino Biologics Inc.
and a research arm of the Chinese military have started human
testing of a potential vaccine, according to the World Health
Organization. In Europe, German company CureVac AG and the
University of Oxford are developing vaccines.
Scientists also are exploring whether existing drugs such as
hydroxychloroquine for malaria or HIV treatments might work against
the coronavirus, and some doctors are already treating patients
with hydroxychloroquine. Results from two Chinese studies of Gilead
Sciences Inc.'s antiviral remdesivir, previously tested in Ebola,
are expected this month. Regeneron Pharmaceuticals Inc, and partner
Sanofi SA are testing a rheumatoid arthritis drug against the
coronavirus.
On the third front, researchers are hunting for entirely new
drugs. Among these efforts, which take longer, are programs to mine
the blood of recovered patients for infection-fighting soldiers
known as antibodies that can be converted into drugs.
All drug and vaccine research is difficult, but tackling a virus
can be especially tricky. Tweaking the immune system, as some drugs
and vaccines targeting infectious diseases aim to do, risks sending
the immune response into overdrive and making things even worse. It
can take researchers several tries to find more powerful
agents.
"I think we can find something that, at least, helps people
out," said Derek Lowe, a veteran drug researcher. "Whether any of
these things work well enough to get people out of their houses,
that's another question. Maybe it works well enough to reduce the
number of people who go on ventilators."
Johnson & Johnson said it and a division of the Department
of Health and Human Services together have committed more than $1
billion of investment to co-fund vaccine research, development, and
clinical testing. Other government agencies and universities are
also spending on research.
Unlike the race to find cures for cancer or other diseases,
there's not necessarily a big payoff at the finish. Companies
haven't indicated what they might charge for medicines if they
work; some have said they'll provide drugs free or at low cost.
Gilead said Saturday it won't charge for 1.5 million doses it has
manufactured for clinical trials and emergency uses, or any
remainder if the drug is approved.
Scenes from several laboratories show the quest from the
inside.
One weekend in January, Kizzmekia Corbett rushed to Building 40
on the National Institutes of Health campus in Bethesda, Md.
Dr. Corbett is a researcher at the National Institute of Allergy
and Infectious Diseases, or NIAID. For years, she and colleagues
have braced for a pandemic, studying bacteria and viruses that
popped up around the world to gain a better understanding when a
bad one finally came.
Around Jan. 10, she got a cellphone alert with a vital piece of
information about a mysterious virus emerging in China. A
consortium of researchers including Chinese scientists had
published online the virus's genetic sequence.
That provided its molecular makeup, crucial information needed
to craft a vaccine for it. The research also indicated the new
virus belonged to a well-known family, the coronaviruses.
Named for the crown-like spikes protruding from their surface,
coronaviruses had caused two deadly outbreaks since 2002: severe
acute respiratory syndrome, or SARS, and Middle East Respiratory
Syndrome, MERS.
Dr. Corbett and a colleague studied the genetic code --
seemingly endless combinations of the letters A, G, C and T, each
standing for the chemicals comprising DNA. The sequence looked
similar to that of the SARS virus. This meant researchers who had
investigated a SARS vaccine, which didn't advance after the
epidemic waned, could pursue a similar tack against the new
coronavirus.
A vaccine would deliver a disabled spike protein, or the genetic
instructions to make a close copy, into the human body. The payload
wouldn't infect a person but would train the immune system to
recognize and attack the virus. If a vaccinated person encountered
the virus, antibodies would spring into action and neutralize
it.
"We're lucky that this is a coronavirus because we know what to
do. It would be a much worse situation" if the virus belonged to a
less-studied family, said Barney Graham, deputy director of the
Vaccine Research Center at NIAID.
As the virus spread in Wuhan, China, and then in other
countries, U.S. government researchers searched for a partner to
help design and make a vaccine. Dr. Graham reached out to one his
team previously worked with, at Moderna, which is pioneering a new
technology for making vaccines. It uses "messenger" RNA, genetic
material that can instruct cells to make proteins able to trigger
immune responses.
Like the NIH, Moderna researchers studied the new virus's
genetic sequence when it was published. They, too, concluded the
spike protein would be the best part to target. So did vaccine
hunters at J&J, Sanofi and other companies.
By Monday, Jan. 13, the NIAID and Moderna agreed on a vaccine
design. Moderna quickly made a small batch for testing. Dr. Corbett
and colleagues started testing it in mice on Feb. 4. Two weeks
later, initial results showed it elicited antibodies to coronavirus
in the blood.
Success in mice often doesn't mean a similar result in people.
Months of testing in humans would be necessary. Moderna retrofitted
equipment at its manufacturing plant outside Boston, and by Feb. 25
the NIAID was ready to recruit healthy volunteers. In the past, it
has usually taken many months for an experimental vaccine to start
human testing after selection of a target.
One morning the following month, George Yancopoulos, chief
scientific officer at Regeneron in Tarrytown, N.Y., texted his head
of infectious disease research. "Good luck today," he wrote. "The
world is sort of maybe depending on you ;)."
It was 8:41 a.m. on Saturday, March 14, the latest in a string
of weekends consumed by the company's hunt for a medicine that
could knock out the virus in someone it had infected.
