By Anna Wilde Mathews
With enrollment for 2018 Affordable Care Act health-insurance
plans starting in just two weeks, insurers are bracing for a
drop-off among consumers put off by higher rates, confusion about
the law's standing and a shorter window to choose coverage.
Companies like Blue Cross Blue Shield of Michigan, Florida Blue
and Medica are rushing to shore up their customer base as the
future of the 2010 health law continues to be debated on Capitol
Hill, where two senators Tuesday announced a tentative deal aimed
at bolstering the ACA marketplaces. The insurers are using
advertising, letters, emails and other outreach techniques to
reassure enrollees about their insurance options under the ACA in
2018.
Other industry players, including online insurance vendor
eHealth Inc., see an opening to offer consumers cheaper
alternatives to ACA policies. While less comprehensive, these plans
could become more appealing if the Trump administration moves
forward with loosening some restrictions on them, as the president
proposed in an executive order last week.
Separately, the Trump administration said it would halt payments
to insurers that are used to reduce health-care costs for
low-income ACA enrollees. Partly because of the anticipated loss of
those federal payments, expected to total $7 billion this year,
major insurers are sharply raising rates in many states.
And many firms say they expect to lose consumers who will bear
the full brunt of the rate increases -- those who aren't eligible
for the health law's premium subsidies, which help enrollees with
annual incomes of less than around $48,000.
"The people we'll lose will likely be the ones who have
affordability issues," said Rick Notter, an executive at Blue Cross
Blue Shield of Michigan. The insurer is raising rates on its ACA
health maintenance organization plans by around 23% on average. It
predicts the state's ACA enrollment will drop by around 9% next
year.
Despite significant rate increases in 2017, enrollment in ACA
plans by subsidized consumers rose an estimated 5.4% in the second
quarter of this year compared with a year earlier, according to
Oliver Wyman, a consulting unit of Marsh & McLennan. But
enrollment in individual coverage by people not receiving subsidies
dropped around 22.4%.
"We will likely see this accelerate in 2018," said Kurt Giesa, a
partner at Oliver Wyman.
Insurers are particularly nervous about losing healthy enrollees
like Daniel Ramos, a 29-year-old massage therapist and personal
trainer in Richmond, Va.
Mr. Ramos, who says he rarely needs health care, was already
skeptical about spending around $250 a month for his current ACA
plan from Anthem Inc. Next year, the only insurer expected to still
sell ACA coverage in Richmond, Cigna Corp., will boost rates 51% on
average across all of its Virginia exchange offerings.
Mr. Ramos, who doesn't get a premium subsidy, says he isn't sure
he will buy an ACA plan again if the options are far more expensive
-- despite the risk of a penalty under the health law's coverage
mandate.
"It feels like a big money hole," he says of the premiums he
pays. "If it becomes more, I'd rather just go ahead and take the
hit and pay the fine next year."
Insurers fear other factors could weigh on 2018 exchange
sign-ups, too. The open enrollment period this year will start on
Nov. 1 in most states and last only about six weeks -- shorter than
in previous years. And the Trump administration has cut back on
advertising and other outreach efforts.
Industry officials also point to confusion over the status of
ACA after months of talk about repealing the law and the
president's comments about Obamacare being "dead" and "finished."
Despite the tentative Senate deal -- which would restore the
federal cost-sharing payments and, potentially, funding for ACA
outreach -- passing legislation before the start of November would
be a heavy lift for Congress.
"It's all of those things together" that will push down
enrollment, along with "the sheer size of the rates," said Chet
Burrell, chief executive of CareFirst BlueCross BlueShield, who
predicts a "decline that will be quite substantial."
CareFirst's ACA rates in Maryland are going up 34.5% for health
maintenance organization plans and 50% for preferred provider
organization plans. The insurer is seeking permission from the
state insurance regulator to make a further boost because of the
halt to federal cost-sharing payments.
