By Brent Kendall and Anna Wilde Mathews
WASHINGTON -- A federal judge Monday blocked the proposed merger
of health insurers Aetna Inc. and Humana Inc. on antitrust grounds,
a potentially fatal blow to the $34 billion deal and a capstone
victory for Justice Department antitrust officials under former
President Barack Obama.
U.S. District Judge John D. Bates ruled the Justice Department
had proven its case that the merger would unlawfully threaten
competition. harming seniors who buy private Medicare coverage as
well as some consumers who purchase health plans through an
Affordable Care Act insurance exchange.
The government's challenge to the merger was among the last
major law-enforcement actions taken by Obama administration
antitrust officials. The administration also challenged Anthem
Inc.'s proposed acquisition of Cigna Corp ., and a ruling in that
case is expected any day. Together the deals could have transformed
an industry already facing uncertainty from Republican plans to
dismantle the Affordable Care Act and replace it with another
health-care plan.
The ruling by Judge Bates, a George W. Bush appointee, followed
a 13-day trial last month. The Justice Department filed a lawsuit
last year challenging the proposed merge, which Aetna and Humana
announced in July 2015. The two companies said the deal would allow
them to offer more cost-effective products by combining their
strengths and becoming more efficient.
For Judge Bates, the proposed transaction was particularly
problematic for the sale of Medicare Advantage plans, a
government-backed alternative to traditional Medicare that is
offered to seniors by private insurers.
Combining Aetna and Humana likely would lead to a substantial
lessening of competition for these plans in 364 counties, the judge
said. Humana is one of the biggest players in the market and Aetna
in recent years expanded its Medicare Advantage footprint
aggressively, putting it "on a collision course with Humana," Judge
Bates said.
"This head-to-head competition benefits seniors who shop for
Medicare Advantage plans in the form of broader networks and lower
costs," the judge wrote in the opinion.
He rejected the insurers' argument that the merged firm wouldn't
be dominant because government-run Medicare was part of the same
market. That holding sets an important precedent for the
managed-care industry. If the judge had reached the opposite
conclusion, companies likely would have perceived a green light for
more ambitious deal-making.
Judge Bates also said the merger would harm competition on
Affordable Care Act insurance exchanges in parts of Florida.
Aetna last year withdrew from selling plans on most state
exchanges, including in Florida, citing mounting financial losses.
The insurer said its move made the government's argument on this
point moot, but Judge Bates disagreed, saying Aetna withdrew from
certain locations "specifically to evade judicial scrutiny of the
merger."
A Humana spokesman said "Aetna and Humana are reviewing the
decision." Aetna signaled it may not be ready to give up its fight
for the deal. "We're reviewing the opinion now and giving serious
consideration to an appeal after putting forward a compelling
case," Aetna spokesman T.J. Crawford said.
Merging parties don't often appeal adverse court rulings because
of the time, money and uncertainty involved in trying to keep a
deal together during prolonged litigation.
Aetna potentially could seek to start new discussions with
incoming Trump administration antitrust enforcers about a way to
salvage the deal, but it could be weeks or months before a new
Justice Department antitrust team is fully in place. Even if such
talks did unfold, Aetna and Humana are now facing a court ruling
that says unequivocally the deal violates federal antitrust
law.
In trading Monday, shares of Humana rose 2.2%, and shares of
Aetna fell 2.7%.
The companies' merger agreement is set to expire Feb. 15, after
which either insurer could walk away from the deal.
The Justice Department said the court's decision would save
customers and taxpayers up to $500 million a year. "Aetna attempted
to buy a formidable rival, Humana, instead of competing
independently to win customers," said Deputy Assistant Attorney
General Brent Snyder, a career official temporarily heading the
antitrust division.
Humana is the second-largest Medicare insurer, with around 3.3
million beneficiaries, or about 16.9% of the Medicare Advantage
market, according to Credit Suisse. Aetna is fourth, with about 1.4
million beneficiaries and 7.2% of the Medicare Advantage market.
Combined, they would surpass the enrollment of Medicare Advantage
leader UnitedHealth Group Inc.
The government's antitrust concerns focused more on particular
geographies, not national market share, because Medicare Advantage
plans are sold on a local basis. Aetna and Humana had argued they
could alleviate the concerns by divesting -- or selling off --
assets representing about 290,000 enrollees in 21 states to Molina
Healthcare Inc., a managed care company focused primarily on
Medicaid.
Judge Bates ruled, however, that the proposed divestiture "would
not ameliorate the anticompetitive effects of the merger."
Molina said it was disappointed in the ruling but remained
committed to growing its Medicare business.
After Monday's ruling, Aetna and Humana now face the prospect of
going it alone, without the added cost-squeezing scale and clout
they had hoped to gain in their combination.
Without the deal, Humana maintains a narrow focus on Medicare
Advantage, a rapidly growing business but one that can be
operationally difficult. The changeover to Republican control in
Washington is generally seen as a positive for private Medicare
plans. Humana has already pulled back from its ACA marketplace
business, which had run losses, and thus reduced its risk from
upheaval if the health law is repealed.
Humana is also poised to emerge with a $1 billion breakup fee
from Aetna if the deal doesn't close. The company has previously
said money from the breakup fee would be allocated according to its
earlier capital plans, which include possible spending on
acquisitions, share buybacks and dividends.
If the deal dies, Aetna Chief Executive Mark T. Bertolini would
lose the chance to rapidly build a diversified insurance powerhouse
with government business balanced against traditional commercial
coverage. Aetna remains far smaller than UnitedHealth and Humana in
the important Medicare market. It will have to find other engines
for growth, either organically or through smaller-scale deals.
Aetna has already sharply scaled back its position in the ACA
marketplaces this year after deepening losses. Its footprint has
fallen to four states, down from 15 in 2016.
Hospitals and doctors have watched insurance industry
consolidation warily, amid concern that larger insurance firms
would push to impose lower reimbursement rates on health-care
providers. Both the American Medical Association and American
Hospital Association cheered the judge's ruling.
Write to Brent Kendall at brent.kendall@wsj.com and Anna Wilde
Mathews at anna.mathews@wsj.com
(END) Dow Jones Newswires
January 24, 2017 02:47 ET (07:47 GMT)
Copyright (c) 2017 Dow Jones & Company, Inc.
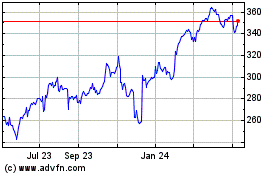
Cigna (NYSE:CI)
Historical Stock Chart
From Mar 2024 to Apr 2024
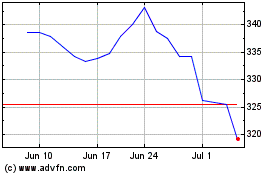
Cigna (NYSE:CI)
Historical Stock Chart
From Apr 2023 to Apr 2024