By Melanie Evans and Anna Wilde Mathews
Black patients were less likely than white patients to get extra
medical help, despite being sicker, when an algorithm used by a
large hospital chose who got the additional attention, according to
a new study underscoring the risks as technology gains a foothold
in medicine.
Hospitals use the algorithm -- from Optum, UnitedHealth Group
Inc.'s health-services arm -- to find patients with diabetes, heart
disease and other chronic ailments who could benefit from having
health-care workers monitor their overall health, manage their
prescriptions and juggle doctor visits, according to the study
published Thursday in the journal Science.
Yet the algorithm gave healthier white patients the same ranking
as black patients who had one more chronic illness as well as
poorer laboratory results and vital signs.
The reason? The algorithm used cost to rank patients, and
researchers found health-care spending for black patients was less
than for white patients with similar medical conditions.
"What the algorithm is doing is letting healthier white patients
cut in line ahead of sicker black patients," said Dr. Ziad
Obermeyer, the study's lead author and an acting associate
professor of health policy at the University of California,
Berkeley.
Optum advises its customers that its predictive algorithms
shouldn't replace physician judgment, a company spokesman said.
Efforts to use analytics in health care have only scratched the
surface of their potential and should be continually reviewed and
refined, he said.
Optum's algorithm is used by more than 50 organizations,
according the company's website. Partners Healthcare in Boston is
among those to have used it, according to published research. A
Partners spokesman said the hospital system is vigilant about how
well its algorithms perform. He added a Partners researcher
co-authored the paper, which "is an important step in rooting out
some of the flaws that exist."
The Washington Post and Science News earlier reported Optum is
the algorithm's developer.
Algorithms, developed by computers crunching vast data sets, are
increasingly shaping choices in medicine, from interpreting medical
scans to predicting who might become addicted to opioids, suffer a
dangerous fall or end up in the hospital.
The technology can speed up and improve some decisions, leading
to better treatment for patients, supporters say. But doctors who
get suggestions to tweak their patients' care based on the findings
of algorithms often don't know the details of the technology that
led to the recommendation.
Poorly designed algorithms risk reinforcing racial and gender
biases, technology experts caution, as studies of algorithms in
nonmedical settings like credit scoring, hiring and policing have
found.
Algorithms "can give the gloss of being very data-driven, when
in fact there are a lot of subjective decisions that go into
setting up the problem in the first place," said Solon Barocas, an
assistant professor at Cornell University who is also a principal
researcher at Microsoft Research.
Researchers behind the study said well-designed algorithms could
help reduce bias that leads to wide disparities in health-care
outcomes and access to care. They created an alternative algorithm
that increased the percentage of those identified for extra help
who were black to about 47%, up from 18%.
"It's a tool that can do a great deal of good and a great deal
of bad, it merely depends on how we use the tool," said Sendhil
Mullainathan, a University of Chicago computational science
professor who was an author of the study.
Hospitals and health insurers across the U.S. use the Optum
algorithm to spot patients who could benefit from extra help from
nurses, pharmacists and case workers, the authors of the study
said.
To identify those with the biggest medical needs, the algorithm
looks at patients' medical histories and how much was spent
treating them, and then predicts who is likely to have the highest
costs in the future.
For the study, data-science researchers looked at the
assessments made by one hospital's use of the algorithm. The study
didn't name the hospital. The researchers focused on the
algorithm's rankings of 6,079 patients who identified themselves as
black in the hospital's records, and 43,539 who identified as white
and didn't identify themselves as any other race or ethnicity.
Then the researchers assessed the health needs of the same set
of patients using their medical records, laboratory results and
vital signs, and developed a different algorithm.
Using that data, the researchers found that black patients were
sicker than white patients who had a similar predicted cost. Among
those rated the highest priority by the hospital's algorithm, black
patients had 4.8 chronic diseases compared with 3.8 of the
conditions among white patients.
The researchers found the number of black patients eligible for
fast-track enrollment in the program more than doubled by
prioritizing patients based on their number of chronic conditions,
rather than ranking them based on cost.
The findings show "how a seemingly benign choice of label (that
is, health cost) initiates a process with potentially
life-threatening results," Ruha Benjamin, author of "Race After
Technology" and an associate African-American studies professor at
Princeton University, said in an accompanying commentary in
Science.
Algorithms are playing an increasing role in medicine, though
largely invisible to patients.
Doctors are using algorithms to read scans for lung cancer, for
instance. Hospitals are deploying the technology to spot which
critically ill patients are likely to worsen dramatically.
Meantime, health insurers are using algorithms for reasons
including to detect patients who are at risk of opioid addiction or
who appear headed toward costly lower-back surgery.
Alan Muney, a former executive at health insurer Cigna Corp.,
said it is common for insurers to use the projected cost of care as
a focus in selecting who might get extra outreach or support.
"It's troubling there was such a big difference" in the effects
for black and white patients based on an algorithm focused on cost,
he said.
Insurers are developing algorithms that include variables beyond
medical costs, including issues that might signal barriers to
accessing care, such as financial stress and food insecurity, he
said.
Write to Melanie Evans at Melanie.Evans@wsj.com and Anna Wilde
Mathews at anna.mathews@wsj.com
(END) Dow Jones Newswires
October 25, 2019 08:54 ET (12:54 GMT)
Copyright (c) 2019 Dow Jones & Company, Inc.
UnitedHealth (NYSE:UNH)
Historical Stock Chart
From Mar 2024 to Apr 2024
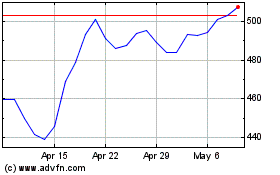
UnitedHealth (NYSE:UNH)
Historical Stock Chart
From Apr 2023 to Apr 2024
