CVS Gives Downbeat Earnings Outlook for First Year as Merged Company -- 3rd Update
February 20 2019 - 2:07PM
Dow Jones News
By Anna Wilde Mathews and Aisha Al-Muslim
CVS Health Corp. offered a downbeat earnings projection for
2019, its first year as a merged health-care company, saying
results would be dragged down by challenges in areas including its
pharmacy-benefits and long-term-care businesses.
The Woonsocket, R.I.-based company, which in November completed
its nearly $70 billion acquisition of insurer Aetna Inc., said that
it was taking rapid steps to address the problems, including a
cost-cutting effort, and that its ambitious deal positioned it for
long-term growth.
CVS, which has said that its deal to bring together drugstores,
pharmacy-benefit management and insurance would help it cut
health-care costs and improve care, said it was building new
offerings.
For 2019, the company said it was projecting adjusted earnings
per share of $6.68 to $6.88, compared with analysts' estimates of
$7.41 a share, as polled by Refinitiv. CVS said its results are
being hurt by factors including smaller benefits from the rollout
of new generic drugs and the performance of Omnicare, its
long-term-care pharmacy business.
In its pharmacy-benefits business, CVS said it was experiencing
a squeeze related to rebates that it receives from drugmakers and
passes on to clients. It has guaranteed clients that it will
provide them certain rebate payments, but it is seeing slower
growth than it had expected in the prices of branded drugs. CVS
said it also will lose the PBM business of Centene Corp., beginning
in 2019.
"Many of these headwinds are transitory in nature," CVS Chief
Executive Larry Merlo said in a call with analysts. He said that
the rebate-guarantee impact would peak in 2019 and ease at the end
of 2020, and that Omnicare's results were expected to stabilize and
improve.
CVS's efforts to bolster its retail offerings, the rollout of a
new PBM contracting model and moves to build its Medicare Advantage
coverage business, among other efforts, will help improve results,
the company said.
CVS also said savings from its Aetna deal are expected to exceed
its previous goal of $750 million in 2020, and should be between
$300 million and $350 million in 2019.
Mr. Merlo said in an interview that 2019 is a transitional year,
and "the work is well under way in terms of the integration of
Aetna," with various pilots being rolled out. He said CVS hopes to
improve pharmacy margins partly by forging contracts that reward it
for taking on a broader role, with services such as helping
patients adhere to their prescriptions and filling gaps in their
care.
CVS swung to a loss for the fourth quarter of 2018, though it
beat analysts' estimates on an adjusted basis. The company reported
a fourth-quarter net loss of $421 million, or 37 cents a share,
down from a profit of $3.29 billion, or $3.22 a share, a year
earlier.
The net results were affected by a $2.2 billion charge related
to the struggling long-term-care business. Adjusted earnings were
$2.14 a share, beating the $2.05 a share analysts polled by
Refinitiv were projecting.
The stock was down 7.9% in afternoon trading Wednesday. Shares
are down 8.9% in the past year.
Mr. Merlo also said in the call that CVS had concerns about the
impact of a new federal proposal that would curb rebates from
drugmakers tied to plans offered under Medicare and Medicaid. He
suggested that the proposal, which could change before it is
finalized and isn't expected to take effect in 2019, might push up
premiums in Medicare's drug-benefit program and damp enrollment by
seniors. He said the proposal could result in a "profit windfall"
for the makers of branded drugs. Mr. Merlo also suggested that
employers and other commercial PBM clients weren't likely to
quickly adopt a model similar to the federal proposal.
Earlier this month, CVS unveiled pilots of a new store format it
called HealthHUB, which focuses more on health and wellness than
its traditional stores by offering health-care services, new
products and services and space for the company and community
groups to offer health-related events.
For the fourth quarter, CVS's revenue rose 12.5% to $54.42
billion, slightly missing the consensus forecast of $54.58 billion
from analysts polled by Refinitiv. Revenue growth was driven by
increased pharmacy network claims, increased prescription volume
and the addition of Aetna, the company said. Same-store sales grew
5.7%, ahead of the FactSet estimate of a 4.6% increase.
After the close of its Aetna deal, CVS created a new
health-care-benefits segment equivalent to the former Aetna
health-care segment, which includes insured and self-insured
medical, pharmacy, dental and behavioral health products and
services. From Nov. 28 to Dec. 31, the health-care-benefits segment
had revenue of $5.55 billion. Its medical membership as of Dec. 31
was 22.1 million, reflecting decreases in commercial insurance and
Medicaid products.
Write to Anna Wilde Mathews at anna.mathews@wsj.com and Aisha
Al-Muslim at aisha.al-muslim@wsj.com
(END) Dow Jones Newswires
February 20, 2019 13:52 ET (18:52 GMT)
Copyright (c) 2019 Dow Jones & Company, Inc.
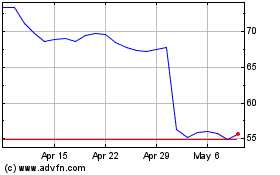
CVS Health (NYSE:CVS)
Historical Stock Chart
From Mar 2024 to Apr 2024
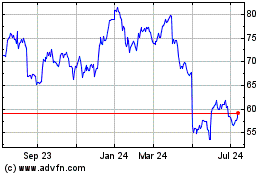
CVS Health (NYSE:CVS)
Historical Stock Chart
From Apr 2023 to Apr 2024