FTC to Study Pharmacy Benefit Manager Practices
June 07 2022 - 2:28PM
Dow Jones News
By Kathryn Hardison
The Federal Trade Commission on Tuesday said it will launch an
inquiry into the prescription drug middleman industry to weigh the
impact that vertically-integrated pharmacy benefit managers have on
the accessibility and affordability of prescription drugs.
The FTC said it is requiring the six largest pharmacy benefit
managers, which negotiate rebates and fees with drug manufacturers,
provide records and information related to their business
practices. The compulsory orders are being sent to CVS Caremark,
Express Scripts Inc., OptumRx Inc., Humana Inc., Prime Therapeutics
LLC and MedImpact Healthcare Systems Inc., the FTC said
Pharmacy benefit managers also reimburse pharmacies for
patients' prescriptions and create drug formularies--a list of
prescription drugs that are paid for by a health plan--and other
policies, the FTC said. The largest pharmacy benefit managers are
vertically-integrated with health insurance companies and
wholly-owned mail order and specialty pharmacies, which the FTC
said gives the managers a large influence on what patients pay for
their prescriptions and where they purchase them.
"Although many people have never heard of pharmacy benefit
managers, these powerful middlemen have enormous influence over the
U.S. prescription drug system," FTC Chairwoman Lina Khan said.
"This study will shine a light on these companies' practices and
their impact on pharmacies, payers, doctors, and patients."
The inquiry will also look into the use of specialty drug lists
and related specialty drug policies. The FTC said it has received
more than 24,000 public comments about pharmacy benefit
managers.
Write to Kathryn Hardison at kathryn.hardison@wsj.com
(END) Dow Jones Newswires
June 07, 2022 14:13 ET (18:13 GMT)
Copyright (c) 2022 Dow Jones & Company, Inc.
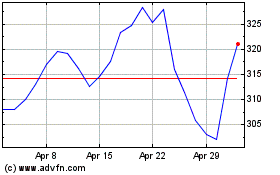
Humana (NYSE:HUM)
Historical Stock Chart
From Mar 2024 to Apr 2024
Humana (NYSE:HUM)
Historical Stock Chart
From Apr 2023 to Apr 2024
