Humana to Waive Medical Costs Related to Coronavirus Treatment
March 30 2020 - 7:58AM
Dow Jones News
By Michael Dabaie
Humana Inc. said it is waiving consumer costs for treatment
related to Covid-19-covered services.
The provider of health insurance services had previously said
that it would cover out-of-pocket costs related to coronavirus
testing. Now, costs related to subsequent treatment for Covid-19,
including inpatient hospital admissions, will be waived for
enrollees of Medicare Advantage plans, fully insured commercial
members, Medicare Supplement and Medicaid, Humana said.
The waiver applies to all medical costs related to treatment of
Covid-19, as well as FDA-approved medications or vaccines when they
become available. Humana said there is no current end date and it
will reassess as circumstances change.
Humana said it will cover member responsibility under the plan
benefits for Covid-19-related services whether treatment is
delivered by in-network or out-of-network providers.
The company said it is also lifting administrative requirements
for members infected with coronavirus and for all patients in
settings where capacity is stretched by the needs of those infected
by coronavirus. The company said it is waiving member cost-share
for all telehealth services delivered by participating in-network
providers and accepting audio-only telephone visits for
reimbursement.
Write to Michael Dabaie at michael.dabaie@wsj.com
(END) Dow Jones Newswires
March 30, 2020 07:43 ET (11:43 GMT)
Copyright (c) 2020 Dow Jones & Company, Inc.
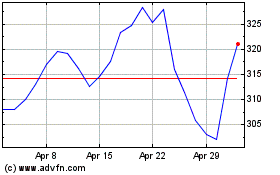
Humana (NYSE:HUM)
Historical Stock Chart
From Mar 2024 to Apr 2024
Humana (NYSE:HUM)
Historical Stock Chart
From Apr 2023 to Apr 2024