A spokesman for the Department of Health and Human Services said
the ACA marketplaces were troubled before the president took
office, and that Mr. Trump's executive order "is intended to
provide Americans with more affordable health-care choices and
allow them to exercise greater control over their health-care
decisions."
Despite the uncertainty, insurers say they're focused on making
sure consumers know when to sign up and understand what's
available. For many people with subsidies, the rate increases will
be largely neutralized because the federal help will rise in tandem
with the cost of plans. Those who don't get subsidies may find that
rate hikes are far sharper on middle-tier "silver" plans, but less
for other types, because of how insurers in some states loaded
their increases.
Insurers will likely be helped by an automatic re-enrollment
process that remains in effect for this year, pushing passive
consumers into new plans.
But that automatic process could mean some consumers will be
signed up for coverage with big rate increases and won't realize it
until they are billed later on.
"We're trying to remind people, 'shop, shop, shop,' " said Geoff
Bartsh, a vice president at Medica, an ACA insurer.
Medica, which is raising rates around 30% or more in states
including Iowa, Nebraska and Wisconsin, is sending letters to
people who will automatically be signed up for its plans. It is
also setting up a special website to help them pick the best
option.
Florida Blue, meanwhile, has created new, lower-cost plans at
the cheapest ACA bronze level to appeal to people who don't get
subsidies, said Jon Urbanek, a senior vice president at the
insurer. The insurer is also sending postcards to prompt people to
shop during open enrollment, and is holding events around the
state. "People are seeing all kinds of confusing messages out
there," Mr. Urbanek said, so the insurer is trying to reassure
them.
For companies that provide cheaper non-ACA products with fewer
benefits, the open enrollment season may offer a chance to snag
more customers.
"We expect a continued acceleration in demand," said Gavin
Southwell, chief executive of Health Insurance Innovations Inc.,
which sells short-term insurance.
Short-term products often are sold only to people who qualify as
healthy, lack certain benefits like maternity care, and don't cover
costs related to pre-existing conditions. Under current
regulations, the plans can't be sold with durations longer than
three months, though that will likely stretch to nearly a year in
many states under changes pushed by Mr. Trump's executive order.
Also, people with short-term plans can still be hit by the ACA's
coverage mandate penalty.
EHealth, the online insurance vendor, is rolling out new
packages that pull together products including short-term
insurance, coverage of online and telephonic doctor visits and
indemnity plans, which generally pay a set sum toward medical
services such as a hospital stay. The bundles provide limited
protection compared with ACA plans. For instance, they lack full
prescription-drug coverage, though they sometimes include discounts
on certain medications. But they are expected to be cheaper than
health-law plans.
The packages are for "those folks who want coverage but are
facing that affordability barrier when they look at the major
medical" plans sold under the ACA, said Paul Rooney, a vice
president at eHealth.
When J. Mitchell Stockdale shopped for ACA plans last year, he
said he found premiums too expensive. So this September, the
53-year-old retired engineering manager in Lenoir City, Tenn.,
decided to buy an eHealth package with an indemnity plan and dental
coverage.
The health plan has limited benefits, including $2,000 a day for
hospital stays, which is less than many hospitals typically bill.
But Mr. Stockdale, who isn't eligible for ACA plan premium
subsidies, says he is betting he won't have major health needs.
"It's a small risk," he said. "I'm willing to take it."
(END) Dow Jones Newswires
October 18, 2017 05:44 ET (09:44 GMT)
Copyright (c) 2017 Dow Jones & Company, Inc.
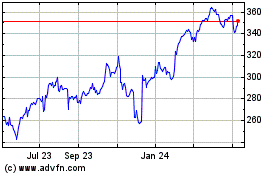
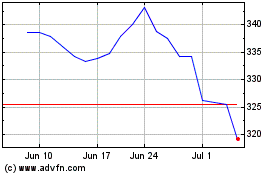
Cigna (NYSE:CI)
Historical Stock Chart
From Mar 2024 to Apr 2024
Cigna (NYSE:CI)
Historical Stock Chart
From Apr 2023 to Apr 2024