By Anna Wilde Mathews and Brent Kendall
Two health-insurance mergers worth a combined $82 billion are
unraveling in the wake of court rulings that found the transactions
violated federal antitrust law, all but quashing a deal boom that
would have reshaped the industry.
Aetna Inc. and Humana Inc. said Tuesday they would terminate
their $34 billion merger agreement instead of attempting to appeal
a judge's decision last month that their combination would harm
senior citizens.
Just hours later, Cigna Corp. said it was calling off its $48
billion merger agreement with Anthem Inc. and pursuing litigation
seeking a $1.85 billion breakup fee plus more than $13 billion in
damages from its deal partner.
Cigna's announcement escalated a monthslong fight in which the
two companies have accused each other of violating their merger
agreement. Anthem immediately disputed Cigna's authority to nix the
deal.
"Anthem will continue to enforce its rights under the merger
agreement and remains committed to closing the transaction," an
Anthem spokeswoman said.
Anthem has said it unilaterally extended the merger agreement
through April 30 and is appealing the antitrust decision, but it
faces numerous obstacles to salvaging the transaction.
The fate of both deals represents a victory for the Obama
administration's antitrust officials, who were able to win the
cases despite major differences between the two transactions.
In the Aetna case, a judge in January said the merger could harm
seniors who buy the private Medicare plans known as Medicare
Advantage. The Anthem antitrust decision by a different judge last
week focused closely on that acquisition's potential impact on
large, multistate employers that offer health coverage to their
workers.
Both acquisitions came together amid an insurance-industry
merger frenzy in 2015, but the dynamics in each have been
different.
Aetna and Humana presented a more united public front. The
companies' tandem announcements of the termination Tuesday said it
was a mutual decision, and both said Aetna will now owe Humana a $1
billion breakup fee.
Aetna Chief Executive Mark T. Bertolini said Tuesday "both
companies need to move forward with their respective strategies in
order to continue to meet member expectations."
Though the decision allows the two insurers to avoid what had
been widely seen as an uphill battle to preserve the deal, it also
leaves them with challenges as they move ahead as stand-alone
companies.
Aetna will now need to find new engines for growth, and it has
highlighted hopes for Medicare, Medicaid and its core commercial
franchise. The Humana deal would have vaulted it to the top
position in the growing Medicare Advantage business.
Humana said Tuesday that the breakup fee is worth about $630
million after taxes. In a call with analysts to discuss its 2017
financial guidance, Humana Chief Executive Bruce Broussard said his
company was "confident in our future."
The company is seen as an attractive takeover target once again,
and Mr. Broussard said Humana was "always oriented toward the most
effective shareholder value, and we would obviously review any kind
of interest into the organization."
Humana, which had retreated somewhat from the Affordable Care
Act's exchanges this year after losses, also said it would fully
withdraw from the business in 2018. Mr. Broussard said the insurer
was "seeing signs of an unbalanced risk pool" in its 2017
enrollment.
That decision is an early difficult sign for the Trump
administration, which, while critical of the Affordable Care Act,
is expected to issue a regulation that includes efforts to
stabilize the law's insurance marketplaces into 2018.
For its part, Anthem faces challenges in its solo effort to
appeal the antitrust ruling. Even if it is able to keep Cigna in
the fold until the end of April, that is almost certainly not
enough time to clear the various legal and regulatory hurdles the
insurer must overcome to complete a deal.
Cigna said in a statement Tuesday that the merger "cannot and
will not achieve regulatory approval" and that "terminating the
agreement is in the best interest of Cigna's shareholders."
The insurer said its lawsuit seeking billions of dollars in
damages from Anthem includes "the amount of premium that Cigna
shareholders did not realize as a result of the failed merger
process." Cigna said it filed the lawsuit in the Delaware Court of
Chancery.
Cigna's move is the latest twist in the increasingly discordant
relationship between the two merger partners, including battles
over strategy, direction and leadership that have become
increasingly public over the past several months.
Analysts have long said litigation between the two appeared
likely in the event of a negative antitrust ruling. During trial
proceedings that began in November, Anthem mounted a legal defense
of the merger single-handedly. Cigna lawyers said very little
during the proceedings, and when they did, it usually didn't help
Anthem's position.
Cigna said Tuesday that Anthem had breached their agreement by
not using its "reasonable best efforts" to win regulatory approval
for the deal.
Anthem declined to comment Tuesday beyond its statement
disputing Cigna's right to break off the merger of the two
insurers.
Write to Anna Wilde Mathews at anna.mathews@wsj.com and Brent
Kendall at brent.kendall@wsj.com
(END) Dow Jones Newswires
February 15, 2017 02:47 ET (07:47 GMT)
Copyright (c) 2017 Dow Jones & Company, Inc.
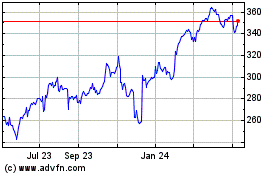
Cigna (NYSE:CI)
Historical Stock Chart
From Mar 2024 to Apr 2024
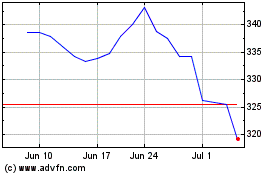
Cigna (NYSE:CI)
Historical Stock Chart
From Apr 2023 to Apr 2024