Spearheading the efforts was Christos Kyratsous, drug-discovery
chief for infectious diseases, who used a rapid-response platform
the company had formed after the 2014 Ebola epidemic in West
Africa.
His team collaborated with colleagues who tended some special
mice with immune systems genetically engineered to have a
human-like response to viruses. Because the mice make antibodies
indistinguishable from people's, researchers working with the mice
can have a compound ready to test in people in months rather than
the years it takes to birth a traditional drug from scratch.
The teams had spent weeks collecting antibodies from mice
exposed to the coronavirus's spike protein, in hopes that two of
the antibody molecules could be combined into a drug able to stop
an infection. They also gathered antibodies from the blood of
recovered coronavirus patients.
Experiments to see whether these killed the virus in test tubes
were being finished up that March Saturday.
"You can come now," Dr. Kyratsous texted Dr. Yancopoulos at 2:45
p.m. Dr. Yancopoulos got off a conference call and walked to the
lab. As he entered the lab and saw Dr. Kyratsous smiling, he texted
a colleague to bring a bottle of champagne.
Data showed they had found hundreds of antibodies that blocked
the virus from entering cells. If it couldn't enter cells, it
couldn't replicate. A treatment was still far away -- but now was
in sight. The champagne popped open.
"My head was in a rush: 'We've got it,' " Regeneron Chief
Executive Leonard Schleifer recalls thinking after his chief
scientific officer gave him the details. "The world is starting to
fall apart, and if we can just hold on, in that lab, in those
tubes, is a cure."
Within days, Regeneron announced it would choose the best two
antibodies for a drug in April and would start clinical trials by
early summer. It is preparing to manufacture hundreds of thousands
of doses a month by the end of the summer.
Getting the drug on the market isn't assured. Clinical trials
showing the treatment is both effective and safe could take months.
These are the stages where so many medicines fail even after they
show promising test-tube and animal results.
Neal Browning was scrolling through his Facebook feed in early
March when a friend's post caught his eye.
Mr. Browning is a network engineer at Microsoft Corp. living in
the Seattle suburb of Bothell, Wash., not far from one of the
country's earliest and worst coronavirus outbreaks. He also lives
close to the research center doing a human study of the vaccine
that Moderna and the NIAID are developing.
The research center, Kaiser Permanente Washington Health
Research Institute, was urgently seeking healthy volunteers to test
the experimental vaccine's safety. Mr. Browning's Facebook friend
knew of the recruitment effort. After Mr. Browning expressed
concern about the virus, the friend texted him details of the
trial.
Many medical facilities across the U.S. are seeking people to
test the safety of potential coronavirus drugs or vaccines. To make
way, they are suspending trials of other medicines, clearing space
for coronavirus study subjects and assigning data-entry workers,
pharmacists and other staff to deal with the paperwork.
Massachusetts General Hospital, one day after agreeing to test
Gilead's remdesivir, walked federal health officials through how it
planned to conduct the trial. It did so by phone for safety reasons
and because time was short, said Libby Hohmann, who oversees the
hospital's clinical-trial effort.
That evening, Dr. Hohmann assembled about a dozen pharmacists,
researchers and physicians in a conference room to parcel out
trial's tasks, such as collecting blood samples and tracking
patients once discharged.
To save time, they skipped typical pretrial exercises such as
training the staff in showing hospital doctors and nurses the way
to administer the drug. "We're sort of doing those on the fly," Dr.
Hohmann said.
Since the trial began March 15, Mass General has enrolled 35
subjects. Among them is a man in his 40s who agreed to be in the
study just before nurses inserted a breathing tube down his throat
because of respiratory problems from the virus, Dr. Hohmann said.
He is now stable, she said.
For the test of Moderna's vaccine, Mr. Browning, the Microsoft
engineer, showed up at the Kaiser research institute in downtown
Seattle on March 16, becoming only the second volunteer.
It had been just nine weeks since researchers selected a section
of the virus's genetic sequence to target, which researchers called
the shortest time by at least a month to get a vaccine into the
first stage of human testing. Even so, the trial is unlikely to
have preliminary results until summer, followed by more testing
required that would push the vaccine's availability out about 12 to
18 months, according to the NIAID.
After his shot, Mr. Browning stayed for about an hour so the
staff could make sure he didn't have any side effects. He drove
home and worked that afternoon helping Microsoft configure network
firewalls to accommodate a surge in employees working remotely,
until the threat posed by the virus can be quashed.
(END) Dow Jones Newswires
April 06, 2020 12:26 ET (16:26 GMT)
Copyright (c) 2020 Dow Jones & Company, Inc.
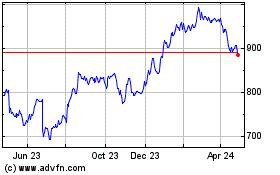
Regeneron Pharmaceuticals (NASDAQ:REGN)
Historical Stock Chart
From Mar 2024 to Apr 2024
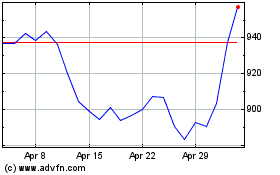
Regeneron Pharmaceuticals (NASDAQ:REGN)
Historical Stock Chart
From Apr 2023 to Apr 2024