By Anna Wilde Mathews and Joseph Walker
UnitedHealth Group Inc.'s insurance arm will change how it
handles some rebates it gets from drugmakers, passing them on to
individuals who take the medicines amid pressure to reduce costs
and bolster transparency around pharmaceuticals.
The move by the biggest U.S. insurer, which will affect only a
limited slice of customers, spotlights a broader debate over
spending on drugs and the industry's opaque system of discounts and
rebates. The Trump administration has suggested it might make a
similar change in the Medicare program.
At issue are the rebates that drugmakers routinely pay to
insurers and pharmacy-benefit managers on brand-name drugs,
offsetting the full listed prices. The companies use the rebates in
a variety of ways, including lowering their own costs and keeping
premiums down. They also often pass along much of the benefit to
employer clients. But critics, including some drugmakers, say more
of the rebates should go directly to the consumers who take the
drugs.
UnitedHealth said that, starting next year, the plans that its
UnitedHealthcare unit insures for employers will redirect the
"overwhelming majority" of the rebate sums to the individuals
taking the affected drugs. The change, for around 7.5 million
covered people, will reduce costs for individuals by amounts
ranging from a few dollars to more than a thousand dollars per
prescription, UnitedHealth said.
Dan Schumacher, president of UnitedHealthcare, said the company
believes it is the first major insurer to make such a change. "We
see it, for those most directly affected, as an opportunity to
provide greater benefit and lower costs."
But UnitedHealth said the change won't affect the approximately
18.6 million consumers in UnitedHealthcare's "self-insured" plans,
where the employer is the payer. PBMs and insurers, including
UnitedHealth, have previously offered employers the option to pass
along the rebates to individuals. But only around 4% of employers
do it, while 68% use the money more generally to offset their
spending on drugs, according to a survey of employers by the
Pharmacy Benefit Management Institute.
A spokeswoman for Express Scripts Holding Co. said most of its
clients "prefer to use the savings from rebates to keep costs low
for all members" by holding down premiums. CVS Health Corp. said
clients covering around 12 million people, out of the 94 million
whose drug benefits the company manages, pass on the rebates to
individuals taking the drugs.
Nathan Cassin, an assistant vice president at Aon PLC, said
employers "like the flexibility" of being able to use rebate money
as they choose, and PBMs typically charge a fee to pass along
rebates to individuals. "That's a reason not to do it," he
said.
The focus on rebates has grown as brand-name drug prices
skyrocketed in recent years. Insurers and PBMs have demanded
ever-larger rebates in exchange for covering the drugs. Last year,
rebates paid by drugmakers to insurers and PBMs represented an
estimated 23.8% of gross drug costs in Medicare's Part D, the
prescription drug program for seniors and the disabled, up from
9.6% in 2007, according to Medicare's board of trustees.
Currently, people enrolled in high-deductible employer plans can
end up paying the full list-price of their medicine before they
meet their deductible, even though the insurer is getting it at a
discounted cost.
Aetna Inc. said, "The majority of rebates we receive go toward
lowering premiums and fees for members." Cigna Corp. said it
"obtains and shares those discounts with our clients according to
the benefit plan design they have chosen." Anthem Inc. said,
"Rebates are used in helping to make premiums and copays more
affordable."
UnitedHealth said that after its change is implemented,
out-of-pocket payments made before a consumer hits a deductible and
"coinsurance," where a consumer pays a percentage of the drug's
cost, will be calculated using post-rebate prices. Consumers with
flat copayments will pay their typical amounts, unless the
after-rebate cost is lower than their copay. In that case, they
will pay the smaller sum.
Last year, federal officials said they were considering
requiring insurers to use a fixed percentage of their rebates to
reduce Part D patients' out-of-pocket costs on prescriptions.
Several PBMs and insurers -- including UnitedHealth -- oppose the
idea and say it will require them to raise premiums.
UnitedHealth's Mr. Schumacher said Medicare plans have a "very
different benefit structure and funding methodology" than its
employer products. The impact of the rebate change on the premiums
of fully insured employer plans will be "negligible," he said.
Peter Bach, a critic of the pharmaceutical industry's pricing
practices and health policy researcher at Memorial Sloan Kettering
Cancer Center in New York, said that rebates should help
individuals who take the affected drugs, including those in
Medicare -- it's "good for consumers to have lower prices at the
pharmacy counter," he said.
Gerard Anderson, a professor at Johns Hopkins University, said
that passing on rebates to consumers could raise premiums for
everyone, and he warned that drug manufacturers already make
payments to PBMs that aren't labeled as rebates, and those could
increase. "You rename it and it's no longer a rebate," he said.
Write to Anna Wilde Mathews at anna.mathews@wsj.com and Joseph
Walker at joseph.walker@wsj.com
(END) Dow Jones Newswires
March 06, 2018 07:14 ET (12:14 GMT)
Copyright (c) 2018 Dow Jones & Company, Inc.
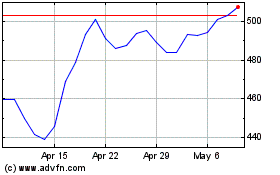
UnitedHealth (NYSE:UNH)
Historical Stock Chart
From Mar 2024 to Apr 2024
UnitedHealth (NYSE:UNH)
Historical Stock Chart
From Apr 2023 to Apr 2024
